Abstract
Purpose of Review
The goal of this review is to outline the new guidelines released by the ASE/EACVI that seek to simplify the assessment of diastolic function and evaluate the use and potential application of new and emerging technologies.
Recent Findings
The latest guidelines have decreased the number of parameters needed to evaluate diastolic function to 3. The parameters necessary include peak tricuspid regurgitation (TR) velocity, average E/e′, and indexed left atrial volume (LAVi). At least 2 out of 3 must be positive to determine diastolic dysfunction. There are certain disease states that limit the application of the new guidelines and diastolic stress testing may be indicated in inconclusive cases. New and emerging technologies such as global longitudinal strain (GLS) may provide new opportunities to determine LV filling pressures.
Summary
New guidelines issued by the ASE and EACVI have simplified the assessment of diastolic function and should be implemented in daily practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) affects 5.7 million Americans over 20 years of age and its prevalence will increase 46 % to over 8 million people by 2030 [1]. It is associated with significant morbidity and mortality as 1 in 9 deaths has heart failure mentioned on the death certificate [2]. Diastolic function is a significant subset of this group of patients as 55 % of patients with symptomatic heart failure have preserved ejection fraction (EF) and the vast majority have some degree of diastolic dysfunction. HF with preserved EF is associated with mortality rates similar to that of HF with reduced EF, making the assessment of the diastolic function vital to this group of patients [1, 3].
Historical Perspective
The guidelines proposed by the ASE and European Association of Cardiovascular Imaging sought to determine left ventricular (LV) filling pressures and diastolic function by simple echocardiographic parameters that were reliable, highly feasible, and reproducible. The gold standard to which these parameters were compared was invasive measurement either mean pulmonary capillary wedge pressure (PCWP), mean left atrial pressure (LAP) (in the absence of significant mitral stenosis), and/or LV end diastolic pressure (LVEDP) [4]. Even though these pressures are different in absolute terms, they are closely related, change somewhat predictably with myocardial disease.
The optimal performance of the LV depends on its ability to be a compliant chamber in diastole that allows it to fill from low LA pressure, before ejecting blood at arterial pressures. The sooner LV filling pressures drop below LAP, the greater the LV filling time [5••].
Elevated filling pressures are the main physiologic consequence of diastolic dysfunction. Filling pressures are considered elevated when a PCWP >12 mmHg or when LVEDP is >16 mmHg.
Echocardiographic Assessment of LV Diastolic Function
The guidelines begin with proposing that determination of diastolic function grade is based on clinical history, age of patient quality 2D images and properly optimized Doppler signals. A single measurement within the normal range does not necessarily equate with a normal study and determination of grade should begin on the presence or absence of elevated LV filling pressures. For patients with normal EF with no obvious cardiac pathology, 4 parameters are recommended: average E/e′ velocity >14 (septal e′ <7 cm/s or lateral e′ <10 cm/s), LA volume index >34 mL/m2, and peak TR velocity >2.8 m/s. Should only lateral or septal e′ velocity is available and under those circumstances, a lateral E/e′ ratio >13 or septal E/e′ ratio >15 is considered abnormal [5••] (Fig. 1). Note that more than 50% of these parameters have to be abnormal to call abnormal diastolic dysfunction. An important caveat to remember is the aforementioned parameters are only applicable to patients without any heart disease.
Algorithm for diagnosis of LV diastolic dysfunction in subjects with normal LVEF. Reprinted from Nagueh, Sherif. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging, J Am Soc Echocardiogr 2016;29:277-314 with permission from Elsevier
LA maximum volume indexed to body surface area (LAVi) the current recommended value and not LA anterior-posterior diameter by M-mode as LA enlargement can occur in both the medial-lateral and superior-inferior directions only, which would result in an increased LA volume while the diameter may be within the normal range [6•].
Determination of Diastolic Dysfunction Grade
Given that LAP relates with PCWP, and thus, pulmonary congestion symptoms at the time of the echocardiogram, the algorithm to determine specific diastolic dysfunction grade presented by the ASE guidelines begins with mitral inflow velocities [in the absence of atrial fibrillation (AF)], significant mitral valve disease; any mitral stenosis or anything greater than moderate mitral regurgitation (MR). It must also be noted that normal aging is associated with many changes in cardiovascular system, especially slowing of LV relaxation. Hence, filling patterns in the elderly resemble younger patients (40–60) with mild diastolic dysfunction and should be taken into account when evaluating diastolic function [7–18].
