Abstract
Background
Dent disease is a rare tubulopathy characterized by manifestations of proximal tubular dysfunction, which occurs almost exclusively in males. It mainly presents symptoms in early childhood and may progress to end-stage renal failure between the 3rd and 5th decades of human life. According to its various genetic basis and to clinical signs and symptoms, researchers define two forms of Dent disease (Dent diseases 1 and 2) and suggest that these forms are produced by mutations in the CLCN5 and OCRL genes, respectively. Dent diseases 1 and 2 account for 60% and 15% of all Dent disease cases, and their genetic cause is generally understood. However, the genetic cause of the remaining 25% of Dent disease cases remains unidentified.
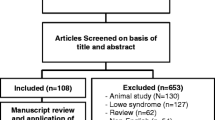
Data sources
All relevant peer-reviewed original articles published thus far have been screened out from PubMed and have been referenced.
Results
Genetic testing has been used greatly to identify mutation types of CLCN5 and OCRL gene, and next-generation sequencing also has been used to identify an increasing number of unknown genotypes. Gene therapy may bring new hope to the treatment of Dent disease. The abuse of hormones and immunosuppressive agents for the treatment of Dent disease should be avoided to prevent unnecessary harm to children.
Conclusions
The current research progress in classification, genetic heterogeneity, diagnosis, and treatment of Dent disease reviewed in this paper enables doctors and researchers to better understand Dent disease and provides a basis for improved prevention and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dent disease is a kind of familial kidney disorder with an X-linked recessive pattern that may cause end-stage renal disease (ESRD). It was found and described by Dent and Friedman for the first time as early as 1964 after they reported two unrelated male individuals with renal rickets due to renal tubular damage. The damage had characteristics of hypercalciuria, hypophosphatemia, low-molecular-weight proteinuria (LMWP), and aminoaciduria [1, 2]. At that time, these symptoms were not formally named but were just described as hypercalciuric rickets. Thirty years later, Wrong et al. [3] carried out additional clinical work and described the disease as a form of hereditary renal “Fanconi Syndrome” that had characteristics of hypercalciuria, LMWP, nephrocalcinosis, slowly progressive renal failure, and a marked male predominance. Wrong et al. [3] termed the condition as Dent disease and suggested that it should be inherited in an X-linked pattern. Subsequently, with the application of molecular genetic analysis, Dent disease was finally confirmed as a rare X-linked recessive renal tubular disorder caused by pathogenic gene variants. Genetic analysis also revealed that Dent disease has characteristics of LMWP, hypercalciuria, and at least one of the following characteristics: nephrocalcinosis, nephrolithiasis, hematuria, hypophosphatemia and chronic kidney disease (CKD) [2, 4].
Typical symptoms of Dent disease are generally found in boys under 10 years old [5, 6]. Between the ages of 30 and 50, 30–80% of patients with Dent disease can develop ESRD [5, 7, 8]. One of the typical histological features observed on Dent disease renal biopsies is reported as being focal global glomerulosclerosis, which can easily be interpreted as focal segmental glomerulosclerosis [9,10,11]. Mutations in the CLCN5 (chloride voltage-gated channel 5) or OCRL gene (inositol polyphosphate-5-phosphatase) are reported to cause Dent disease. For example, approximately 200 mutations in the CLCN5 gene and more than 140 mutations in the OCRL gene have been reported [12, 13]. In males, one altered copy of a gene in each cell is sufficient to cause the signs and symptoms of the disorder, whereas females with one mutated copy of the gene can be carriers that pass on the altered gene and cause milder signs and symptoms of the disorder (mainly hypercalciuria and microscopic hematuria, and rarely ESRD or CKD) [14].
With the rapid development of next-generation sequencing technology in recent years, more diverse mutation types of CLCN5 gene and OCRL gene as well as unknown genotypes in patients with Dent disease can be identified by performing genome sequencing. These newly discovered genotypes have allowed researchers to make significant progress in the early diagnosis of Dent patients. Therefore, this paper attempts to provide a thorough review of the latest research progress regarding Dent disease’s classification, genetic mutation, diagnosis, and treatment.
