Abstract
Background
Data registries facilitate knowledge acquisition and quality improvement. ImageGuide is a registry developed by the American Society of Nuclear Cardiology collecting data since 2015, providing insight into current nuclear cardiology practice.
Methods and Results
HIPAA de-identified data on > 100 practice- and patient-related variables from 19 US practices were obtained from ImageGuide. Continuous variables are reported as the mean ± standard deviation; discrete variables are reported as N (%). Practices were from 12 states; 9520 studies were submitted. The average patient was a 66-year-old man. Chest pain was the most common indication; 96% of studies were appropriate. Rest/stress 1-day studies were most common; stress/rest 1- and 2-day studies comprised < 5%. Tc-99 m was the most common radiopharmaceutical. Tl-201 was used in 14% of rest studies. Most studies were not corrected for attenuation. 89% were of good or better quality. 62% of studies were normal.
Conclusions
Practice diversity is limited, but patient demographics are reflective of reported current practice. Most studies are appropriate and may obviate the need for invasive testing. Radiation dosimetry could be decreased with wider adoption of stress/rest studies and avoidance of Tl-201. ImageGuide will be an important tool to guide non-invasive cardiac imaging in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As an efficient tool in targeted data collection, registries enable analysis of both quality and outcomes related to disease states, processes, and therapeutic interventions. As healthcare costs increase, high value care has received greater attention,1 and appropriate use criteria (AUC) have been established for diagnostic testing and interventions. Cardiac registries are being used to assess compliance with AUC, the Medicare AUC mandate, and other guidelines, and to guide quality improvement. Payment is increasingly tied to participation in such quality improvement measures, largely driving growth in registry participation.
ImageGuide is a non-invasive cardiovascular imaging registry developed by members of the American Society of Nuclear Cardiology (ASNC). Its aims include facilitating documentation of performance metrics and adherence to best practices, maintenance of laboratory accreditation, participation in quality improvement, and investigation into patient outcomes.2,3,4,5 It is recognized as a qualified clinical data registry (QCDR) by the Centers for Medicare and Medicaid Services (CMS).6
Methods
Nuclear cardiology laboratories enrolled in ImageGuide on a rolling basis. Participating practice demographics were captured in the initial application, including practice size, location, accrediting agency and accreditation status, and submitting physician information; see Appendix A for a sample enrollment form. Patient- and test-related data were entered into ImageGuide via certified data reporting vendor, web-based interface, or direct link to the PACS imaging and reporting system following required legal documentation allowing for sharing of identified data. The registry shares data with investigators appropriate to the investigator’s hypotheses and IRB review. For the purpose of this study, patient-specific data from the registry were HIPAA de-identified and included baseline demographics, indication for study, appropriateness, study protocol and radiopharmaceutical used, and results. A full list of included variables is provided in a sample submission form, which can be found in Appendix B. Practices are required to report all studies and data are subject to random audit by ASNC staff to assure compliance and accuracy of data reporting. In 2018 this included 3% of the providers and 10% of the studies and all fields included in the MIPS performance measures. Data collection began in Quarter 1 of 2015 and continues to the present; data are reported as of Quarter 3 of 2018 (total of 15 quarters), having met a pre-determined evaluation point of 10,000 patient records. Continuous variables are reported as the mean ± standard deviation or median (interquartile-range), and discrete variables are reported as N (%). Reported radiation doses in ImageGuide were given in mCi; these values were multiplied by 37 to convert to MBq.
The Institutional Review Board of the Greenville Health System approved the study. As the data received from the registry contained no patient-identifiable information, informed consent was not required.
Results
Practice Demographics
As of data harvest in July 2018, there were 19 participating practices, together submitting data on 9520 patients.
Practices submitting data were from 12 different U.S. states (see Table 1 for location of participating practices; Table 2 presents additional practice demographics). Data were incomplete for many non-required fields. Most were clinic-based or independent imaging facilities and followed a for-profit business model. Single photon emission computed tomography (SPECT) was the most common imaging modality, followed by positron emission tomography (PET) and planar. Most laboratories had additional imaging capabilities, with echocardiography being the most commonly available modality. Eight companies were represented in the quantitative package used for image and data analysis.