Similar to the prior guidelines, mitral E/A ratio ≤0.8 and E velocity ≤50 cm/s represented normal LAP and grade 1 diastolic dysfunction. An E/A ratio ≥2 indicates elevated LAP and grade 3 diastolic dysfunction. For mitral inflow patterns between 0.3 and 2 or ≤0.8 with E > 50 cm/s, it is recommended that 3 additional criteria be evaluated: average E/e′ >14, TR velocity >2.8 m/s, and LA volume index >34 ml/m2. If 2 out of 3 are negative, there is normal LAP/grade I diastolic dysfunction. If 2 out of 3 or all 3 are positive, there is elevated LAP/grade II diastolic dysfunction. If only 2 out of the 3 criteria are available, 2 negative is considered normal LAP/grade 1, 2 positive criteria is considered elevated LAP/grade II, with 1 positive, and 1 negative is considered indeterminate for both LAP and diastolic dysfunction [5••] (Fig. 2). Note this algorithm applies to patients with cardiac pathology: decreased ejection fraction (<50%) or patients with diastolic dysfunction and preserved ejection fraction. This is seen in patients with myocardial diseases such as coronary artery disease with wall motion abnormalities, hypertrophy from hypertension, cardiomyopathies ( ie amyloid) or known heart failure with preserved ejection fraction.
Algorithm for estimation of LV filling pressures and grading LV diastolic function in patients with depressed LVEF and patients with myocardial disease and normal LVEF after consideration of clinical and other 2D data. Note pulmonary vein S/D ratio <1 can be used to conclude elevated LAP in patients with reduced LVEF. JASE, vol 29/issue 4, author(s), Nagueh, Sherif. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging, J Am Soc Echocardiogr 2016;29:277-314 with permission from Elsevier
Limitations of the diastolic function algorithm
There are several situations where the algorithm may be difficult to implement. The most obvious is AF (with lack of A wave), at least moderate mitral annular calcification, any mitral stenosis, prior mitral valve surgery, and mitral regurgitation more than moderate. Patients with LV assist devices (LVAD), left bundle branch block, and ventricular pacing the algorithm.
Estimating LV Filling Pressures in Specific Cardiovascular Diseases
Hypertrophic Cardiomyopathy (HCM)
The 2016 update recommend a comprehensive approach to assess LV diastolic dysfunction in patients with HCM. The individual variables described earlier, when used alone, have modest correlations with LV filling pressures with patients with HCM, likely due to variability in phenotype, obstructive versus nonobstructive physiology, muscle mass, and amount of myocardial fiber disarray. More recently, studies using speckle-tracking echocardiography (STE) have reported the association between LV systolic and diastolic strain, LA strain, and LV diastolic function. Furthermore, they have linked exercise tolerance to LV function parameters, such as torsion and untwisting rate [19–22].
Restrictive Cardiomyopathy
Restrictive cardiomyopathies comprise a heterogeneous group of diseases including but not limited to cardiac amyloidosis, idiopathic restrictive cardiomyopathy, and sarcoidosis. Diastolic dysfunction can vary significantly in cardiac amyloidosis, ranging from grade I with normal LV filling pressures in early stages, to grade III in later stages when LV relaxation is significantly impaired and LV filling pressures become elevated. Assessment of diastolic function in these patients has evolved from mitral inflow and pulmonary vein flow, to tissue Doppler imaging, and now STE, STE which can be used to measure both strain and strain rate. Advanced grades of restrictive cardiomyopathy are characterized by mitral inflow E/A ratio >2.5, E velocity deceleration time (DT) <150 ms, isovolumic relaxation time (IVRT) <50 ms [19], decreased septal and lateral e′ velocities, but higher lateral e′ compared with septal e′ (which is reversed in constrictive pericarditis [annulus reversus]), E/e′ >14, and LA volume index >50 ml/m2. The presence of normal annular e′ velocity in a patient referred with heart failure should raise suspicion of pericardial constriction [23, 24]. STE of LV myocardium in patients with cardiac amyloidosis has shown a distinctive phenotype of apical sparing compared to hypertensive heart disease, HCM, and aortic stenosis. The ratio of LV free wall strain to LV septal strain by STE is about 1 in patients with restrictive cardiomyopathy, usually <1 in patients with constriction because of less deformation of the anterolateral LV wall compared to the septum. It is important to make the distinction between restrictive LV filling, which can occur in other diseases such as coronary artery disease, HCM, dilated cardiomyopathy, and restrictive cardiomyopathy as grade III diastolic dysfunction is associated with a poor outcome [25–29].
