Abstract
Background
To systematically evaluate the incidence characteristics of testicular microlithiasis (TM) in children and its association with primary testicular tumors (PTT).
Methods
A systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement. A priori protocol was registered in the PROSPERO database (CRD42018111119), and a literature search of all relevant studies published until February 2019 was performed. Prospective, retrospective cohort, or cross-sectional studies containing ultrasonography (US) data on the incidence of TM or the association between TM and PTT were eligible for inclusion.
Results
Of the 102 identified articles, 18 studies involving 58,195 children were included in the final analysis. The overall incidence of TM in children with additional risk factors for PTT was 2.7%. In children, the proportion of left TM in unilateral cases was 55.7%, the frequency of bilateral TM was 69.0%, and proportion of classic TM was 71.8% [95% confidence interval (CI) 62.4–81.1%, P = 0.0, I2 = 0.0%]. About 93.5% of TM remained unchanged, and newly detected PTT rate was very low (4/296) during follow-up. The overall risk ratio of TM in children with a concurrent diagnosis of PTT was 15.46 (95% CI 6.93–34.47, P < 0.00001).
Conclusions
The incidence of TM in children is highly variable. Nonetheless, TM is usually bilateral, of the classic type, and remains stable or unchanged at follow-up. Pediatric patients with TM and contributing factors for PTT have an increased risk for PTT; however, there is no evidence to support mandatory US surveillance of children with TM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
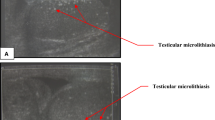
Testicular microlithiasis (TM) is usually incidentally detected by scrotal ultrasonography (US) and is characterized by calcium deposits in the seminiferous tubules [1]. TM can be identified as punctuate, nonshadowing echogenic foci on US [2]. Clinically, the most accepted classification of TM is classic TM (CTM) and limited TM (LTM). LTM is defined as < 5 echogenic foci in both testes, while CTM is defined as ≥ 5 foci in either or both testes [3]. TM is thought to be due to abnormal calcification or the presence of debris in the spermatogenic tubules. However, the exact cause of these calcifications is unknown.
The incidence of TM varies considerably between children according to the study periods, age groups and geographic locations [2]. The incidence of TM ranges from 0.7% to 8.7% in children with potential risk factors for primary testicular tumors (PTT) (testicular pain, testicular masses, infertility/subfertility, personal or family history of TT, cryptorchidism, or other reasons for scrotal US) [2, 4,5,6,7,8,9,10,11], and 4.1% to 4.2% in asymptomatic children [1, 12] according to currently published papers.
The annual incidence of PTT is 3–5 cases per 100,000 men. PTT is the most common tumor in young adults, in which the prognosis is favorable if the condition is diagnosed and treated early. Although many studies determined the prevalence of TM and its association with PTT in the past 20 years, the association between TM and PTT is still under debate, especially in pediatric population [2, 4, 9, 10, 13,14,15,16,17,18,19,20,21]. Some studies found that TM was benign and did not require regular follow-up whereas more contemporary studies recommended a strict follow-up. Consequently, the condition is clinically significant because of its association with testicular malignancy and the potentially elevated risk of malignancy in patients with isolated TM (without a concurrent diagnosis of TT).
To the best of our knowledge, several systematic reviews and meta-analysis have been conducted to determine the association between TM and PTT in adult population [22,23,24], while no systematic reviews on pediatric patients with TM has ever been conducted. And this relevance remains eagerly to be clarified. In addition, there was no systematic review to date determined the incidence characteristics of TM in pediatric populations, including asymptomatic patients with otherwise good clinical outcomes and patients with concurrent urinogenital abnormalities, subtypes of CTM or LTM, unilateral and bilateral TM, according to study periods and age groups. Furthermore, the association between TM and PTT in children remains to be revealed.
There are currently no evidence-based guideline for pediatric urologists and clinicians to guide decision-making for patients with TM. The aim of this systematic review and meta-analysis is to critically explore these topics and their relevance between TM and PTT to aid decision-making and guide future research in children.
Methods
Registry
This study was registered in the PROSPERO database (CRD42018111119). The aims and methods of the investigation were described on February 22, 2019. The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [25].