Clinical classification
There are two forms of Dent disease that are generally defined by researchers according to a mutated gene on the X-chromosome; they are Dent disease 1 and Dent disease 2. Patients with mutations in the CLCN5 gene are categorized as patients with Dent disease 1, which accounts for about 60% of all cases of Dent disease. Patients with mutations in the OCRL gene are defined as patients with Dent disease 2, which accounts for about 15% of all cases of Dent disease. The genetic origin of the remaining cases (25% of all cases) is still unclear [1, 6].
Dent disease 1 and Dent disease 2 are partially similar in clinical and biological phenotypes. The main clinical manifestations of Dent disease 1 patients include LMWP, hypercalciuria, renal calcification, and nephrolithiasis, and renal tubular dysfunction. Some patients may even have progressive renal failure and rickets-related symptoms [15]. By comparison, patients with Dent disease 2 are likely to have milder extrarenal characteristics than those with Lowe syndrome. Their symptoms generally include muscle weakness, ocular abnormalities, and milder mental retardation [16, 17]. Also, recent observations have shown that Dent disease 2 presents with typical cutaneous features, namely hidradenitis suppurativa, previously never reported [18, 19].
Dent disease 1 and CLCN5 mutations
Dent disease 1 is caused by inactivating mutations in the CLCN5 gene located on the short arm of the X-chromosome (Xp11.22) [1]. The CLCN5 gene encodes a 746 amino-acid CLC-5 protein, a highly conserved electrogenic 2Cl−/H+ antiporter [20], which contains 18 α-helices, with two phosphorylation and one N-glycosylation site. CLC-5 protein consists of a homodimer that spans the cell membrane in the opposite direction. Each subunit has its own pore responsible for the selective transport of chloride and hydrogen ions [21]. CLC-5 is mainly expressed in the proximal tubule and intercalated cells of the collecting duct in the kidney, and it is predominantly located in early endosomes, colocalizing with V-ATPase [22].
Generally, glucose, albumin, transferrin, ions, vitamin D, amino acids, insulin, growth hormone, and parathyroid hormone filtered by the glomerulus are effectively reabsorbed in the proximal tubule. The reabsorption process is essentially mediated by megalin/cubilin and is accomplished via endocytosis. With the help of H+-ATPase, endosomes are gradually acidified, resulting in dissociation of the receptor ligand complex and subsequent degradation of the ligand in the lysosome [23]. Researchers have demonstrated that CLC-5 plays a crucial role in endosome acidification, and it is a direct drive of protons into proximal tubular cells, thus contributing to endocytic pathways. In the absence of functional CLC-5, the endocytosis of proximal renal tubular epithelial cells is inhibited, and the biological function of reabsorbing carbohydrates, amino acids, and hormones cannot be exerted, resulting in LMWP. Besides, defects in endocytosis of proximal tubular epithelial cells lead to the reabsorption of parathyroid hormone (PTH) in the proximal tubules, causing an increase in the concentration of PTH in the urine and thus the high level of 1,25-(OH)2-vitamin D3 [1, 24]. Thereby, intestinal absorption of calcium is promoted, leading to clinical symptoms of hypercalciuria and renal calcification [1, 25]. When expression of the megalin receptor on the apical membrane of the proximal tubule is deficient, inflammation and apoptotic pathways in renal epithelial cells can be triggered [26].
Dent disease and hereditary hypophosphatemic rickets are both related to the changes of CLCN5 gene. More than 200 different mutations of CLCN5 gene have been identified thus far, mainly including nonsense variants (p.R637X, p.Y143X), missense variants (p.A540D, p.G135E, p.G703V), deletion variants (exons 9, 10, 11, 12, 13, 1 missing), and a frameshift variant (p.T260Tfs*10) [24, 25]. The mutation sites of CLCN5 gene have the unfixed and diverse characteristics; their connection with clinical symptoms is still unclear. Mansour-Hendili et al. [12] reviewed 234 kinds of CLCN5 gene mutations reported from January 2001 to December 2014. By descriptive analysis, they revealed that there are 33.33% of missense, 29.05% of frameshift, 17.52% of nonsense and other mutation types. Among them, nine nonsense (p.R28X, p.R34X, p.W279X, p.R347X, p.R467X, p.R637X, p.R648X, p.R704X and p.R718X) and three missense (p.S244L, p.R516W and p.S545N) mutations have been detected in patients from different geographic origins and thus can be considered as mutation hotspots.