Valvular Heart Disease
In the case of mitral stenosis or regurgitation, transmitral velocities and annular dynamics are mostly determined by the degree of valvular disease and offer limited value as indicators of LV disease. Patients with mitral stenosis typically have normal or reduced LV filling pressures in the absence of significant myocardial disease. A semi-quantitative estimate of instantaneous LAP can be provided the shorter the IVRT and how high the peak E velocity is. LAP is significantly elevated if the mitral A velocity remains >1.5 m/s. The ratio of IVRT versus the time interval between the onset of mitral E velocity and annular e′ velocity (IVRT/TE-e′) correlates well with mean PCWP and LAP in patients with mitral stenosis as e′ velocity is not only reduced but also delayed and occurs at the LA-LV pressure crossover point. However, E/e′ ratio is not useful in this instance. For mitral regurgitation (MR), velocity recording by CW Doppler provides a highly specific, but non-sensitive sign of increased LAP with early peaking. E/e′ ratio has a direct significant correlation with LAP, increased hospitalization, and mortality in patients with depressed EFs, however, does not appear to be useful in patients with preserved EFs. The IVRT/TE-e′ ratio >3 correlates reasonably well with PCWP >15 mmHg in these patients [30]. Aortic stenosis usually portends no difficulties to the application of the guidelines except for the coexistence of moderate to severe MAC [31, 32]. Severe aortic regurgitation can interfere with the sample volumes of mitral inflow velocities, and careful positioning of the sample volumes is necessary. Acute severe AR abbreviates the LV diastolic period, which lead to diastolic MR, an indication of elevated LVEDP.
Atrial Fibrillation
LV diastolic dysfunction leads to LA dilatation, which can precipitate AF, and is common amongst patients with heart failure. Doppler assessment of LV diastolic function is limited by the beat to beat variability, and absence of organized atrial activity. In depressed LVEF, mitral DT ≤160 ms has reasonable accuracy for the prediction of increased LV diastolic pressures and adverse clinical outcomes. Other Doppler measurements, which may be employed to determine diastolic dysfunction, are mitral E velocity (≥1.9 m/s), IVRT ≤65 ms, DT of pulmonary venous diastolic velocity ≤220 ms,E/ Vp ratio ≥1.4, and E/e′ ratio ≥11 [33–35]. The IVRT/TE-e′ ratio can also be used to predict LV filling pressures in the setting of impaired LV relaxation [36, 37].
AV Block and Pacing
Properly timed atrial contractions increase cardiac output by 25–30 %. Cardiac conduction abnormalities due to disease, aging, drugs, or pacing can adversely affect AV synchrony, synchronous LV contraction, and relaxation may alter LV systolic and diastolic function. If the PR interval is too short, atrial filling is terminated by early ventricular contraction, reducing mitral A duration, and therefore, LV end diastolic volume and cardiac output. First-degree AV block of 200–280 ms is well tolerated, but ≥280 ms leads to fusion of the E and A velocities [4]. If atrial contraction occurs before early diastolic mitral flow velocity has decreased to ≤20 cm/s, the E/A ratio is reduced further due to a much higher A wave velocity [38]. The resulting E/A ratio is usually less than 1 and can be misinterpreted as impaired relaxation. A right bundle branch block delays activation of the RV myocardium, and although minor changes to LV and RV synchrony are observed, no studies have shown that this leads to meaningful changes in LV diastolic variables or exercise capacity. A left bundle branch block, however, is usually associated with heart disease and LV diastolic dysfunction. As long as there is no fusion of mitral E and A velocities, all the variables to evaluate diastolic function and filling pressures remain valid. Cardiac pacing has a varied effect on LV systolic and diastolic function. Chronic RV pacing induces LV dyssynchrony which reduces LV filling, LV ejection fraction, and cardiac output, leading to an increased incidence of heart failure and AF. There are few studies that have explored at the utility of mitral annular velocities in this instance and their accuracy is decreased in the presence of bundle branch block, RV pacing, and cardiac resynchronization therapy [39–41].