Eleven laboratories reported accreditation by the Intersocietal Accreditation Commission (IAC), with four receiving accreditation from the American College of Radiology (ACR). One of these reported accreditation from both organizations. Physicians were certified most commonly by the Certification Board in Nuclear Cardiology, followed by the American Board of Nuclear Medicine. Six physicians reported dual certifications.
Patient Demographics
Table 3 presents patient demographic data. The average age was 66, and patients were predominantly male. Data on race/ethnicity and insurance provider were limited due to incomplete reporting in these fields.
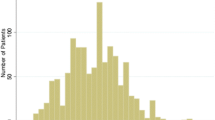
The primary indication was given in 99.8% of studies (Figure 1). Pretest chest pain is classified in 2754 patients (28.93%), not necessarily those for whom chest pain was given as the primary or secondary indication for testing; of these patients, no chest pain was reported in 46.91% and atypical angina in 27.78%. Non-anginal chest pain, typical angina, and angina equivalent were less commonly reported, in 9.37%, 8.24%, and 7.70%, respectively.
Most studies (96.08%) were reported as appropriate; a small proportion of studies (3.13%) were reported as may be appropriate and few (0.59%) as rarely appropriate.
Imaging Characteristics
Details on testing protocols are given in Table 4. The stressor was pharmacologic in most studies, followed by exercise and less commonly by combined exercise/pharmacologic stress. Of the pharmacologic agents, regadenoson was most commonly used, followed by adenosine and dipyridamole; dobutamine with or without atropine was rarely used. The Bruce protocol was the most commonly employed exercise protocol. Rest/stress 1-day was by far the most common imaging protocol.
Technetium-99 m (Tc-99 m) based radiopharmaceuticals were the most common agents employed in SPECT stress imaging; thallium-201 (Tl-201) was used rarely. Among PET radioisotopes, Rubidium-82 (Rb-82) was most commonly used.
In rest imaging, Tc-99 m sestamibi was again most commonly used, followed by Rb-82 and Tc-99 m tetrofosmin. Notably, Tl-201 was used in over 14% of rest studies.
2,511 studies (26.78% were corrected for attenuation. Of these, transmission was used in 81.60%, CT in 4.50%, and other methods (including supine or prone) in 13.90%.
Hemodynamic data for rest,exercise and pharmacologic stress are presented in Table 5. Anginal stress symptoms were reported in 3415 patients (35.87%), not necessarily those for whom chest pain was given as an indication for testing; of these, no chest pain was reported in 89.14%, typical angina in 2.11%, atypical angina in 5.59%, anginal equivalent in 2.72%, and non-anginal chest pain in 0.44%.
The reason for termination was reported in > 80% of studies. The majority of studies were terminated due to reaching the end of the protocol. Figure 2 provides a full list of reported reasons and their frequencies.
The self-reported study quality was excellent or good in most studies, with few reported as poor or other quality (Figure 3).
The left ventricular perfusion summary was given for approximately 94% of studies (Figure 4); over 66% of studies were reported as normal or probably normal, with a smaller proportion of studies showing ischemia. Transient ischemic dilation was noted in 15.80% of studies. Studies were rarely reported as uninterpretable, correlating with the study quality data reported in Figure 3.
Discussion
This study examined data gathered from the initial 10,000 records/three years of the ImageGuide Registry, a first-of-its-kind registry that affords a unique look at nuclear cardiology practice in the United States today. As there are essentially two major data subsets contained in the whole, we will discuss them separately.
Practice Demographics
Representative laboratories were geographically diverse, with participating practices from the Northeast, Southeast, Midwest, and West. Practice demographics are notable for a high proportion of clinic-based and independent imaging facilities with only one hospital-based practice, in contrast to a higher percentage seen in prior studies.7,8,9 Several possible explanations may account for this. Our study included a small number of practices (19, compared with hundreds in the cited studies), increasing the probability of random sampling error. Additionally, hospital-owned practices often have more administrative hurdles to overcome in adopting new protocols and procedures, which may delay enrollment in the registry for this demographic. The lower proportion of hospital-owned practices may also explain the higher proportion of labs with accreditation in our study compared with prior studies, as hospital systems may not have strict requirements for maintaining accreditation for the purposes of reimbursement.