Except for mutations in exons, researchers have found that intronic mutations of CLCN5 gene play an essential role in causing Dent disease that may have been ignored in previous studies. Matsumoto et al. [27] described a 40-year-old Japanese male with Dent disease caused by a novel intronic mutation (1348-1G > A) on the splicing site of CLCN5 gene that had not been included in any genetic databases before. Two other intronic mutations (IVS3 + 2G > C and IVS3 − 1G > A) also were discovered by Tosetto et al. [28]. Researchers concluded that different types of mutants can be broadly classified into three categories [29, 30]. The first type of mutant is characterized by the inability to induce 2Cl−/H+ reverse current. The second type of mutant is characterized by the inability to perform protein processing and maturation stably. The last type is characterized by insufficient bioelectrical activity. Although the mutations in the CLCN5 gene observed in patients with Dent disease have been summarized by Grand et al. [31], the relationship between mutation types (missense, nonsense, deletion, or frameshift) and prediction results of disease or prognosis is unknown.
Dent disease 2 and OCRL mutations
Dent disease 2 is caused by the mutation of OCRL, which is located on the long arm of the X-chromosome (Xq26.1) and contains 24 exons. The OCRL gene mutation was first identified by Attree et al. [32]; it causes Lowe syndrome, an X-linked recessive disorder that is characterized by congenital cataracts, intellectual disability and renal syndrome. Mutations in OCRL also were found to underlie Dent disease 2 by Hoopes et al. [33]. Research has shown that pathogenic mutations can occur in all regions of the OCRL gene. The mutation sites that are distributed in exons 1–15 region of the OCRL gene, while Lowe syndrome is mainly distributed in exons 8–23 [1, 13, 34]. To date, more than 140 mutation sites in the OCRL gene that cause Dent disease 2 have been reported, including insertions, deletions, splicing, and missense mutations [13]. Dent disease 2 associated missense mutations are distributed in exons 4–15, mainly in exons 9–15 [1, 13, 34], whereas the other mutations (nonsense, frameshift and splicing) are found within the first seven exons and exons 22–24 [16, 34, 35].
It encodes the inositol polyphosphate 5-phosphatase (OCRL1) [32] that hydrolyzes phosphatidyl-inositol 4,5-bisphosphate (PIP2) to regulate membrane transport and cytoskeletal structure and function [24]. Universally expressed in almost all tissues, the protein structural domain mainly includes a 5-phosphatase catalytic domain, a Rho-GAP-like domain, an N-terminal domain, and a C-terminal lipid-binding domain [24, 36, 37]. Previously, it was thought that the mutation sites affecting Dent disease 2 were mainly located in PH domain [34]. However, Ye et al. found that the 5-phosphatase catalytic domain and Rho-GAP-like domain coding region of OCRL are important functional domains in Dent disease 2 [13]. In the nephron, it is mainly located in the glomerulus, proximal tubules and collecting ducts [38].
The OCRL1 protein is originally concentrated in a complex trans-Golgi network that classifies proteins and other molecules and delivers them to intended destinations inside and outside the cells. It also exists in the endosomes and specialized compartments formed on the cell surface to transport proteins and small molecules to the specified destinations within the cell. The lack in OCRL1 leads to impaired endocytosis of zebrafish, indicating that tubular endocytosis requires catalytic activity of OCRL1, which is needed for endocytic transport in vivo [39]. Regarding the detailed molecular mechanisms, some researchers maintained that shrunk OCRL1 activity could lead to accumulation of PIP2 and thus change cellular phosphatidylinositol 4-phosphate 5-kinase signaling pathway associated with endocytosis [39, 40].