Diastolic Stress Test
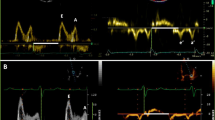
Myocardial relaxation is one of the earliest manifestations of myocardial dysfunction and is consistently reduced in all forms of disease including hypertensive heart disease, ischemia, and HCM [42]. Exercise echocardiography is frequently used to detect reduced LV systolic and/or diastolic reserve capacity in the setting of coronary disease or diastolic dysfunction. Mitral annular e′ velocity increases with early diastolic E velocity in normal subjects during exercise so that E/e′ ratio remains unchanged from rest to stress [43]. Previous studies have shown that the higher the e′ is, the higher the exercise capacity. Augmented relaxation (e′) is reduced in patients with diastolic dysfunction and has lower velocities. Several studies have reported good correlation between E/e′ ratio and invasively obtained PCWP pressure [43]. A diastolic stress test is indicated when the resting echocardiogram does not provide the answer for dyspnea and exercise intolerance. There is no need to undergo stress testing for patients with completely normal hearts (preserved e′ velocities, normal resting diastolic function). Consequently, patients with abnormal results at baseline consistent with elevated LV filling pressures should not be referred for a stress test because cardiac etiology of dyspnea has already been established. The most appropriate patients are those with dyspnea, exercise intolerance, grade 1 diastolic dysfunction, and normal LA mean pressures at rest. Diastolic stress should be performed with exercise (supine bike or treadmill) and not dobutamine as the drug does not replicate day to day physiologic stress. The test is considered definitely abnormal (indicating diastolic dysfunction) when all of the following 3 conditions are met: average E/e′ >14 or septal E/e′ ratio >15 with exercise, peak TR velocity >2.8 m/s with exercise, and septal e′ velocity is <7 cm/s or lateral e′ velocity <10 cm/s [43–46]. Isolated increase in TR velocity should not be used to draw conclusions as normal subjects can have a significant increase in peak TR velocity related to increased pulmonary blood flow. In these patients, invasive hemodynamic investigation with exercise may be necessary. Data regarding prognostic utility of diastolic stress testing is scarce. Increased LV filling pressures (E/e′ >13) with exercise has shown incremental prognostic power to clinical parameters as well as 2D findings diagnostic of myocardial ischemia [47]. In the example listed above, a 65-year-old woman was referred for a stress test for the evaluation of shortness of breath that was thought to be cardiac or pulmonary in etiology. She exercised 5.8 METS (82 % of predicted) and reported some generalized fatigue. At rest, the diastolic parameters would be assessed as grade 1 with normal LAP based on mitral E velocity of 57 cm/s, E/A ratio <0.8, and average E/e′ of 9. During stress, however, the E velocity increases to 121 cm/s, E/A ratio 3.0, but with an average E/e′ of 17.3, indicating diastolic dysfunction (Fig. 3). The overall recommendations are summarized in Table 1.
Novel and emerging parameters in the assessment of diastolic function
Deformation imaging with global longitudinal strain (GLS) by STE has become an increasingly popular tool to assess early stages of systolic dysfunction, as well as for the assessment of diastolic function. Global myocardial peak diastolic strain and strain rate at the time of E avoids Doppler-associated angulation errors and tethering artifacts. Many studies have shown this method to have reasonable accuracy in predicting LV filling pressures in patients with E/e′ ratio of 8–15, normal EF, and regional dysfunction with low inter and intra-observer variability [48–50].
LV untwisting rate (torsion) by 2D speckle tracking imaging has also shown promise in determining LV filling pressures. Repeated measure regression models showed moderately strong correlation of peak LV twisting with peak LV untwisting rate (r = 0.74), as well as correlations of peak LV untwisting rate with the time constant of LV pressure decay. While normal untwisting rates can be seen in patients with diastolic dysfunction, the timing of peak untwisting rate is typically abnormal in patients with diastolic dysfunction [50, 51].