Information sources and search strategy
The systematic literature search of databases was conducted by two independent reviewers on February 22, 2019. The articles that contained relevant information on TM and PTT of pediatrics were initially searched from PubMed, Cochrane Library, Web of Science Database, Science Direct, China National Knowledge Infrastructure and Wanfang Data. The string terms TM and PTT or synonyms were searched using Boolean operators. Only pediatric population were considered to be included. A MeSH terms search and keywords search were combined. The references of the included studies and reviews were also manually searched.
Definitions and study design
The study population was divided into three groups according to the reasons for US for subgroup analysis: (1) asymptomatic, military volunteers or healthy controls with otherwise good clinical outcomes; (2) symptomatic, including patients with scrotal pain, scrotal masses, swelling, testicular torsion, varicocele, hydrocele or other urogenital symptoms; (3) referral for US examination without providing specific reasons for this examination. The latter two groups were combined as the TM patients with potential risk factors for PTT. The rates of these complications were analyzed separately and then combined to assess the overall effect.
Given the recent advances in US technology, the study period was stratified into three categories—until 2009, 2009–2013, and after 2013—to determine whether the incidence of TM and its association with PTT varied with time. The subtypes of CTM or LTM, unilateral and bilateral TM, and the association of TM and PTT were also analyzed. No other analyses consider age group differences because of the complexity of the analysis of this variable and data limitations.
Apart from comparing the rate of concurrent diagnosis of PTT in patients with and without TM, we also made effort to investigate the interval development of TT. The follow-up information of patients with isolated TM was assessed. And a new incidence rate (number of cases per 10,000 person-months of follow-up) was measured to determine the incidence of PTT in these patients with time concerned.
Eligibility criteria
(1) Pediatric studies (pediatrics defined as age under 19) with statistical data on the incidence/follow-up information of TM or comparative data on the association between TM and PTT; (2) detection of TM by US; (3) when overlapping or duplicate data were found, the most recent or complete data were considered.
Exclusion criteria
(1) Case reports, clinical series, reviews, comments, editorial letters and animal studies; (2) repeated studies or studies with incomplete data; (3) studies that performed the pathological diagnosis of TM without radiological diagnosis; (4) cellular, molecular, or histological studies on TM; (5) studies focused on radiological features/improvements in the detection of TM or microlithiasis in other locations; (6) studies containing only adult patients.
Study selection and data extraction
Two collaborators independently reviewed the electronically and manually retrieved articles. After screening the titles and abstracts, potentially relevant studies were selected. A full-text review was performed subsequently. All disagreements were solved by discussion or by a third reviewer.
Each included article was thoroughly reviewed. The following data were extracted (Table 1): first author, year, location, study period, sample size, population and transducer frequency of US. In addition, the following seven items were marked with “√” for convenience of recognizing the paper contents: incidence of TM, subtypes of PTT, type of TM, follow-up period, laterality of TM, additional risk factors for PTT and stratification according to age groups.
The incidence of TM was determined using data from specific groups (asymptomatic patients, patients with additional risk factors for PTT and patients with CTM/LTM) and data on the laterality of TM and stratification according to age groups (Supplementary Table 1).
The association between TM, overall incidence of testicular germ-cell tumor (TGCT) and the incidence of TGCT in children in different periods according to sample size and follow-up time and strategy is depicted in Table 2. An e-mail was sent to the authors when the included articles published in the past 10 years contained incomplete data.
Quality assessment
The quality of the studies was assessed using the Agency for Healthcare Research and Quality (AHRQ), with modifications to match the needs of the current meta-analysis. The questionnaire contained 11 items, in which each item had three possible answers: “Yes,” “No,” or “Unclear” (Supplementary Table 2).