OCRL mutations also may cause Dent disease or Lowe syndrome and thus have an influence on the kidney [41]. Some researchers consider Dent disease 2 as a mild Lowe syndrome [42]; however, the renal manifestations of Lowe syndrome are different from the Dent disease with tubular dysfunction. Lowe syndrome can present with symptoms of renal glycosuria, aminoaciduria, and phosphate urinary tract. These symptoms are rare in Dent disease. As the OCRL gene is actively expressed throughout the body, the reason why Dent disease 2 primarily affects the kidney and, to a lesser extent, the brain, eyes, and other tissues remains unclear.
Heterogeneity of Dent disease
Approximately 25% of patients with Dent disease do not carry the CLCN5 or OCRL mutations, indicating the presence of other unrecognized genetic factors. Patients with Dent disease are generally believed to have a single gene mutation either in the CLCN5 gene or in the OCRL gene; very few patients have been reported to carry both OCRL and CLCN5 disease-causing mutations and thereby realize the additive effect of Dent disease [43]. Using the next-generation sequencing to analyze the whole exome of nine patients in Children’s Hospital of Fudan University, Zhang et al. [30] identified possible modifier genes CFTR, SCNN1A, and SCNN1B associated with cystic fibrosis (CF) or CF-like diseases that could contribute to Dent disease pathology. However, the exact disease-causing mutation of these genes has not yet been identified [30]. Glomerular pathology, specifically involving the podocyte, may promote the progression of Dent disease [15]. A better screening tool is thus needed as a possible diagnosis tool, and the awareness of identifying novel mutations related to Dent disease also should be raised.
Diagnosis
Early diagnosis is the key to treatment of Dent disease as it can prevent drug abuse, as well as occurrence and development of renal failure by conducting possible effective interventions. However, Dent disease is often diagnosed at an advanced stage or is sometimes undiagnosed. The clinical manifestations of Dent disease are diverse. In addition, the lack of typical serological changes and insufficient recognition by pediatricians make it extremely difficult to diagnose Dent disease early in routine clinic work. The occurrence of proteinuria in children is first regarded as caused by glomerular lesions, which leads to misdiagnosis as nephrotic syndrome. Consequently, corticosteroids and immunosuppressive therapies are incorrectly used for treatment; thus, Dent disease can easily be ignored. For example, Li et al. [44] reported that 16 of 19 patients with Dent disease had been misdiagnosed, and 11 of 19 had received incorrect or unnecessary treatment.
Currently, the diagnostic methods of Dent disease mainly include two aspects: targeting symptoms and targeting gene mutations. A typical phenotype characterized by LMWP, hypercalciuria, and progressive renal failure in various combinations often makes clinical diagnosis easier and more precise [28]. Dent disease should be considered in patients if they are characterized by proteinuria and/or focal glomerulosclerosis, particularly in male patients without edema or hypoalbuminemia and also in male patients with a family history of renal disease on the maternal side [1, 45]. Hypercalciuria is not a typical symptom used for the diagnosis of Dent disease, whereas LMWP is a common symptom presented in all patients. For example, Sekine et al. [8] concluded that the incidence of hypercalciuria in 86 cases of Japanese Dent disease was only 51%. Children with renal Fanconi syndrome also have clinical features such as proximal tubule dysfunction, which is similar to patients with Dent disease.
The following cases are more likely to be diagnosed as Dent disease: (1) the patient has proximal renal tubular dysfunction without symptoms of acidosis; (2) male patients have no edema or low protein blood symptoms, but have a family history of renal disease in male patients on the maternal side [1, 33, 46]. Verified by experimental data, urine protein electrophoresis provides a more rapid and accurate method of screening for LMWP to find tubular disease [47,48,49]. Albumin/total protein ≤ 0.21 and α1-microglobulin/creatinine of ≥ 120 mg/g have been put forward as criteria for screening Dent disease [11]; however, this laboratory diagnostic technology has not been used routinely in clinical work. The sub-clinical physical condition also may go under-diagnosed, limiting early diagnosis of Dent disease. Genetic testing is recommended to confirm the diagnosis on clinically suspected patients and their female family members. Genetic testing, especially next-generation sequencing, has not been applied well in clinical diagnosis due to its high cost and lack of awareness, despite its ability to provide accurate diagnosis [44]. At present, the most commonly used procedure for gene sequencing of suspected cases is to extract the peripheral blood genomic DNA of the patients, to amplify all coding sequences of CLCN5 gene and OCRL gene, and to sequence and analyze the PCR products. This procedure is useful in the diagnosis of Dent disease, but it is rather time-consuming. A better screening tool is therefore needed as a possible diagnosis tool. The awareness of identifying novel mutations related to Dent disease also should be raised. Researchers suggest that when a patient develops proteinuria, a protein test on the hepatic tubule can be used to distinguish between renal tubular proteinuria and glomerular proteinuria. Further genetic testing can then be performed in the laboratory to determine whether the CLCN5 and/or OCRL genes are mutated. Raising clinicians’ awareness of Dent disease is also important.