Recently, there have been studies demonstrating an inverse correlation between LA strain and mean PCWP. The correlation appears to be stronger in patients with reduced LVEF, but significant correlations were noted in patients with preserved LVEF as well. LA deformation was feasibly measured, and along with invasively measured PCWP, was used to estimate LA stiffness. E/e′ ratio was employed in conjunction with LA strain to derive a noninvasive dimensionless parameter. It was shown that LA systolic strain was significantly lower in patients with diastolic heart failure than those patients with diastolic dysfunction. Furthermore, LA stiffness was highest in patients with systolic heart failure when compared to those with only diastolic dysfunction, but higher than normal controls. LA strain and stiffness appear to be a promising variable in distinguishing patients with HFpEF from those with diastolic dysfunction who are not in heart failure [51, 52].
Examples of Diastolic Function Grade
Figure 4 shows a 40-year-old woman who presented for evaluation of palpitations and syncope. She has no prior history of cardiac disease and has an EF of 55%. Tile A depicts LAVi of 23.1 ml/m2; Tile B is pulsed wave Doppler of mitral inflow depicting both E velocity of 1.1 m/s and E/A ratio of 1.6. Tiles C and D are tissue Doppler samplings of the lateral and medial mitral annulus representing normal values and an average E/e′ ratio of 9.9. The TR velocity (not pictured) showed an incomplete jet profile with peak velocity under 2 m/s. Given the absence of heart disease, using algorithm in Fig. 1, none of the criteria are met and the assessment of diastology in this patient would be normal.
Figure 5 presents a 62-year-old man with HOCM, hypertension, and hyperlipidemia who was being evaluated for septal myectomy. He has EF of 65% with septal hypertrophy Tile A is a pulsed-wave Doppler-signal depicting mitral inflow with an E/A ratio of 1.53. Tiles B and C show low tissue Doppler velocities with average E/e′ ratio of 20. Tiles D and F represent continuous wave TR velocity over 3 m/s. Tile E shows representative LAVi of 40 ml/m2. By Fig. 2 criteria, all 3 are met and the interpretation of diastology in this case would be grade II with elevated LAP.
Figure 6 is a 66-year-old man with past history of coronary bypass, hypertension, and type II diabetes who presents with angina with nausea and vomiting. He has an EF of 45% with wall motion abnormalities. Tile A represents LAVi of 25 ml/m2 which is normal. Tile B is pulsed-wave Doppler of mitral inflow shows E velocity of 1 m/s and E/A ratio of 1.15. Tiles C and D represent tissue Doppler velocities of the medial and lateral mitral annulus, depicting low velocities and an average E/e′ ratio of 13.5. Tile E represents a TR velocity of 2.5 m/s with incomplete jet envelope. Based on Table 2, despite an E/A ratio >1, the diastolic function of this case would be grade I with normal LAP, as the 3 evaluation criteria are negative.
Changes in diastolic function with age
Normal individuals demonstrate a rapidly accelerating E wave, rapid deceleration, and an A wave significantly smaller than the E wave as previously mentioned. With normal LV compliance, the mitral deceleration time (DT) is typically between 160 and 240 ms with an IVRT 70–90 ms. With normal aging, there is slowing of LV relaxation with gradual decrease in peak E velocity, and concurrent increase in peak A wave velocity. In most patients, E and A waves become equal in the 6th decade of life with E/A ratio <1 in the 7th decade onwards [53]. There is also a progressive increase in E/e′ with age, and although men generally have a lower baseline E/e′ values compared to women, the progression is similar. Current data suggest that cutoff values for E/e′ should be age-adjusted, but more research is needed to assess the correlation with elevated LV filling pressures. As always, it is important to correlate the echocardiographic data with clinical symptoms prior to implementing diastolic function algorithms [54].
Conclusions
The assessment of diastolic function has significant prognostic value, however, was previously difficult to implement with many confounding variables. The most recent ASE/EACVI guidelines have simplified the algorithm to 3 parameters to allow echocardiographers to efficiently assess diastolic function. The guidelines are easy to use and apply to the vast majority of cases. Emerging data around new technologies such as GLS provide an exciting new direction in the assessment of diastolic function yet has an undetermined role at present and should be studied further. The newest ASE/ESC guidelines should be implemented in all echocardiography labs and clinical practice.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mozaffarian D et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2015;133:e38–360.