Statistical analysis
STATA software version 15.0
The mean incidence of TM was determined by meta-analysis of single rate. The meta-analysis of risk ratios (RRs) was performed using STATA 15.0 software (Stata Corporation, College Station, Texas, USA) and the random effects model, which assigned a weight to each study based on both within-study variance and between-study heterogeneity. The commands used in the meta-analysis after installing the meta package were ssc install metan (data editing); gen rate = case/total; gen ser = sqrt(rate*(1–rate)/total); metan rate ser, label (namevar = author year) by (subgroup) random. The mean incidence of TM in asymptomatic patients and patients with additional risk factors for PTT according to the study periods, CTM/LTM and age groups was measured separately using these commands. The laterality of TM was also determined. Begg’s adjusted rank correlation test and Egger’s regression asymmetry test were used for assessing publication bias. Publication biases with a P value larger than 0.05 in both tests were considered not significant.
RevMan software version 5.3
Dichotomous variables were analyzed using Review Manager version 5.3 (Cochrane Collaboration, Oxford, United Kingdom) and the Mantel–Haenszel method. The crude RRs and their 95% confidence intervals (CIs) were calculated using random effects models to determine the association between TM and PTT. The heterogeneity of the studies was tested using both the χ2 test (P ≥ 0.1 indicated low heterogeneity) and inconsistency index (I2) statistics. Publication bias was assessed by funnel plots. Begg’s test and Egger’s test were adopted (by STATA) if the funnel plot symmetry was not easy to recognize. The χ2 test was used to determine inter-subgroup differences. P values smaller than 0.05 were considered significant.
Results
Identification and eligibility of the studies
The initial database search yielded 102 articles (Fig. 1). Another two articles were found by manual searching. After eliminating eight duplicate articles, 96 titles and abstracts were screened. After comprehensively screening 25 full texts, 18 manuscripts complied with the eligibility criteria of this meta-analysis [1,2,3,4,5,6,7,8,9,10,11, 20, 26,27,28,29,30,31], 16 studies evaluated the incidence of TM and 5 manuscripts compared the association between TM and PTT.
Quality assessment
There is no quantitative evaluation of the AHRQ questionnaire. The 11 items used to score the included studies are shown in Supplementary Table 2. Almost all the studies that determined the association between TM and PTT had an acceptable quality.
Incidence of TM
The individual incidence of TM in children is shown in Supplementary Table 1. The pooled mean incidence of TM with 95% CI using I2 in children is shown in Table 3.
Overall incidence of TM
Eighteen studies involving 58,195 children were evaluated to determine the incidence of TM. Two studies assessed the incidence of TM in asymptomatic patients. The mean incidence of TM in the asymptomatic pediatric population was 4.2% (95% CI 2.7–5.6%, P = 0.0, I2 = 0%).
The population with potential risk factors for PTT was stratified into two main subgroups—symptomatic, referred for US—according to the reasons for scrotal US. The overall incidence of TM in children with additional risk factors for PTT was 2.7% (95% CI 2.0–3.3%, P = 0.0, I2 = 92.0%). The mean incidence of TM in children who were symptomatic and referred for US was 3.7% and 2.5%, respectively.
Incidence of TM in different periods
To analyze the variance in the incidence of TM in different periods, the appropriate data were stratified according to the following time intervals: before 2009, 2000–2013 and after 2013 (using data from 5, 6, 5 studies).
In children, the mean incidence was 1.6%, 3.8% and 3.0%, respectively. Considering only two study periods—after 2009 and before 2009, the mean incidence of TM after 2009 was 3.3% in children. The incidence of TM tended to increase with time.
Incidence of CTM/LTM
Seven and five studies determined the pooled incidence of CTM and LTM in children, respectively. The pooled mean incidence of CTM and LTM was 2.5% and 0.9%, respectively.
Four pediatric studies investigated the incidence of both CTM and LTM at the same time. The rate of CTM and LTM in TM was determined by analyzing data on the individual incidence of these complications. The proportion of CTM in children was 71.8% (95% CI 62.4–81.1%, P = 0.0, I2 = 0.0%).
Incidence of TM according to laterality
In children, the pooled mean incidence of left, right, unilateral and bilateral TM was 0.9%, 0.8%, 0.7% and 1.6%, respectively (Table 3). We also determined the proportion of left or right TM in unilateral cases and the incidence of unilateral and bilateral TM without considering the incidence of CTM/LTM.