Treatment
Dent disease is a congenital genetic disease, and it is still incurable. Only symptomatic support can be taken, including reduction of hypercalciuria, prevention of nephrocalcinosis and kidney stones, and retardation of the evolution of chronic kidney disease. For treatment of Dent disease, current interventions are designed firstly to drink plenty of water, so as to avoid high calcium, high sodium and high oxalate diets, as well as to control high calcium urine and to prevent kidney calcification and its complications. The main clinical measurements for hypercalciuria are low-calcium diet and hydrochlorothiazide intake to promote calcium reabsorption at the distal end of the tubule and to delay the progression of the disease. However, it should be noted that a low-calcium diet and a low vitamin D intake may affect bone health and may increase the risk of kidney stone formation [50, 51]. Many publications have reported that the potassium citrate diet, the drug combination treatment of amiloride, hydrochlorothiazide and potassium citrate, and the angiotensin-converting enzyme inhibitor drug significantly reduce urinary calcium and protect kidney function [51,52,53].
Gabriel et al. [54] found that the bone marrow transplantation can improve proximal tubular dysfunction of Dent disease in virtue of Clcn5Y/- mice, which is a faithful model for Dent disease. GH therapy can increase height velocity and serum insulin-like growth factor 1 levels, especially delay the improvement of phosphaturia in Dent disease patients [55]. Unfortunately, research objects in these studies were limited, and control defects were insufficient. To produce a good treatment plan, more clinical trials are needed to provide a theoretical basis for treatment.
Conclusions
Dent disease is an X-linked recessive inherited tubular disease and has clinical features of LMWP, hypercalciuria, and renal calcification. Some patients with Dent disease may have renal dysfunction or renal failure. Dent disease is mainly caused by mutations of CLCN5 gene, and a small proportion of Dent disease cases is caused by mutations of OCRL gene.
In the past few decades, great progress has been made in understanding Dent disease. With the deepening of molecular genetic research in Dent disease, the discovery of more pathogenic genes has promoted a more thorough understanding of the pathogenesis of Dent disease. Gene therapy may bring new hope to the treatment of Dent disease. Further research is needed to exploit disease heterogeneity and to develop early diagnosis technologies. The abuse of hormones and immunosuppressive agents, which may cause unnecessary harm to children, should be avoided in the treatment of Dent disease. Moreover, attention should be paid to the identification of type 1 and type 2 Dent disease and to other complications.
References
Ehlayel AM, Copelovitch L. Update on Dent disease. Pediatr Clin N Am. 2019;66:169–78.
Dent CE, Friedman M. Hypercalciuric rickets associated with renal tubular damage. Arch Dis Child. 1964;39:240–9.
Wrong OM, Norden AG, Feest TG. Dent's disease; a familial proximal renal tubular syndrome with low-molecular-weight proteinuria, hypercalciuria, nephrocalcinosis, metabolic bone disease, progressive renal failure and a marked male predominance. QJM. 1994;87:473–93.
Bignon Y, Alekvo A, Frachon N, Lahuna O, Jean-Baptiste Doh-Egueli C, Deschênes G, et al. A novel CLCN5 pathogenic mutation supports Dent disease with normal endosomal acidification. Hum Mutat. 2018;39:1139–49.
