Abstract
Background
Limited data address the roles of gender, perfusion defect reversibility, and imaging position in interpretation of images acquired on an upright/supine cadmium-zinc-telluride (CZT) cardiac imaging system.
Methods and Results
From a consecutive cohort of patients imaged on an upright/supine CZT camera, 260 patients with coronary angiograms were studied. Multivariable models identified gender as a significant effect modifier for imaging variables of CAD. For males, a supine summed stress score (SSS) ≥ 3 provided high accuracy (sensitivity 70.7%, specificity 72.2%), and highest contribution to multivariable models. In females, supine SSS ≥ 2 provided the best cut-off for defect size and severity (sensitivity 90%, specificity 35.9%), but specificity was improved substantially to 53.3% with decrease in sensitivity to 80% by also requiring quantitative identification of perfusion defect reversibility in the supine position. Eight variables, accurate for predicting coronary disease, were more accurate with supine than upright imaging.
Conclusions
Perfusion defect reversibility improved specificity in female patients for detection of coronary disease compared to perfusion defect size and extent alone. Supine images provided superior accuracy for detection of coronary disease compared to upright images.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cadmium-zinc-telluride (CZT) technology provides a combination of improved cardiac image resolution with substantially reduced imaging duration and/or radiotracer dose. Although large studies have evaluated the diagnostic accuracy for detection of coronary artery disease (CAD) using a CZT camera designed for supine and prone imaging,1,2 the published literature to guide the interpretation of upright/supine cardiac image sequences acquired with a CZT camera is more limited.3,4,5,–6 The existing upright/supine CZT camera literature focuses on total perfusion defect size and severity (i.e. summed stress score [SSS]), but variously excluded patients with prior myocardial infarction,3,4 prior coronary revascularization,3,4 cardiomyopathy,3,5 valvular heart disease,3 left bundle branch block or pacemakers,5 and non-obese patients,6 or excluded consideration of comparison resting images.4 We hypothesized that, in consecutive subjects referred for stress myocardial perfusion imaging (MPI), who also underwent coronary angiography, different diagnostic criteria might be necessary to maximize overall test accuracy, provide guidance to selectively increase test sensitivity, and identify new criteria that are gender specific.
Methods
Study Population
The study was approved by the Institutional Review Board of the University of Cincinnati as a retrospective review and was exempt from informed consent.
Between June 20th, 2014 and June 19th, 2015, 1889 patients underwent exercise or pharmacologic (regadenoson) single-photon emission computerized tomography (SPECT) MPI in the University of Cincinnati Exercise Laboratory. From this cohort, 260 patients who completed both upright and supine stress and rest images and underwent coronary angiography within 3 months of the stress MPI were consecutively included in the present study, regardless of the past history.
Myocardial Perfusion SPECT Imaging
Patients were instructed not to use caffeinated beverages or foods for 24 hours prior to testing. Beta-blockers and calcium channel antagonists were routinely withheld for 24 to 48 hours prior to testing, unless approval was denied by the referring physician. Stress imaging was performed on a treadmill by the Bruce protocol or using pharmacological stress with regadenoson 0.4 mg intravenously, with adjunctive exercise where possible.
Upright and supine stress and rest images were acquired on a D-SPECT CZT dedicated cardiac camera (Spectrum Dynamics Inc., Palo Alto, CA). Upright imaging was performed with the imaging chair at a 65°-70° angle. Rest images were acquired for 3-11 minutes at 60 minutes following weight-based injection of 9.4-14 mCi of technetium-99m tetrofosmin. Stress images were acquired for at least 3 minutes at 30-45 minutes following weight-based injection of 27.7-42 mCi of technetium-99m tetrofosmin.