Heidenreich PA et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–19.
Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, et al. Roger VL Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–16.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–33.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29 Suppl 4:277–314. This is the updated guidelines document released in April 2016 and is the single most important document outlined in this review that simplifies the assessment of diastolic function.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39. This document is the precursor to changes the recommendations to chamber quantification. The indexed LA volume cutoff of 34 ml/m2 is incorporated into the new updated guidelines.
Schirmer H, Lunde P, Rasmussen K. Mitral flow derived Doppler indices of left ventricular diastolic function in a general population - the Tromso study. Eur Heart J. 2000;21:1376–86.
Caballero L, Kou S, Dulgheru R, Gonjilashvili N, Athanassopoulos GD, Barone D, et al. Echocardiographic reference ranges for normal cardiac Doppler data: results from the NORRE Study. Eur Heart J Cardiovasc Imaging. 2015;16:1031–41.
EchoNoRMAL (Echocardiographic Normal Ranges Meta-Analysis of the Left Heart) Collaboration. Ethnic-specific normative reference values for echocardiographic LA and LV size, LV mass, and systolic function: the EchoNoRMAL study. JACC Cardiovasc Imaging. 2015;8:656–65.
Nikitin NP, Witte KK, Thackray SD, de Silva R, Clark AL, Cleland JG. Longitudinal ventricular function: normal values of atrioventricular annular and myocardial velocities measured with quantitative two-dimensional color Doppler tissue imaging. J Am Soc Echocardiogr. 2003;16:906–21.
De Sutter J, De Backer J, Van de Veire N, Velghe A, De Buyzere M, Gillebert TC. Effects of age, gender, and left ventricular mass on septal mitral annulus velocity (E′) and the ratio of transmitral early peak velocity to E′ (E/E′). Am J Cardiol. 2005;95:1020–3.
Tighe DA, Vinch CS, Hill JC, Meyer TE, Goldberg RJ, Aurigemma GP. Influence of age on assessment of diastolic function by Doppler tissue imaging. Am J Cardiol. 2003;91:254–7.
Yamada H, Oki T, Mishiro Y, Tabata T, Abe M, Onose Y, et al. Effect of aging on diastolic left ventricular myocardial velocities measured by pulsed tissue Doppler imaging in healthy subjects. J Am Soc Echocardiogr. 1999;12:574–81.
Munagala VK, Jacobsen SJ, Mahoney DW, Rodeheffer RJ, Bailey KR, Redfield MM. Association of newer diastolic function parameters with age in healthy subjects: a population-based study. J Am Soc Echocardiogr. 2003;16:1049–56.
Dalen H, Thorstensen A, Vatten LJ, Aase SA, Stoylen A. Reference values and distribution of conventional echocardiographic Doppler measures and longitudinal tissue Doppler velocities in a population free from cardiovascular disease. Circ Cardiovasc Imaging. 2010;3:614–22.
Arbab-Zadeh A, Dijk E, Prasad A, Fu Q, Torres P, Zhang R, et al. Effect of aging and physical activity on left ventricular compliance. Circulation. 2004;110:1799–805.
Yamakado T, Takagi E, Okubo S, Imanaka-Yoshida K, Tarumi T, Nakamura M, et al. Effects of aging on left ventricular relaxation in humans - analysis of left ventricular isovolumic pressure decay. Circulation. 1997;95:917–23.
Rietzschel ER, De Buyzere ML, Bekaert S, Segers P, De Bacquer D, Cooman L, et al. Rationale, design, methods and baseline characteristics of the Asklepios study. Eur J Cardiovasc Prev Rehabil. 2007;14:179–91.
Nagueh SF, Lakkis NM, Middleton KJ, Spencer III WH, Zoghbi WA, Quinones MA. Doppler estimation of left ventricular filling pressures in patients with hypertrophic cardiomyopathy. Circulation. 1999;99:254–61.
McMahon CJ, Nagueh SF, Pignatelli RH, Denfield SW, Dreyer WJ, Price JF, et al. Characterization of left ventricular diastolic function by tissue Doppler imaging and clinical status in children with hypertrophic cardiomyopathy. Circulation. 2004;109:1756–62.