Devuyst O, Thakker RV. Dent's disease. Orphanet J Rare Dis. 2010;5:28.
Blanchard A, Curis E, Guyon-Roger T, Kahila D, Treard C, Baudouin V, et al. Observations of a large Dent disease cohort. Kidney Int. 2016;90:430–9.
Claverie-Martin F, Ramos-Trujillo E, Garcia-Nieto V. Dent's disease: clinical features and molecular basis. Pediatr Nephrol. 2011;26:693–704.
Sekine T, Komoda F, Miura K, Takita J, Shimadzu M, Matsuyama T, et al. Japanese Dent disease has a wider clinical spectrum than Dent disease in Europe/USA: genetic and clinical studies of 86 unrelated patients with low-molecular-weight proteinuria. Nephrol Dial Transpl. 2014;29:376–84.
Solanki AK, Arif E, Morinelli T, Wilson RC, Hardiman G, Deng P, et al. A novel CLCN5 mutation associated with focal segmental glomerulosclerosis and podocyte injury. Kidney Int Rep. 2018;3:1443–53.
Fervenza FC. A patient with nephrotic-range proteinuria and focal global glomerulosclerosis. Clin J Am Soc Nephrol. 2013;8:1979–87.
Beara-Lasic L, Cogal A, Mara K, Enders F, Mehta RA, Haskic Z, et al. Prevalence of low molecular weight proteinuria and Dent disease 1 CLCN5 mutations in proteinuric cohorts. Pediatr Nephrol. 2019. https://doi.org/10.1007/s00467-019-04210-0.
Mansour-Hendili L, Blanchard A, Le Pottier N, Roncelin I, Lourdel S, Treard C, et al. Mutation update of the CLCN5 gene responsible for Dent disease 1. Hum Mutat. 2015;36:743–52.
Ye Q, Shen Q, Rao J, Zhang A, Zheng B, Liu X, et al. Multicenter study of the clinical features and mutation gene spectrum of Chinese children with Dent disease. Clin Genet. 2020;97:407–17.
Zhang H, Wang C, Yue H, Hu WW, Gu JM, He JM, et al. Identification of a novel mutation in the CLCN5 gene in a Chinese family with Dent-1 disease. Nephrology (Carlton). 2014;19:80–3.
Wang X, Anglani F, Beara-Lasic L, Mehta AJ, Vaughan LE, Herrera HL. Glomerular pathology in Dent disease and its association with kidney function. Clin J Am Soc Nephrol. 2016;11:2168–76.
Zaniew M, Bökenkamp A, Kołbuc M, La Scola C, Baronio F, Niemirska A, et al. Long-term renal outcome in children with OCRL mutations: retrospective analysis of a large international cohort. Nephrol Dial Transpl. 2018;33:85–94.
Bökenkamp A, Böckenhauer D, Cheong HI, Hoppe B, Tasic V, Unwin R, et al. Dent-2 disease: a mild variant of Lowe syndrome. J Pediatr. 2009;155:94–9.
Marzuillo P, Caiazzo R, Coppola C, Camponesco O, Miraglia Del Giudice E, Argenziano G, et al. Polyclonal gammopathy in an adolescent affected by Dent disease 2 and hidradenitis suppurativa. Int J Dermatol. 2020. https://doi.org/10.1111/ijd.14789.
Marzuillo P, Piccolo V, Mascolo M, Apicella A, Argenziano G, Della Vecchia N, et al. Patients affected by dent disease 2 could be predisposed to hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2018;32:e309–11.
Picollo A, Pusch M. Chloride/proton antiporter activity of mammalian CLC proteins ClC-4 and ClC-5. Nature. 2005;436:420–3.
Dutzler R, Campbell EB, Cadene M, Chait BT, Mackinnon R. X-ray structure of a ClC chloride channel at 3.0 Å reveals the molecular basis of anion selectivity. Nature. 2002;415:287–94.
Novarino G, Weinert S, Rickheit G, Jentsch TJ. Endosomal chloride-proton exchange rather than chloride conductance is crucial for renal endocytosis. Science. 2010;328:1398–401.