SPECT images were processed with iterative reconstruction (ordered subset expectation maximization) on a Spectrum Dynamics Cedars View processing station. Interpretation of the images was accomplished with Corridor4DM SPECT software (INVIA Medical Imaging Solutions, Ann Arbor, MI), by two experienced physicians, independently and in blinded fashion, without knowledge of test indication or patients’ clinical data, except gender, height and weight. Each of the 17 cardiac segments at stress and rest, in each imaging position, was interpreted on a scale from 0 (normal) to 4 (absent myocardial activity) as previously reported from our laboratory.7 Close attention was provided in positioning the base and apex limits to assure the congruence of stress and rest limits. Summed stress score (SSS), summed rest score (SRS), and summed difference score (SDS) were recorded from upright and supine positions, and average SSS was calculated from the average of the upright and supine stress images. Upright and supine transient ischemic dilation (TID) ratios and rest and post-stress left ventricular ejection fraction (LVEF) were calculated from the gated images by the 4DM SPECT software. In addition, for both the upright and supine positions, quantitative percent stress and rest regional perfusion defect sizes were calculated for the left anterior descending, left circumflex, and right coronary artery territories. Any pixel value in the left ventricle that was more than or equal to 2 standard deviations below the mean value for the normal population was considered abnormal.7 Summed stress percentage (SSP) (Figure 1) and summed rest percentage (SRP) were each calculated as the sum of the defect percentages in all three coronary artery territories. Summed change percentage (SCP) was calculated as the difference between SSP and SRP. Visual evidence of defect reversibility consisted of any decrease in defect severity or size by at least one grade, and was assessed for reversibility in either upright or supine position, in both upright and supine position, and for reversibility in either upright or supine position accompanied by a fixed defect in the other position. Total quantitative assessment of defect reversibility (QREV) for the entire left ventricle (Figure 1), including the border zones not assigned to a specific coronary artery, was assessed as any increase in total left ventricular defect percent at stress compared to rest, and, also, as any 5% or greater increase in reversibility from stress to rest. Due to the use of a different software in the present study, the combined SSS criterion in the present study did not precisely reproduce the previously published methods.3 In the present study, the combined criterion for SSS ≥ 3 in both upright and supine positions was not limited to abnormal pixels identified in the upright position and then confirmed in the supine position.
Quantitative variable Summed Stress Percentage (SSP) (blue rectangle) is the sum of the percent abnormality for the three coronary territories (in this illustration, SSP = 9). Image is taken from a male subject with supine summed stress score of 0 and < 5 in both positions, suggesting absence of CAD by previously published criteria. In the present analysis, the summed stress percentage ≥ 6 is abnormal and consistent with the finding of a 90% stenosis in the mid left anterior descending coronary artery in this patient. QREVS is the total quantitative change in defect reversibility (QREV) in the entire left ventricle in the supine position, calculated as total defect percent (yellow circle) at stress minus the total defect percent at rest. In this male patient QREVS is normal
Coronary Angiography
Coronary angiographic images were blinded for the patient’s age, gender, past medical history, presenting symptoms, and stress MPI results. Angiographic CAD was defined as a stenosis either ≥ 50% in the left main coronary artery or ≥ 70% in the left anterior descending, left circumflex, or right coronary artery, or a major branch. Angiographic CAD was assessed independently by one blinded reader and then compared with the un-blinded reading in the patient’s chart. Any differences were resolved independently by a second blinded reader.
Statistical Analysis
Continuous variables were described using mean and standard deviation (SD) while categorical data were described using frequency and proportion. All data were summarized for entire cohort and separately for each gender. Student’s t test was used to determine significant difference between samples for quantitative variables while Fisher’s exact test was used for categorical variables. The unadjusted logistic regression analysis was carried out to determine each considered clinical factor associated with angiographic CAD and the predictive performance of each variable was obtained using receiver operating characteristics curve (ROC) analysis. The multivariable logistic regression analysis was carried out to determine multiple predictors for angiographic CAD. Various predictive models were developed to predict CAD (a) Model 1: baseline predictors without using any imaging parameters (b) Model 2 & 3: baseline predictors plus nuclear test variables. The results of logistic regression analysis were summarized using odds ratio and 95% confidence interval (CI) and P value while predictive summary was measured using the area under the ROC curve. Furthermore, nuclear test variables at upright and supine positions were evaluated separately for predicting CAD using logistic regression models. The diagnostic performance of all considered nuclear tests (SSS, SRS, SDS, total quantitative reversibility, transient ischemic dilation, qualitative reversibility on each or combined positions) in relation to angiographic CAD was summarized using sensitivity and specificity by each gender separately for entire cohort and pharmacologic tests cohort only. Various final predictive models for CAD separately for each gender were developed and model performance was specified for an appropriate threshold maximizing sensitivity and specificity. Backward stepwise selection criteria with probability of removal with 15% cut-off of the predicted probability by the model was used for developing multivariable logistic regression. In addition, any variable which provided at least 2% increase in the area under the curve from the comparative nested model was added in the multivariable model. The important results were summarized with cluster bar diagram or ROC curves. All statistical analyses were carried out using STATA 15.1 (StataCorp, College Station, TX). P values less than 5% were regarded as statistically significant results.