In children, the prevalence of left TM in unilateral cases was 55.7%, while the frequency of bilateral TM was 69.0%. These results indicated that bilateral TM was much more common than unilateral TM in pediatric population.
Incidence of TM according to age groups
Two pediatric studies determined the incidence of TM in 2–3-year prepubertal age groups [2, 12]. Data are shown in Table 3. The inter-study heterogeneity was very high. And the results were not significant.
Association between TM and PTT
Five studies involving 1299 children with TM and 43,117 children without TM were included in the meta-analysis to assess the association between TM and PTT. Among them, four original studies determined the association between TM and PTT in pediatric population with potential risk factors for PTT [2, 9, 10, 20]. Only one study investigated the relevance of TM and PTT in asymptomatic children [12]. Nonetheless, PTT was not detected in 28 asymptomatic children with TM and 642 asymptomatic children without TM.
The populations that were symptomatic and referred for US constituted the group with additional risk factors for PTT. The pooled RR of TT in the population with TM compared with that without TM is shown in Fig. 2. The RR of TM with a concurrent diagnosis of PTT in children was 15.46 (95% CI 6.93–34.47, P < 0.00001, I2 = 58%), with high heterogeneity (P for heterogeneity < 0.00001, I2 > 50%). The funnel plot showed a roughly asymmetrical distribution, indicating suspicious publication bias. In the groups that were symptomatic and referred for US, TM was associated with an increased risk of PTT, with a RR of 5.97 and 21.57, respectively (Fig. 2). The test for subgroup difference (χ2 = 2.16, P = 0.14) showed that there were no significant differences in the relative RR between these two groups.
The forest plot indicates the risk ratio of a concurrent diagnosis of primary testicular tumor (PTT) in the presence of testicular microlithiasis (TM) in a selected population with potential additional risk factors for PTT among pediatric population. M-H, Mantel–Haenszel odds ratio, CI confidence interval, TM testicular microlithiasis, US ultrasonography, df degrees of freedom, I2 inconsistency index
Follow-up outcomes of pediatric population with TM
Ten studies conducted the follow-up of pediatric population with previously diagnosed TM, the follow-up time, strategy and newly detected tumor characteristics are depicted in Table 2. A total number of 296 TM patients were included, in which the follow-up time ranged from 1–85 months. Among them, only four children with TM were diagnosed with newly detected PTT during a relatively long follow-up time. In addition, two of which had a history of ipsilateral or contralateral tumor or cryptorchidism. According to our analysis, about 93.5% of TM remained stable or unchanged during follow-up.
Discussion
This systematic review and meta-analysis first determined the epidemiological incidence of TM according to CTM/LTM subtypes, age groups, study periods and TM laterality among pediatric population. The study also determined the association between TM and synchronous/heterochronous diagnosis of PTT and addressed the follow-up information and findings of pediatric patients with TM according to currently published papers.
This study is the most comprehensive review on the incidence of TM and its association with PTT among pediatric population, but still has some limitations. This systematic review included all relevant studies published worldwide from 1998 to 2017, regardless of frequency of US transducers. And there was no adjustment on these differences. The large time span of these studies and recent advances in US technology increased the variability in the detection level of TM. For these reasons, differences in multicenter approaches, US parameters and equipment between studies are unavoidable. Therefore, considering the within-study variance and between-study heterogeneity, the random-effect model was used in our study, no matter single-rate meta-analysis or dichotomous variables.
Cooper et al. pointed out that the incidence of TM varied from 4.60% to 9.02% considering two study periods: before 2001 and after 2001 [2]. Enlighted by his view, the prevalence data were divided into three time intervals—past 5 years (after 2013), past 5–10 years (2009–2013) and > 10 years (before 2009). And the results indicated that the prevalence tended to increase with time. Considering two study periods—before 2013 and after 2013, the prevalence of TM increased from 1.6% to 3.3% in the pediatric population. In our opinion, advances in US technology and health awareness led to the increased detection of TM.
The overall incidence of TM was 4.2% in asymptomatic children, whereas the overall incidence of TM in children with additional risk factors for PTT was 2.7%, according to currently available data. Publication bias seems to be the main reason why the incidence of TM in asymptomatic children is higher than that in children with pre-existing conditions.