Günther W, Lüchow A, Cluzeaud F, Vandewalle A, Jentsch TJ. ClC-5, the chloride channel mutated in Dent's disease, colocalizes with the proton pump in endocytotically active kidney cells. Proc Natl Acad Sci USA. 1998;95:8075–88.
Claverie-Martín F, Ramos-Trujillo E, García-Nieto V. Dent's disease: clinical features and molecular basis. Pediatr Nephrol. 2011;26:693–704.
Günther W, Piwon N, Jentsch TJ. The ClC-5 chloride channel knock-out mouse—an animal model for Dent's disease. Pflugers Arch. 2003;445:456–62.
Wellhauser L, D'Antonio C, Bear CE. ClC transporters: discoveries and challenges in defining the mechanisms underlying function and regulation of ClC-5. Pflugers Arch. 2010;460:543–57.
Matsumoto A, Matsui I, Mori T, Sakaguchi Y, Mizui M, Ueda Y, et al. A case of severe osteomalacia with Dent disease caused by a novel intronic mutation of the CLCN5 gene. Internal Med. 2018;57:3603–10.
Tosetto E, Ghiggeri GM, Emma F, Barbano G, Carrea A, Vezzoli G, et al. Phenotypic and genetic heterogeneity in Dent's disease—the results of an Italian collaborative study. Nephrol Dial Transpl. 2006;21:2452–63.
Lourdel S, Grand T, Burgos J, González W, Sepúlveda FV, Teulon J. ClC-5 mutations associated with Dent's disease: a major role of the dimer interface. Pflugers Arch. 2012;463:247–56.
Zhang Y, Fang XY, Xu H, Shen Q. Genetic analysis of Dent's disease and functional research of CLCN5 mutations. DNA Cell Biol. 2017;36:1151–8.
Grand T, L'Hoste S, Mordasini D, Defontaine N, Keck M, Pennaforte T, et al. Heterogeneity in the processing of CLCN5 mutants related to Dent disease. Hum Mutat. 2011;32:476–83.
Attree O, Olivos IM, Okabe I, Bailey LC, Nelson DL, Lewis RA, et al. The Lowe's oculocerebrorenal syndrome gene encodes a protein highly homologous to inositol polyphosphate-5-phosphatase. Nature. 1992;358:239–42.
Hoopes RR Jr, Shrimpton AE, Knohl SJ, Hueber P, Hoppe B, Matyus J, et al. Dent disease with mutations in OCRL1. Am J Hum Genet. 2005;76:260–7.
De Matteis MA, Staiano L, Emma F, Devuyst O. The 5-phosphatase OCRL in Lowe syndrome and Dent disease 2. Nat Rev Nephrol. 2017;13:455–70.
Staiano L, De Leo MG, Persico M, De Matteis MA. Mendelian disorders of PI metabolizing enzymes. Biochim Biophys Acta. 2015;1851:867–81.
Song E, Luo N, Alvarado JA, Lim M, Walnuss C, Neely D, et al. Ocular pathology of oculocerebrorenal syndrome of Lowe: novel mutations and genotype–phenotype analysis. Sci Rep. 2017;7:1442.
Stenson PD, Ball EV, Mort M, Phillips AD, Shiel JA, Thomas NS, et al. Human Gene Mutation Database (HGMD): 2003 update. Hum Mutat. 2003;21:577–81.
Erb BC, Velázquez H, Gisser M, Shugrue CA, Reilly RF. cDNA cloning and localization of OCRL-1 in rabbit kidney. Am J Physiol. 1997;273:F790–5.
Oltrabella F, Pietka G, Ramirez IB, Mironov A, Starborg T, Drummond IA, et al. The Lowe syndrome protein OCRL1 is required for endocytosis in the zebrafish pronephric tubule. PLoS Genet. 2015;11:e1005058.
Mehta ZB, Pietka G, Lowe M. The cellular and physiological functions of the Lowe syndrome protein OCRL1. Traffic. 2014;15:471–87.