Patient and Imaging Data
Given the limited practice sample size, it is important to consider the quality of patient-level data in assessing the generalizability of these results. Patient demographics, in particular average age, sex distribution, and BMI are similar to those seen in prior studies.10,11 Not all data elements are required on the submission form, and demographic data reporting for non-required fields ranged from 100% for sex to 2.54% for insurance status. This is likely attributable to the methodology used to collect the early data in the registry; most of the included sites manually input the data, which may result in the omission of many non-required fields. As more sites utilize data reporting through direct harvesting from the report or a certified vendor, the data set is expected to become more robust.
There has been much discussion in recent years as MPI has expanded in availability and technological power, with increased utilization leading to increased costs and radiation burden.7,12,13,14,15,16 AUC were developed to guard against overutilization, and assessing adherence to these helps us gauge how consistently we deliver indicated testing.
The vast majority of MPI studies were deemed appropriate. This is in contrast to prior studies which showed inappropriate ordering of tests in the 3–45% range.11 Notably, whereas prior studies used algorithms and computer-based logic to assign an indication and determine appropriateness, appropriateness was self-reported by the participating practices in ImageGuide, allowing for greater possibility of bias. As a Qualified Clinical Data Registry by CMS, ImageGuide staff perform a manual audit of selected patient records to confirm accuracy of data reporting. During a recent audit there was 98.11% agreement between medical record documentation and data reported in the registry (Lattoz, Daniel, ASNC Staff, unpublished data, 2019). Also of note, AUC were laboratory-selected and are not reported in the registry. As there has been significant change in AUC and its impact, including the upcoming Congressional mandate for use of decision support tools, the appropriateness of studies could have evolved. This discrepancy between published trial data and the registry data regarding AUC warrants further investigation regarding current AUC results in practice.
The data on MPI results were notable for a sizeable percentage showing normal left ventricular perfusion. Given the high percentage of reportedly appropriate tests, this speaks to the high value of MPI, as the number of patients for whom the need for invasive testing was obviated by a normal perfusion study is likely quite large.
A high proportion of tests were reported as being of good or excellent quality, with a low percentage of tests having an uninterpretable left ventricular perfusion study. However, it is interesting to note that over half of all studies did not utilize attenuation correction. It has previously been recommended in joint position statements by the ASNC and Society of Nuclear Medicine and Molecular Imaging that attenuation correction be utilized when feasible, increasing the accuracy, prognostic value, and efficiency of perfusion imaging.17,18 Wider adoption of attenuation correction thus represents another area for ongoing improvement.
As with all tests utilizing ionizing radiation, the As Low As Reasonably Achievable (ALARA) principle is important with respect to test protocol, appropriate patient selection, isotope utilization and dosimetry. Einstein et al.13 have suggested four goals to reduce radiation exposure to patients; two of these can be examined further through this data: (1) wider adoption of stress-first imaging, which in appropriately selected patients could obviate the need for rest imaging if stress perfusion is normal, and (2) greater adherence to AUC in clinical practice. As to the latter, we do see a higher (reported) adherence to AUC compared to prior studies. As to the former, the authors found in their survey of nuclear cardiologists a 7.2% rate of stress-only imaging protocol utilization, which they identified as a “missed opportunity” for reducing radiation exposure for a greater percentage of patients. In ImageGuide, rates of stress-only studies are even lower: < 2% in the current data analysis. When stress/rest 1- and 2-day studies are included, as a normal perfusion in the stress portion could potentially allow the physician to cancel the second part of the protocol, this number rises to 6.54%, still lower than previously reported.
Also pertinent is the use of thallium-201 based protocols. In a study of the IAC data repository the highest average and maximum radiation effective doses were associated with Tl-201 and Tl-201/Tc-99 m dual isotope studies, which together constituted 9.1% of studies.7 Reduced reliance on Tl-201 based protocols has thus been identified as a target for reduction in radiation exposure. A symposium in 2012 identified procedures exposing patients to > 20 mSv as a target for increased scrutiny with regards to appropriateness;14 a majority of both dual- and single-isotope Tl-201 based protocols were associated with radiation doses above this threshold in the IAC study.
In our study, we identified that Tl-201 is still being used frequently in dual isotope protocols. The proportion we identified is higher than previously reported, nearly 14%; sampling error may well affect both studies: in the case of the IAC study, due to the small number of patients sampled from each practice, and in the present study, due to the small number of participating practices; regardless, decreasing usage of Tl-201 continues to be an area of concern in patient safety.