Among TM patients, CTM accounted for approximately 71.8% in children. LTM may not be easily detected compared with CTM on US. Children do not usually cooperate with static US. For this reason, the detection of LTM in this population is more challenging, leading to a higher rate of CTM cases in children. Furthermore, advances in US technology in recent years have increased the detection rate of TM in children relative to adults.
The overall incidence of TM differed significantly according to the age groups (Table 3) and increased with age. Similarly, the overall incidence of TT increased with age regardless of the presence of TM. However, the incidence of TM did not increase linearly with advancing age. One peak occurred at age 6–14 years. Further cellular and molecular studies are necessary to address the pathogenesis of TM.
In asymptomatic pediatric populations with otherwise good clinical outcomes, there is no convincing evidence supporting that TM alone is premalignant. In populations with additional risk factors for PTT, the presence of TM increased the risk of TT with a relative RR of 15.46 for a concurrent diagnosis of PTT in children, but with strong evidence of heterogeneity and suspicious publication bias. After comprehensive summary of pediatric patients with TM, we found that more than 90% of TM remained unchanged. And the newly detection rate of PTT was very low (less than 1%, 2/296), if there was no ipsilateral or contralateral tumor or operation history. Our findings suggest that frequent US surveillance is not required in pediatric patients with TM, unless they had severe genitourinary abnormalities.
Several case reports demonstrated a causal relationship between the pre-existence of TM and the subsequent development of TT [32,33,34]. Nonetheless, these studies had an unacceptable bias toward favorable outcomes: (1) the analysis of follow-up information from a clinical series of patients with isolated TM indicated that approximately 90% of the cases of TM remained stable during follow-up; (2) the cumulative incidence of newly detected PTT in a relatively short time was very low, ranging from 0 to 46.30 cases per 10,000 person-months; (3) most patients with newly detected tumors during follow-up had a history of ipsilateral or contralateral testicular abnormality or tumor; (4) the sample size was small, and the follow-up time was short.
In pediatric populations that were symptomatic and referred for US, TM was associated with an increased risk of PTT with a respective RR of 5.97 and 21.57, respectively (Fig. 2). Although the incidence of TM and TT in populations from clinical studies was higher than that in the general population, this finding indicates that the presence of TM should be considered, especially in subjects with scrotal or testicular abnormalities or symptoms. During follow-up, some studies recommend a testicular examination, surveillance imaging or both, whereas others indicate that these procedures are not necessary [35]. Although US contributes to the early detection of TTs, DeCastro et al. have pointed out that frequent US surveillance is not cost-effective and does not significantly improve the outcomes associated with TT [36]. So we do not recommend regular US surveillance for children with TM, but testicular examination by themselves or parents.
In conclusion, the incidence of TM varies significantly between pediatric populations according to age groups, study periods and laterality. TM is most commonly bilateral, of the classic type, and remains stable or unchanged at follow-up. The overall incidence of TM in children with additional risk factors for PTT is 2.7%, which is much higher than expected.
There is no convincing evidence supporting that TM alone is premalignant. TM was strongly associated with increased diagnosis of PTT in children with potential risk factors for PTT. The incidence of TT in patients with isolated TM was very low during follow-up unless they had a history of ipsilateral or contralateral abnormality or tumor.
We currently do not recommend regular US surveillance for children with TM, but testicular examination by themselves or parents, unless they have severe genitourinary abnormalities or history of tumors or operations.
References
Poyrazoglu S, Saka N, Agayev A, Yekeler E. Prevalence of testicular microlithiasis in males with congenital adrenal hyperplasia and its association with testicular adrenal rest tumors. Hormone Res Paediatr. 2010;73:443–8.
Cooper ML, Kaefer M, Fan R, Rink RC, Jennings SG, Karmazyn B. Testicular microlithiasis in children and associated testicular cancer. Radiology. 2014;270:857–63.
Goede J, Hack WW, van der Voort-Doedens LM, Pierik FH, Looijenga LH, Sijstermans K. Testicular microlithiasis in boys and young men with congenital or acquired undescended (ascending) testis. J Urol. 2010;183:1539–43.