Geske JB, Sorajja P, Nishimura RA, Ommen SR. The relationship of left atrial volume and left atrial pressure in patients with hypertrophic cardiomyopathy: an echocardiographic and cardiac catheterization study. J Am Soc Echocardiogr. 2009;22:961–6.
Biagini E, Spirito P, Rocchi G, Ferlito M, Rosmini S, Lai F, et al. Prognostic implications of the Doppler restrictive filling pattern in hypertrophic cardiomyopathy. Am J Cardiol. 2009;104:1727–31.
Appleton CP, Hatle LK, Popp RL. Demonstration of restrictive ventricular physiology by Doppler echocardiography. J Am Coll Cardiol. 1988;11:757–68.
Cohen GI, Pietrolungo JF, Thomas JD, Klein AL. A practical guide to assessment of ventricular diastolic function using Doppler echocardiography. J Am Coll Cardiol. 1996;27:1753–60.
Koyama J, Ray-Sequin PA, Falk RH. Longitudinal myocardial function assessed by tissue velocity, strain, and strain rate tissue Doppler echocardiography in patients with al (primary) cardiac amyloidosis. Circulation. 2003;107:2446–52.
Sallach JA, Klein AL. Tissue Doppler imaging in the evaluation of patients with cardiac amyloidosis. Curr Opin Cardiol. 2004;19:464–71.
Choi JH, Choi JO, Ryu DR, Lee SC, Park SW, Choe YH, et al. Mitral and tricuspid annular velocities in constrictive pericarditis and restrictive cardiomyopathy: correlation with pericardial thickness on computed tomography. JACC Cardiovasc Imaging. 2011;4:567–75.
Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002;90:1284–9.
Seward JB, Casaclang-Verzosa G. Infiltrative cardiovascular diseases: cardiomyopathies that look alike. J Am Coll Cardiol. 2010;55:1769–79.
Diwan A, McCulloch M, Lawrie GM, Reardon MJ, Nagueh SF. Doppler estimation of left ventricular filling pressures in patients with mitral valve disease. Circulation. 2005;111:3281–9.
Kusunose K, Yamada H, Nishio S, Tomita N, Hotchi J, Bando M, et al. Index-beat assessment of left ventricular systolic and diastolic function during atrial fibrillation using myocardial strain and strain rate. J Am Soc Echocardiogr. 2012;25:953–9.
Soeki T, Fukuda N, Shinohara H, Sakabe K, Onose Y, Sawada Y, et al. Mitral inflow and mitral annular motion velocities in patients with mitral annular calcification: evaluation by pulsed Doppler echocardiography and pulsed Doppler tissue imaging. Eur J Echocardiogr. 2002;3:128–34.
Nagueh SF, Kopelen HA, Quiñones MA. Assessment of left ventricular filling pressures by Doppler in the presence of atrial fibrillation. Circulation. 1996;94:2138–45.
Temporelli PL, Scapellato F, Corrà U, Eleuteri E, Imparato A, Giannuzzi P. Estimation of pulmonary wedge pressure by transmitral Doppler in patients with chronic heart failure and atrial fibrillation. Am J Cardiol. 1999;83:724–7.
Chirillo F, Brunazzi MC, Barbiero M, Giavarina D, Pasqualini M, Franceschini-Grisolia E, et al. Estimating mean pulmonary wedge pressure in patients with chronic atrial fibrillation from transthoracic Doppler indexes of mitral and pulmonary venous flow velocity. J Am Coll Cardiol. 1997;30:19–26.
Kusunose K, Yamada H, Nishio S, Tamai R, Niki T, Yamaguchi K, et al. Interval from the onset of transmitral flow to annular velocity is a marker of LV filling pressure. JACC Cardiovasc Imaging. 2013;6:528–30.
Rivas-Gotz C, Khoury DS, Manolios M, Rao L, Kopelen HA, Nagueh SF. Time interval between onset of mitral inflow and onset of early diastolic velocity by tissue Doppler: a novel index of left ventricular relaxation: experimental studies and clinical application. J Am Coll Cardiol. 2003;42:1463–70.
Appleton CP. Influence of incremental changes in heart rate on mitral flow velocity: assessment in lightly sedated, conscious dogs. J Am Coll Cardiol. 1991;17:227–36.