It is worth noting as well that SPECT outnumbers PET roughly 4:1 in the total number of study protocols performed; it has yet to be seen if the latter, which is associated with a lower radiation exposure burden, will outstrip the former modality in years to come, though certainly there are still significant logistical barriers to more widespread availability of PET-MPI.
Strengths of this study include its large and unselected patient population, the latter of which is an advantage the IAC repository study and International Atomic Energy Agency (IAEA) Nuclear Cardiology Protocols Study (INCAPS) lacked, despite their large practice sample sizes.7,16 Whereas the IAC repository featured data on 3–5 index patient cases per practice per accreditation period, and the INCAPS assessed samples of consecutive patients over a one-week period of each practice’s choice, practices participating in ImageGuide are required to report all studies.
Notable limitations include the small practice sample size. The steering committee for ImageGuide has previously expressed, however, that initial participating laboratories were to be intentionally selected so as to be representative of the greater community.4 As such, very large practices have not been included in the early phase of the registry, so as not to overwhelm the data set while the overall numbers are still small, and participating practices represent a variety of practice types and geographic locations. With more laboratories having already enrolled and many more in process, the future promises an increasingly robust data set, which will increase the statistical power and generalizability of later studies.
A more thorough treatment of the topic of radiation exposure would include effective radiation dose in milliseverts (mSv). Though this would be a pertinent area for future research, dose conversions to mSv is beyond the scope of the current study.
ImageGuide’s designation as a QCDR will likely encourage continued growth in registry participation, as it provides an avenue for fulfilling MIPS requirements for obtaining full CMS reimbursement. As more practices join, the diversity of practice type and size should also grow. It is unclear to what degree patient demographics and imaging details may differ in larger laboratories from those seen in the smaller practices participating in this early phase of the registry; this could be another interesting area for future study. Additional future efforts include the ability to provide practices ongoing feedback in addition to the MIPS data reports currently available. The potential for including images in the future will also expand the potential for evaluating image quality and accuracy of interpretation as the registry matures. Finally, as the registry grows, the data set is expected to become more representative of practice nationally.
New Knowledge Gained
A higher than previously reported rate of appropriate studies was seen in our study. Targets for future quality improvement emerge, including reduction of radiation exposure with protocol modification and greater utilization of attenuation correction.
Conclusion
The ImageGuide registry, while young, already provides valuable insights into the current state of nuclear cardiology practice in the United States. These early data indicate an encouraging level of adherence to AUC and also identify several areas for ongoing work in quality improvement. As the registry grows to include more practices and patients, the data contained therein will continue to increase in value for future study, affording opportunity to direct policies affecting the practice of nuclear cardiology as a whole.
Abbreviations
- AUC:
-
Appropriate use criteria
- QCDR:
-
Qualified clinical data registry
- CMS:
-
Centers for Medicare and Medicaid Services
- IAC:
-
Intersocietal Accreditation Commission
- MPI:
-
Myocrdial perfusion imaging
- ALARA:
-
As low as reasonably achievable
- INCAPS:
-
International Atomic Energy Agency (IAEA) Nuclear Cardiology Protocols Study
References
Levinson W, Kallewaard M, Bhatia RS, Wolfson D, Shortt S, Kerr EA et al. A growing international campaign. BMJ Qual Saf 2015;24:167-74. https://doi.org/10.1136/bmjqs-2014-003821
Shaw LJ, Wang TY, Mahmarian JJ, Tilkemeier PL, Douglas PS, Arrighi JA et al. Registry. J Nucl Cardiol 2013;20:655-56. https://doi.org/10.1007/s12350-013-9743-x.
Williams KA, McKinley AP, for the Executive Council of ASNC. How the ASNC ImageGuide Registry will guide healthcare policy. J Nucl Cardiol 2013;20:948-50. https://doi.org/10.1007/s12350-013-9770-7.
Tilkemeier P, Wang TY, Lytle BL, Denton EA, for the Executive Council of the ASNC. ImageGuideTM: Cardiovascular imaging data registry. J Nucl Cardiol 2013;20:1186-87. https://doi.org/10.1007/s12350-013-9789-9.
Tilkemeier PL, Mahmarian JJ, Wolinsky DG, Denton EA. ImageGuideTM update. J Nucl Cardiol 2015;22:994-97. https://doi.org/10.1007/s12350-015-0217-1.