Chiang LW, Yap TL, Asiri MM, Phaik Ong CC, Low Y, Jacobsen AS. Implications of incidental finding of testicular microlithiasis in paediatric patients. J Pediatr Urol. 2012;8:162–5.
Deganello A, Svasti-Salee D, Allen P, Clarke JL, Sellars MEK, Sidhu PS. Scrotal calcification in a symptomatic paediatric population: prevalence, location, and appearance in a cohort of 516 patients. Clin Radiol. 2012;67:862–7.
Dutra RA, Perez-Bóscollo AC, Melo EC, Cruvinel JC. Clinical importance and prevalence of testicular microlithiasis in pediatric patients. Acta Cir Bras. 2011;26:387–90.
Leenen AS, Riebel TW. Testicular microlithiasis in children: sonographic features and clinical implications. Pediatr Radiol. 2002;32:575–9.
Rhee A, Cooper M, Misseri R, Kaefer M, Meldrum K, Cain M, et al. Pediatric testicular microlithiasis: what's a doctor to do? J Urol. 2012;187:E342.
Trout AT, Chow J, McNamara ER, Darge K, Ramirez Grueso R, Munden M, et al. Association between testicular microlithiasis and testicular neoplasia: large multicenter study in a pediatric population. Radiology. 2017;285:576–83.
Volokhina YV, Oyoyo UE, Miller JH. Ultrasound demonstration of testicular microlithiasis in pediatric patients: is there an association with testicular germ cell tumors? Pediatr Radiol. 2014;44:50–5.
Yesil S, Tanyildiz HG, Sahin G. How should we monitor boys with testicular microlithiasis? Pediatr Hematol Oncol. 2016;33:171–7.
Goede J, Hack WW, van der Voort-Doedens LM, Sijstermans K, Pierik FH. Prevalence of testicular microlithiasis in asymptomatic males 0 to 19 years old. J Urol. 2009;182:1516–20.
Chen JL, Chou YH, Tiu CM, Chiou HJ, Wang HK, Chiou SY, et al. Testicular microlithiasis: analysis of prevalence and associated testicular cancer in Taiwanese men. J Clin Ultrasound. 2010;38:309–13.
Coffey J, Huddart RA, Elliott F, Sohaib SA, Parker E, Dudakia D, et al. Testicular microlithiasis as a familial risk factor for testicular germ cell tumour. Br J Cancer. 2007;97:1701–6.
Derogee M, Bevers RF, Prins HJ, Jonges TG, Elbers FH, Boon TA. Testicular microlithiasis, a premalignant condition: prevalence, histopathologic findings, and relation to testicular tumor. Urology. 2001;57:1133–7.
Heller HT, Oliff MC, Doubilet PM, O'Leary MP, Benson CB. Testicular microlithiasis: prevalence and association with primary testicular neoplasm. J Clin Ultrasound. 2014;42:423–6.
Korde LA, Premkumar A, Mueller C, Rosenberg P, Soho C, Bratslavsky G, et al. Increased prevalence of testicular microlithiasis in men with familial testicular cancer and their relatives. Br J Cancer. 2008;99:1748–53.
Kosan M, Gonulalan U, Ugurlu O, Oztekin V, Akdemir O, Adsan O. Testicular microlithiasis in patients with scrotal symptoms and its relationship to testicular tumors. Urology. 2007;70:1184–6.
Middleton WD, Teefey SA, Santillan C, McFarland EG, Sadeghi S. Prospective evaluation of the incidence of testicular microlithiasis and its association with testicular tumors. Radiology. 2000;217:558.
Otite U, Webb JA, Oliver RT, Badenoch DF, Nargund VH. Testicular microlithiasis: is it a benign condition with malignant potential? Eur Urol. 2001;40:538–42.
Ringdahl E, Claybrook K, Teague JL, Northrup M. Testicular microlithiasis and its relation to testicular cancer on ultrasound findings of symptomatic men. J Urol. 2004;172:1904–6.
Rashid HH, Cos LR, Weinberg E, Messing EM. Testicular microlithiasis: a review and its association with testicular cancer. Urol Oncol. 2004;22:285–9.