Results
Demographic characteristics and representative nuclear variables for consecutive patients who completed myocardial perfusion imaging during the study period and had a subsequent coronary angiogram are shown in Table 1. Men had a higher average body mass index (BMI) (34.0 vs 30.7, P < .001), were less likely to have had coronary artery bypass surgery (3% vs 15%, P = .025), and had higher stress (59% vs 51%, P < .001) and rest (60% vs 52%, P < .001) LVEF compared to women. Other baseline characteristics, including pre-test likelihood of coronary artery disease,8 and nuclear variables were equally distributed between men and women. A pharmacologic stress test was performed in 73.9% of the patients. Significant angiographic CAD was present in 77 of the 260 study patients (29.6%, 95% CI 24%-36%), including 56 men and 21 women. In view of the small number of female patients (n = 6) who completed treadmill exercise to target heart rate and were found to have angiographic CAD, data are presented for the combined pharmacologic and exercise group and separately for patients tested with pharmacologic stress.
Unadjusted/univariate demographic predictors of angiographic CAD are presented in Table 2. Although both age and gender were predictive for the presence of angiographic coronary disease, the calculated pre-test likelihood of disease8 was not.
Nuclear test variables were analyzed to compare the predictability for angiographic CAD in the upright vs supine position. Eight of the variables most strongly associated with angiographic CAD all performed best when acquired in the supine rather than upright position (top of Table 3). This included the continuous variables SSS, SDS, SSP, SRP, SCP, supine LVEF, transient ischemic dilation, and the binary variable visual reversibility. Six additional binary variables were also predictive (bottom of Table 3), including total quantitative assessment of defect reversibility for the entire left ventricle in the supine position (QREVS), combined SSS,3 consensus of the two readers that a scan was normal vs abnormal, and visual reversibility criteria 1, 3, and 5. As a predictor of angiographic coronary disease, purely subjective detection of myocardial perfusion defect reversibility approached the level of quantitative identification of defect reversibility (data not shown), but was limited by inter-observer variability (kappa score for subjective identification of a reversible perfusion defect in either imaging position was 0.452). Quantitative variables describing defect size in individual coronary artery distributions were tested but were not among the most significant predictors
Adjusted, multivariable predictors of significant angiographic CAD were best identified by three models (Table 4). Model 1, without including any nuclear perfusion variables, identified age, BMI, male gender, history of CAD, history of percutaneous coronary intervention, history of coronary artery bypass surgery, and post-stress supine LVEF to be independently associated with CAD (AUC = 81%). Inclusion of nuclear perfusion variables in Model 2 yielded better predictive performance for CAD (AUC = 82%) and showed combined SSS, QREVS, along with male gender, history of CAD, PCI and body mass index ≥ 35 kg/m2 independently associated with the presence of CAD. Model 3 showed that replacing two nuclear variables with only supine SSS ≥ 3 in Model 2 produced the same predictive performance (AUC = 82%).