Tilkemeier PL, Doukky R, Kirkpatrick JN, Desai MY, Nagueh SF. Coming-of-age: The ImageGuideTM Registry at three. J Nucl Cardiol 2019;26:72-5. https://doi.org/10.1007/s12350-018-1442-1.
Jerome SD, Tilkemeier PL, Farrell MB, Shaw LJ. Nationwide laboratory adherence to myocardial perfusion imaging radiation dose reduction practices. J Am Coll Cardiol 2015;8:1170-76. https://doi.org/10.1016/j.jcmg.2015.07.008.
Maddux PT, Farrell MB, Ewing JA, Tilkemeier PL. Improved compliance with reporting standards: A retrospective analysis of Intersocietal Accreditation Commision nuclear cardiology laboratories. J Nucl Cardiol 2018;25:986-94. https://doi.org/10.1007/s12350-016-0713-y.
Maddux PT, Farrell MB, Ewing JA, Tilkemeier PL. Improving compliance with Intersocietal Accreditation Commission (IAC) reporting standards: A serial comparison of 523 labs over seven years. J Nucl Cardiol 2018;25:2044-52. https://doi.org/10.1007/s12350-017-0904-1.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2013;107:2900-07. https://doi.org/10.1161/01.CIR.0000072790.23090.41.
Ladapo JA, Blecker S, O'Donnell M, Jumkhawala SA, Douglas PS. Appropriate use of cardiac stress testing with imaging: A systematic review and meta-analysis. PLoS ONE 2016;11:e0161153. https://doi.org/10.1371/journal.pone.0161153.
de Gonzalez A, Kim KP, Smith-Bindman R, McAreavey D. Myocardial perfusion scans: Projected population cancer risks from current levels of use in the United States. Circulation 2011;123:2403-10. https://doi.org/10.1161/CIRCULATIONAHA.110.941625.
Einstein AJ, Tilkemeier PL, Fazel R, Rakotoarivelo H, Shaw LJ, for the American Society of Nuclear Cardiology. Radiation safety in nuclear cardiology—current knowledge and practice: Results from the 2011 American Society of Nuclear Cardiology member survey. JAMA Intern Med 2013;173:1021-23. https://doi.org/10.1001/jamainternmed.2013.483
Einstein AJ, Berman DS, Min JK, Hendel RC, Gerber TC, Carr JJ et al. Patient-centered imaging: Shared decision making for cardiac imaging procedures with exposure to ionizing radiation. J Am Coll Cardiol 2014;63:1480-89. https://doi.org/10.1016/j.jacc.2013.10.092.
Mercuri M, Pascual TNB, Mahmarian JJ, Shaw LJ, Dondi M, Paez D et al. Estimating the reduction in the radiation burden from nuclear cardiology through use of stress-only imaging in the United States and worldwide. JAMA Intern Med 2016;176:269-73. https://doi.org/10.1001/jamainternmed.2015.7106.
Bouyoucef SE, Mercuri M, Pascual TN, Allam AH, Vangu M, Vitola JV et al. Nuclear cardiology practices and radiation exposure in Africa: Results from the IAEA Nuclear Cardiology Protocols Study (INCAPS). Cardiovasc J Afr 2017;28:229-34. https://doi.org/10.5830/CVJA-2016-091.
Hendel RC, Corbett JR, Cullom SJ, DePuey EG, Garcia EV, Bateman TM. The value and practice of attenuation correction for myocardial perfusion SPECT imaging: A joint position statement from the American Society of Nuclear Cardiology and the Society of Nuclear Medicine. J Nucl Cardiol 2002;9:135-43.
Heller GV, Links J, Bateman TM, Ziffer JA, Ficaro E, Cohen MC et al. American Society of Nuclear Cardiology and Society of Nuclear Medicine joint position statement: Attenuation correction of myocardial perfusion SPECT scintigraphy. J Nucl Cardiol 2004;11:229-30. https://doi.org/10.1016/j.nuclcard.2003.12.001.
Disclosures
Dr. Elder, Dr. Tilkemeier, and Dr. Ewing have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
All editorial decisions for this article, including selection of reviewers and the final decision, were made by guest editor Randall Thompson, MD.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elder, J.B., Tilkemeier, P.L. & Ewing, J.A. Insights into Nuclear Cardiology in the United States from the first 3 years of the ImageGuide Registry. J. Nucl. Cardiol. 29, 166–176 (2022). https://doi.org/10.1007/s12350-020-02112-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02112-5