Tops LF, Schalij MJ, Holman ER, van Erven L, van der Wall EE, Bax JJ. Right ventricular pacing can induce ventricular dyssynchrony in patients with atrial fibrillation after atrioventricular node ablation. J Am Coll Cardiol. 2006;48:1642–8.
D’Souza KA, Mooney DJ, Russell AE, MacIsaac AI, Aylward PE, Prior DL. Abnormal septal motion affects early diastolic velocities at the septal and lateral mitral annulus, and impacts on estimation of the pulmonary capillary wedge pressure. J Am Soc Echocardiogr. 2005;18:445–53.
Nagueh SF, Bhatt R, Vivo RP, Krim SR, Sarvari SI, Russell K, et al. Echocardiographic evaluation of hemodynamics in patients with decompensated systolic heart failure. Circ Cardiovasc Imaging. 2011;4:220–7.
Kosmala W, Jellis C, Marwick TH. Exercise limitation associated with asymptomatic left ventricular impairment: analogy with stage B heart failure. J Am Coll Cardiol. 2015;65:257–66.
Nagueh SF, Sun H, Kopelen HA, Middleton KJ, Khoury DS. Hemodynamic determinants of the mitral annulus diastolic velocities by tissue Doppler. J Am Coll Cardiol. 2001;37:278–85.
Burgess MI, Jenkins C, Sharman JE, Marwick TH. Diastolic stress echocardiography: hemodynamic validation and clinical significance of estimation of ventricular filling pressure with exercise. J Am Coll Cardiol. 2006;47:1891–900.
Ritzema JL, Richards AM, Crozier IG, Frampton CF, Melton IC, Doughty RN, et al. Serial Doppler echocardiography and tissue Doppler imaging in the detection of elevated directly measured left atrial pressure in ambulant subjects with chronic heart failure. JACC Cardiovasc Imaging. 2011;4:927–34.
Talreja DR, Nishimura RA, Oh JK. Estimation of left ventricular filling pressure with exercise by Doppler echocardiography in patients with normal systolic function: a simultaneous echocardiographic-cardiac catheterization study. J Am Soc Echocardiogr. 2007;20:477–9.
Holland DJ, Prasad SB, Marwick TH. Prognostic implications of left ventricular filling pressure with exercise. Circ Cardiovasc Imaging. 2010;3:149–56.
Wang J, Khoury DS, Thohan V, Torre-Amione G, Nagueh SF. Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation. 2007;115:1376–83.
Dokainish H, Sengupta R, Pillai M, Bobek J, Lakkis N. Usefulness of new diastolic strain and strain rate indexes for the estimation of left ventricular filling pressure. Am J Cardiol. 2008;101:1504–9.
Notomi Y, Lysyansky P, Setser RM, Shiota T, Popovic ZB, Martin-Miklovic MG, et al. Measurement of ventricular torsion by two-dimensional ultrasound speckle tracking imaging. J Am Coll Cardiol. 2005;45:2034–41.
Notomi Y, Popovic ZB, Yamada H, Wallick DW, Martin MG, Oryszak SJ, et al. Ventricular untwisting: a temporal link between ventricular relaxation and suction. Am J Physiol Heart Circ Physiol. 2008;294:H505–13.
Nappo R, Degiovanni A, Bolzani V, Sartori C, Di Giovine G, Cerini P, et al. Quantitative assessment of atrial conduit function: a new index of diastolic dysfunction. Clin Res Cardiol. 2016;105:17–28.
Plana JC, Klein A. Assessment of diastolic function by echocardiography. In: Desai MY, editor. The practice of clinical echocardiography, 4th edn. Philadelphia: Elsievier; 2012. p. 197–217. Print.
Carvalho JC et al. Effect of age and sex on echocardiographic left ventricular diastolic function parameters in patients with preserved ejection fraction and normal valvular function. Cardiol J. 2013;20(5):513–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
KDP, PC, and AK declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Echocardiography
Rights and permissions
About this article
Cite this article
Patel, K.D., Collier, P. & Klein, A.L. Modern Assessment of Diastolic Function. Curr Cardiovasc Imaging Rep 9, 28 (2016). https://doi.org/10.1007/s12410-016-9388-7
Published:
DOI: https://doi.org/10.1007/s12410-016-9388-7