The only demographic variable from the multivariable analysis that altered impact of the nuclear variables on the detection of angiographic CAD was gender. Therefore, gender-specific analysis of nuclear variables was performed. Individual test performance separated by gender showed that, in general, specificity was lower for women as compared to men (Table 5). For male patients the highest level of combined sensitivity and specificity by perfusion imaging was achieved with either the combined SSS3 (sensitivity 69.0%, specificity 74.4%), supine SSS ≥ 3 (sensitivity 70.7%, specificity 72.2%), or supine SSP ≥ 6 (sensitivity 79.3%, specificity 53.3%). For female patients, high sensitivity of 90.0% was provided by supine SSS ≥ 2 with decline in specificity to 35.9% or by QREVS with sensitivity of 85.0%, but with low specificity of 34.8%. The performance of these nuclear tests (supine SSS, combined SSS, SSP and QREVS) remained the same and high in the pharmacologic only population as well.
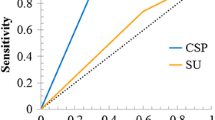
The highest performing multivariable models separated by gender for prediction of angiographic CAD are shown in Table 6. For male patients, the highest combination of sensitivity and specificity for detection of CAD was provided by Model 2 which included supine SSS ≥ 3, along with age ≥ 60 years and histories of PCI or CABG, and post-stress supine LVEF (AUC 83%).Two other indices of defect size and extent, combined SSS (Model 1: AUC = 82%) and SSP ≥ 9 (Models 1 and 3: AUC = 82 and 81%) along with age ≥ 60 years and histories of PCI and CABG were strong predictors for CAD. For female patients, combined SSS and quantitative defect reversibility along with history of CAD, history of cardiomyopathy, and BMI ≥ 35 Kg/m2 produced a high predictive accuracy for CAD (Model 1: AUC = 86%). Use of a supine SSS ≥ 2 along with histories of CAD, cardiomyopathy, and BMI ≥ 35 kg/m2 produced the highest predictive accuracy for CAD (Model 2: AUC = 87%). Predictive equation model 2, with probability of CAD ≥ 37%, yielded the highest sensitivity (82.5%) and specificity (71.9%) for males while predictive equation model 2 with probability of CAD ≥ 13% produced highest sensitivity (90%) and specificity (71.1%) for females (Table 6, Supplementary Figure 1). QREV did not improve accuracy of the model for male patients (Table 6, Figure 2), due to limited specificity. In contrast, QREVS was a significant predictor of CAD in female patients (Table 6, model 1, and Figure 3). In female patients, a supine SSS ≥ 2 provided the strongest imaging predictor of angiographic CAD. Figure 4 illustrates that for male patients, high accuracy was achieved with supine SSS ≥ 3, particularly in patients who had pharmacologic stress. Sensitivity for male patients for all tests could be improved to 79.3% with a SSP ≥ 6, but with a decline in specificity to 53.3%. Similarly, QREVS increased the sensitivity to 79.3%, but with a loss of specificity to 40.0%. For female patients, the addition of QREVS to supine SSS ≥ 2 provided a sensitivity of 80% and specificity of 53.3%. The combination in women of supine SSS ≥ 2 and QREVS for pharmacologic stress testing only yielded a sensitivity of 92.9% with a specificity of 54.3%.
Total quantitative reversibility (QREVS) of the entire left ventricle in the supine position and subjective identification of defect reversibility in either the upright or supine position did not improve accuracy of the model in male patients due to limited specificity. SSSS ≥ 3 is supine summed stress score ≥ 3
In female patients, a supine summed stress score (SSSS) ≥ 2 provided the strongest single imaging predictor of angiographic coronary artery disease. Total quantitative reversibility (QREVS) for the entire left ventricle in the supine position was also a significant predictor of coronary artery disease in female patients. Rev. either, subjective identification of defect reversibility in either the upright or supine position
Supine summed stress score (SSSS) ≥ 3 provided favorable sensitivity and specificity in male patients. Sensitivity could be improved in males with supine summed stress percentage (SSSP) ≥ 6, but with loss of specificity. In female patients, a SSSS ≥ 2 combined with total quantitative reversibility (QREVS) for the entire left ventricle in the supine position provided the strongest imaging predictor of angiographic coronary artery disease, for all stress testing modalities and for pharmacologic testing only
Discussion
Limited data are available to guide the use in female patients of upright and supine imaging on a CZT cardiac camera. Nakazato provided the fundamental report comparing upright and supine CZT imaging to coronary arteriography.3 That report contained 15 women tested with a stress and rest Tc-99m perfusion study and was focused on quantitative perfusion defect size and extent. Patients in that study were highly selected, excluding patients with prior myocardial infarction, coronary artery revascularization, non-ischemic cardiomyopathy, or valvular heart disease. The present study used upright and supine technetium-99m perfusion imaging on a CZT camera with angiographic correlation, and examined a broad range of subjective and quantitative perfusion imaging variables in a population of 148 women and 112 men. In the present analysis, accuracy of upright and supine CZT imaging in women was highest by combining a highly sensitive criterion for perfusion defect size and extent, supine, SSS ≥ 2, with a quantitative measure of defect reversibility, QREVS.