Tan IB, Ang KK, Ching BC, Mohan C, Toh CK, Tan MH. Testicular microlithiasis predicts concurrent testicular germ cell tumors and intratubular germ cell neoplasia of unclassified type in adults: a meta-analysis and systematic review. Cancer. 2010;116:4520–32.
Wang T, Liu L, Luo E, Liu T, Wei A. A meta-analysis of the relationship between testicular microlithiasis and incidence of testicular cancer. Urol J. 2015;12:2057–64.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Dagash H, Mackinnon EA. Testicular microlithiasis: what does it mean clinically? BJU Int. 2007;99:157–60.
Furness PD, Husmann DA, Brock JW 3rd, Steinhardt GF, Bukowski TP, Freedman AL, et al. Multi-institutional study of testicular microlithiasis in childhood: a benign or premalignant condition? J Urol. 1998;160:1151–4; discussion 1178.
Marte A, Pintozzi L, Creti G, Chiesa PL, Renzo DD, Gasparella M, et al. Long-term follow-up of testicular microlithiasis in children and adolescents: multicenter prospective cohort study of the Italian society of pediatric urology. Eur J Pediatr Surg. 2017;27:155–60.
Miller FN, Rosairo S, Clarke JL, Sriprasad S, Muir GH, Sidhu PS. Testicular calcification and microlithiasis: association with primary intra-testicular malignancy in 3,477 patients. Eur Radiol. 2007;17:363–9.
Nishimura Y, Moriya K, Nakamura M, Nishida M, Sato M, Kudo Y, et al. Prevalence and chronological changes of testicular microlithiasis in isolated congenital undescended testes operated on at less than 3 years of age. Urology. 2017;109:159–64.
Xia B, Sun L, Lin Z, Xu W, Wang B, Liu L. The application of ultrasonography in diagnosing testicular microlithiasis in children. Chin J Pediatr Surg. 2002;1:28–30 (in Chinese).
Akhter W, Khan SAA, Khan FR, Younis A, Khan SMJZ. Testicular microlithiasis: case report and literature review. Afr J Urol. 2012;18:38–40.
Berger A, Brabrand K. Testicular microlithiasis–a possibly premalignant condition. Report of five cases and a review of the literature. Acta Radiol. 1998;39:583–6.
Whitacre R, Zaslau S. Bilateral testicular microlithiasis with a unilateral testicular germ cell tumor: a case report. W Virgin Med J. 2003;99:233–4.
Winter TC, Kim B, Lowrance WT, Middleton WD. Testicular microlithiasis: what should you recommend? AJR Am J Roentgenol. 2016;206:1164–9.
DeCastro BJ, Peterson AC, Costabile RA. A 5-year followup study of asymptomatic men with testicular microlithiasis. J Urol. 2008;179:1420–3; discussion 1423.
Funding
This study was supported by the National Natural Science Foundation of China (Protocol no. 81873828).
Author information
Authors and Affiliations
Contributions
CJY conceived and designed the meta-analysis, independently searched the electric databases, and independently extracted the data, led analysis and interpretation of data, drafted the manuscript and revised content based on feedback. JDL independently searched the electric databases, and independently extracted the data, led analysis and interpretation of data, drafted the manuscript and revised content based on feedback, and acted as second reviewer. JZ led analysis and interpretation of data, drafted the manuscript and revised content based on feedback. TXZ and YW assisted with the retrieval of the database and acquisition of data, assisted with the interpretation of data and provided critical revision of drafts. TL, DWH, and GHW assisted with the conception and design, interpretation of data, and critical revision of drafts. SDW conceived and designed the meta-analysis, and acted as the corresponding author, provided funding support, assisted with interpretation of data, provided critical revision of drafts and acted as the third (mediating) reviewer. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yu, CJ., Lu, JD., Zhao, J. et al. Incidence characteristics of testicular microlithiasis and its association with risk of primary testicular tumors in children: a systematic review and meta-analysis. World J Pediatr 16, 585–597 (2020). https://doi.org/10.1007/s12519-019-00328-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-019-00328-1