Lowe CU, Terrey M, Maclachlan EA. Organic-aciduria, decreased renal ammonia production, hydrophthalmos, and mental retardation; a clinical entity. AMA Am J Dis Child. 1952;83:164–84.
Festa BP, Berquez M, Gassama A, Amrein I, Ismail HM, Samardzija M, et al. OCRL deficiency impairs endolysosomal function in a humanized mouse model for Lowe syndrome and Dent disease. Hum Mol Genet. 2019;28:1931–46.
Addis M, Meloni C, Tosetto E, Ceol M, Cristofaro R, Melis MA, et al. An atypical Dent's disease phenotype caused by co-inheritance of mutations at CLCN5 and OCRL genes. Eur J Hum Genet. 2013;21:687–90.
Li F, Yue Z, Xu T, Chen M, Zhong L, Liu T, et al. Dent disease in Chinese children and findings from heterozygous mothers: phenotypic heterogeneity, fetal growth, and 10 novel mutations. J Pediatr. 2016;174:204–10.e1.
Frishberg Y, Dinour D, Belostotsky R, Becker-Cohen R, Rinat C, Feinstein S, et al. Dent's disease manifesting as focal glomerulosclerosis: is it the tip of the iceberg? Pediatr Nephrol. 2009;24:2369–73.
Bogdanović R, Draaken M, Toromanović A, Dordević M, Stajić N, Ludwig M. A novel CLCN5 mutation in a boy with Bartter-like syndrome and partial growth hormone deficiency. Pediatr Nephrol. 2010;25:2363–8.
Zhang H, Wang F, Xiao H, Yao Y. The ratio of urinary α1-microglobulin to microalbumin can be used as a diagnostic criterion for tubuloproteinuria. Intractable Rare Dis Res. 2018;7:46–50.
He G, Zhang H, Wang F, Liu X, Xiao H, Yao Y. Diagnosis and treatment of Dent disease in 10 Chinese boys. Intractable Rare Dis Res. 2017;6:41–5.
Levinson SS. Urine protein electrophoresis and immunofixation electrophoresis supplement one another in characterizing proteinuria. Ann Clin Lab Sci. 2000;30:79–84.
Raja KA, Schurman S, D'Mello RG, Blowey D, Goodyer P, Van Why C, et al. Responsiveness of hypercalciuria to thiazide in Dent's disease. J Am Soc Nephrol. 2002;13:2938–44.
Cebotaru V, Kaul S, Devuyst O, Cai H, Racusen L, Guggino WB, et al. High citrate diet delays progression of renal insufficiency in the ClC-5 knockout mouse model of Dent's disease. Kidney Int. 2005;68:642–52.
Vaisbich MH, Henriques Ldos S, Igarashi T, Sekine T, Seki G, Koch VH. The long-term use of enalapril and hydrochlorothiazide in two novel mutations patients with Dent's disease type 1. J Bras Nefrol. 2012;34:78–81.
Vrljicak K, Batinić D, Milosević D, Nizić-Stancin L, Ludwig M. A boy with Dent-2 disease. Coll Antropol. 2011;35:925–8.
Gabriel SS, Belge H, Gassama A, Debaix H, Luciani A, Fehr T, et al. Bone marrow transplantation improves proximal tubule dysfunction in a mouse model of Dent disease. Kidney Int. 2017;91:842–55.
Sheffer-Babila S, Chandra M, Speiser PW. Growth hormone improves growth rate and preserves renal function in Dent disease. J Pediatr Endocrinol Metab. 2008;21:279–86.
Funding
The study was supported by National Natural Foundation of China (81470939 & 81770710), Natural Science Foundation of Zhejiang Province (LH14H050002, LY15H050001, LQ18H050001), and Ai You Foundation.
Author information
Authors and Affiliations
Contributions
JYY wrote the initial draft. HLM revised the manuscript. QXF and MJH reviewed and revised the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Ethical approval
Not needed.
Conflict of interest
All authors disclosed no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jin, YY., Huang, LM., Quan, XF. et al. Dent disease: classification, heterogeneity and diagnosis. World J Pediatr 17, 52–57 (2021). https://doi.org/10.1007/s12519-020-00357-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-020-00357-1