The finding of reversibility of perfusion defects from stress to rest is consistent with ischemia and was independently predictive of angiographic coronary stenosis in women in the present study. Fixed defects, whether related to myocardial scar or attenuation artifacts, increase summed stress and rest scores, but do not specifically correspond to a residual coronary artery stenosis. In contrast to summed stress and rest scores, QREVS may be better suited to avoid incorrectly identifying shifting soft tissue artifacts related to change in body position as a sign of coronary stenosis in women. The summed difference score (SDS) is another accepted measure of defect reversibility. In the present study, SDS was univariately predictive of the presence or absence of angiographic coronary artery disease, but was not independently predictive in the multivariable models. This may reflect that the reference standard was the presence of angiographic stenosis and not specifically the presence of myocardial ischemia, as might be identified by a fluorodeoxyglucose positron emission tomogram. The more predictive variable, SSS, reflects the presence of anatomic disease related to scar or ischemia.
Guidelines from American Society of Nuclear Cardiology (ASNC)9 recommend routine use of 2-position imaging (upright/supine or supine/prone) to mitigate attenuation artifact defects. Nevertheless, when upright and supine images yield discordant findings that are not typical in location for attenuation artifact it may be useful to know if prediction of coronary disease is generally more accurate by upright or supine images. The present study found that stress perfusion defect size and extent on supine images alone was more accurate than on upright images alone for identifying angiographic CAD.
The current study included stress and rest images acquired in both the upright and supine positions. The combination of supine stress and rest images for detection of defect reversibility provided more accurate detection of CAD than upright stress and rest images, which appears to have implications for the best selection of stress/rest positioning for this CZT imaging system. In the current study, eight nuclear test variables which were strongly associated with angiographic CAD performed best when acquired in the supine position as compared to the upright position, including continuous variables SSS, SDS, SSP, SRP, QREV, supine LVEF, and transient ischemic dilation, as well as the binary variable, visual reversibility.
Gender-specific differences in cardiovascular epidemiology, clinical manifestations, management and outcomes are being increasingly identified. There has been a call for gender-specific research to identify such differences. A prior meta-analysis of 26 studies performed on conventional gamma cameras showed no significant difference in the sensitivity (P = .15) or specificity (P = .23) between male and female patients for detection of CAD.10 However, gender-specific analysis of nuclear variables in detecting angiographic CAD in the present study with an upright CZT cardiac camera showed that, in general, specificity was lower for women as compared to men. In addition, there were significant differences in optimal cut-off criteria in predicting angiographic CAD between the two genders. For male patients, a supine SSS ≥ 3 provided a high level of combined sensitivity (70.7%) and specificity (72.2%), and was the strongest perfusion variable in the multivariable models. For female patients, the single variable providing the highest combination of sensitivity and specificity was a supine SSS ≥ 2 alone, with a strong overall sensitivity of 90%, but with decline in specificity to 32.9%. An alternative single predictor was QREVS with a sensitivity of 85.0% and specificity of 34.8%. On multivariable analysis, variables identifying perfusion defect reversibility were significant predictors of CAD in female patients but not in male patients. Such differences in gender-specific interpretation of SPECT imaging have not been reported previously and may have significant implications for clinical practice. For female patients, with both supine SSS ≥ 2 and QREVS present, there was a sensitivity of 92.9% and specificity of 54.3% with pharmacologic stress and a combined sensitivity of 80% and specificity of 53.3% for both stress modalities (Figure 4).
To our knowledge, this is the first study in which gender-specific differences in interpretation of computer-generated data for CZT SPECT systems on an upright camera system were analyzed and presented. Gimelli and associates,11 who studied 61 female patients with supine and prone CZT imaging, and angiographic correlation, analyzed correlation with perfusion defect extent and severity. No quantitative or qualitative index of defect reversibility was reported. The current study differs from prior studies of upright and supine CZT imaging in terms of patient selection. We included consecutive patients presenting to a hospital stress nuclear laboratory, with no exclusion for known CAD, prior coronary revascularization, cardiomyopathy, left bundle branch block, heart failure, atrial fibrillation, or valvular heart disease, hence, the results may be applicable to a wide patient population. The presence of known CAD, including prior myocardial infarction, and/or prior coronary artery revascularization, is a likely confounder in the detection of residual coronary artery stenosis when stress defect size and extent is the principal variable. As a result, to provide an acceptable level of test specificity, test sensitivity may be reduced substantially. We therefore noted additional diagnostic options that improve test sensitivity, but at a larger loss of specificity. For example, in male patients, supine SSS ≥ 2 provided sensitivity of 76.0% and specificity of 55.6% and supine SSP ≥ 6 provided sensitivity of 79.3% and specificity of 53.3% (example in Figure 1).
Limitations of this study include retrospective analysis of patients who had both a SPECT-MPI and coronary angiography, which may have introduced referral bias. In addition, the study was conducted at a single large academic medical center, so the population characteristics and results may vary for other patient populations. The present study is limited by the small number of women (n = 21) who were found to have significant coronary artery disease at catheterization. As a result of the small number of female patients who exercised to target heart rate on the treadmill and were found to have significant angiographic CAD, it was not feasible to present exercise data separately. Data were, therefore, analyzed as a combined pharmacologic and exercise stress group and as a pharmacologic group only. Difference in the software used in the present study limited exact duplication of the previously published method for prediction of CAD by combined upright and supine CZT imaging.3 The present study, by not constraining the requirement for SSS ≥ 3 in both positions to abnormal pixels in the upright position that could be confirmed in the supine position may have provided slightly higher sensitivity and lower specificity. Further, coronary angiography was performed in most patients without functional assessment with fractional flow reserve or other invasive physiologic measurement. Future studies with comparison of the imaging findings to invasive functional measures and to long-term outcome will provide a better reference standard.
If higher sensitivity is a priority, we found in males that the variable supine summed stress percentage ≥ 6 could increase sensitivity to 79.3%, but with a decline in specificity to 53.3%. An alternative approach to increase sensitivity with less loss of specificity is to incorporate clinical and left ventricular function variables in a predictive model. The multivariable predictive models in the present study (see legend for Table 6, yielded improved prediction of CAD for male patients (sensitivity 82%, specificity 67%) and female patients (sensitivity 90%, specificity 71%), but these predictive models require prospective validation.
Conclusions
For males, a supine summed stress score (SSS) ≥ 3 provided favorable accuracy (sensitivity 70.7%, specificity 72.2%), and highest contribution to multivariable models for prediction of angiographic coronary artery disease. In females, supine SSS ≥ 2 provided the best cut-off for defect size and severity (sensitivity 90%, specificity 35.9%), but specificity was improved substantially to 53.3% with decrease in sensitivity to 80% by also requiring quantitative identification of perfusion defect reversibility in the supine position. Incorporating patient-related factors may optimize test performance further, for males (sensitivity 82%, specificity 67%) and for females (sensitivity 90%, specificity 71%).
New Knowledge Gained
The present study suggests that when the findings on supine and upright images are discordant in a territory not readily explained by attenuation artifact, that the supine images are more likely than the upright images to provide accurate identification of abnormal perfusion. The study also suggests that significant gender-based differences exist in the optimal cut-offs for objective CZT SPECT MPI variables acquired with an upright camera, and hence differences in the approach to test interpretation may be needed.
Abbreviations
- SPECT:
-
Single-photon emission computerized tomography
- SSS:
-
Summed stress score
- Combined SSS:
-
Combined summed stress score (SSS ≥ 3 both supine and upright, or SSS ≥ 5 in either upright or supine position)
- Supine SSS:
-
Summed stress score in supine position
- SRS:
-
Summed rest score
- SDS:
-
Summed difference score
- SRP:
-
Summed rest percentage
- SSP:
-
Summed stress percentage
- QREV:
-
Total quantitative change in defect reversibility in the entire left ventricle
- QREVS:
-
QREV in the supine position
References
Duvall WL, Sweeny JM, Croft LB, Barghash MH, Kulkarni NK, Guma KA, et al. Comparison of high efficiency CZT SPECT MPI to coronary angiography. J Nucl Cardiol 2011;18:595-604.
Gimelli A, Liga R, Duce V, Kusch A, Clemente A, Marzullo P. Accuracy of myocardial perfusion imaging in detecting multivessel coronary artery disease: A cardiac CZT study. J Nucl Cardiol 2017;24:687-95.
Nakazato R, Tamarappoo BK, Kang X, Wolak A, Kite F, Hayes SW, et al. Quantitative upright-supine high-speed SPECT myocardial perfusion imaging for detection of coronary artery disease: Correlation with invasive coronary angiography. J Nucl Med 2010;51:1724-31.
Betancur J, Hu L-H, Commandeur F, Sharir T, Einstein AJ, Fish MB, et al. Deep learning analysis of upright-supine high-efficiency SPECT myocardial perfusion imaging for prediction of obstructive coronary artery disease: A multicenter study. J Nucl Med 2019;60:664-70.
Perrin M, Djaballah W, Moulin F, Claudin M, Veran N, Imbert L, et al. Stress-first protocol for myocardial perfusion SPECT imaging with semiconductor cameras: High diagnostic performances with significant reduction in patient radiation doses. Eur J Nucl Med Mol Imaging 2015;42:1004-11.
Ben-Haim S, Almukhailed O, Neill J, Slomka P, Allie R, Shiti D. Clinical value of supine and upright myocardial perfusion imaging in obese patients using the D-SPECT camera. J Nucl Cardiol 2014;21:478-85.
Jameria ZA, Abdallah M, Fernandez-Ulloa M, O’Donnell R, Dwivedi AK, Washburn E, et al. Analysis of stress-only imaging, comparing upright and supine CZT camera acquisition to conventional gamma camera images with and without attenuation correction, with coronary angiography as a reference. J Nucl Cardiol 2018;25:540-9.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350-8.
Dorbala S, Ananthasubramaniam K, Armstrong IS, Chareonthaitawee P, DePuey EG, Einstein AJ, et al. Single photon emission tomography (SPECT) myocardial perfusion imaging guidelines: Instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol 2018;25:1784-846.
Iskandar A, Limone B, Parker MW, Perugini A, Kim H, Jones C, et al. Gender differences in the diagnostic accuracy of SPECT myocardial perfusion imaging: A bivariate meta-analysis. J Nucl Cardiol 2013;20:53-63.
Gimelli A, Bottai M, Quaranta A, Giorgetti A, Genovesi D, Marzullo P. Gender differences in the evaluation of coronary artery disease with a cadmium-zinc-telluride camera. Eur J Nucl Med Mol Imaging 2013;40:1542-8.
Acknowledgement
The authors thank Marge Duke for her invaluable assistance with the data management.
Disclosures
None of the above authors have any conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding
Funded by a Grant from the John R. Strauss Fund for Research and Education in Cardiovascular Imaging.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12350_2019_1878_MOESM1_ESM.tif
Supplementary material 1 Supplemental Fig. 1 Receiver operating curves for male model 2 and female model 2 (TIFF 4841 kb)
Rights and permissions
About this article
Cite this article
Athar, M.W., Waqar, F., Dwivedi, A.K. et al. Effects of gender and defect reversibility on detection of coronary disease with an upright and supine cadmium-zinc-telluride camera. J. Nucl. Cardiol. 28, 1569–1582 (2021). https://doi.org/10.1007/s12350-019-01878-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-019-01878-7