Abstract
Solitary fibrous tumor (SFT) is a rare mesenchymal neoplasm most often arising from the pleura and rarely in extra-pleural locations, including the gastrointestinal tract. We describe two cases of a SFT presenting as submucosal colonic lesion and review the literature on this lesion. One submucosal lesion was localized in the cecum and was 10 mm in size. The second lesion presented as a 17 mm submucosal rectal lesion. Both lesions presented as well-circumscribed submucosal lesions arranged in short fascicles, blending with abundant collagenous stroma. In both cases, the spindle cells were positive for CD34, STAT6 and CD99, and molecular studies showed NAB2:STAT6 fusion supporting the diagnosis of SFT. Both patients are alive and well 10 and 5 years post-excision, respectively. In conclusion, SFT can occur in the colon as a submucosal lesion and should be included in the differential diagnosis of colonic mesenchymal lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Solitary fibrous tumor (SFT) is a rare spindle cell neoplasm first described as a pleural-specific tumor [1]. It has since been identified in several extra-pleural locations including abdominal cavity, soft tissue, mediastinum, leptomeninges, retroperitoneum, and orbit. Rare cases involving the liver, pancreas, lung, adrenal, bladder, prostate, testis, thyroid, salivary glands, and gastrointestinal (GI) tract have also been described [2]. SFT of the GI tract is very rare, and only a few reports of cases mainly localized in the serosal surface or mesentery of sigmoid colon [3], or muscularis propria or mesentery of the small bowel [4] have been described. The cell of origin of this rare mesenchymal lesion is unknown. In this article, we report two rare cases of SFT presenting as a submucosal colonic lesions and review the literature on this topic.
Case series
Case 1
Our first case of SFT has been previously described by our group in 2016 and now included in this short report [5]. The patient was a 54-year-old asymptomatic male who underwent an elective screening colonoscopy. A 10 mm submucosal lesion was detected in the cecum and completely excised by snare polypectomy. (Fig. 1A) Histologically, the colonic mucosa overlying the nodule was unremarkable, and the submucosa showed a well-circumscribed nodule (Fig. 1B) composed of a patternless proliferation of spindle cells preferentially localized at the periphery of the nodule (Fig. 1C) and a central hypocellular fibro collagenous area with a few slit-like vascular spaces (Fig. 1D). The neoplastic cells were bland with uniform elongated nuclei and scant cytoplasm.
A Endoscopic appearance of the submucosal lesion in the cecum. B Low-power hematoxylin and eosin (H&E)-stained submucosal mesenchymal lesion. C Intermediate power of hypercellular spindle cell area at the periphery of the polyp. D Intermediate power of hypocellular fibrosclerotic and vascular area at the center of the lesion. E Immunohistochemistry showing strong nuclear staining of the spindle cells for STAT6. F Immunohistochemistry showing positive staining for CD34 confirms the unequivocal diagnosis of a solitary fibrous tumor.
The immunohistochemical profile of the neoplastic cells was characterized by strong and diffuse positivity for CD34, (Fig. 1E) CD99, and in particular, demonstrated strong nuclear staining for STAT6 protein (Fig. 1F). Pertinent negative immunohistochemical stains included: CD117, DOG-1, S100, EMA, SMA, and MSA. The MIB-1 labeling index was low ~ 1%. Molecular studies showed NAB2:STAT6 fusion. Based on the morphology and immunohistochemical profile, a diagnosis of SFT was rendered. The lesion was completely removed endoscopically and the patient is currently asymptomatic, without any complication, recurrence, or metastasis years after polypectomy.
Case 2
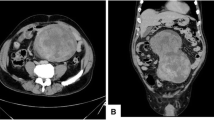
The second case is that of 58-year-old female who underwent an elective screening colonoscopy and was found to have a 17 mm submucosal lesion in the distal rectum. (Fig. 2A) The lesion was completely excised via endoscopic transanal approach. Macroscopically, it appeared well demarcated, and the cut surface showed a 17 × 16 × 8 mm submucosal, semi-firm, white-tan nodule. Histologically, the rectal mucosa overlying the lesion was unremarkable, and the submucosa showed a well-demarcated fibrous nodule (Fig. 2B) composed of a proliferation of spindle cells with a keloid-like collagenous stroma (Fig. 2C) and hemangiopericytoma-like vessels (Fig. 2D). The neoplastic cells were bland with uniform elongated nuclei and scant cytoplasm.
A Endoscopic appearance of the submucosal lesion in the posterior rectum. B Low-power hematoxylin and eosin (H&E)-stained deep submucosal well-circumscribed nodule. C High-power of spindle cell proliferation without cytologic atypia or prominent mitotic activity intermixed with thick collagenous and keloid fibers. D Intermediate power of Staghorn-like proliferation of dilated blood vessels in a fibromyxoid background. E CD34 immunohistochemistry showing positive staining of the spindle cells. F STAT6 Immunohistochemistry showing diffuse and strong nuclear staining supporting the diagnosis of a solitary fibrous tumor
On immunohistochemistry, the neoplastic cells demonstrated similar immunophenotype as in case 1 with diffuse positivity for CD34, (Fig. 2E) CD99, and nuclear staining for STAT6 protein (Fig. 2F). Desmin was weakly and focally expressed. Negative immunohistochemical stains included: CD117, DOG-1, S100, EMA, SMA, S100, and MSA. The MIB-1 labeling index was low < 1%. Molecular studies showed NAB2:STAT6 fusion. Based on the morphology, immunohistochemical and molecular profile, a diagnosis of SFT was rendered. In both cases, the lesion lacked infiltrative margins, high cellularity, nuclear pleomorphism, tumor necrosis, large size, and high mitotic activity or high proliferative activity index by MIB-1, features associated with an increased risk of malignant behavior [6]. The patient is currently asymptomatic, without any complication, recurrence, or metastasis 5 years after excision.
Review of the literature
Solitary fibrous tumor (SFT) is a rare fibroblastic mesenchymal neoplasm most often arising from the pleura and rarely in extra-pleural locations, including the gastrointestinal tract.
From a review of the literature, we have identified only one additional case of SFT in the colon presenting as submucosal lesion [7]. The patient was a 66-year-old male who on colonoscopy had a 35 mm pedunculated lesion in the descending colon. The histology showed a well-demarcated submucosal proliferation of oval to short, haphazardly arranged spindle shaped cells with scattered ectatic blood vessels, and central areas with more collagenous stroma. No cytological atypia, or necrosis was identified, and only rare mitosis was present. The neoplastic cells were strongly and diffusely positive for CD34, and STAT6, while negative for CD117, DOG-1, SMA and S100. No molecular studies were reported. Polypectomy was curative, and on follow-up, the patient remains disease-free.
Discussion
The first case of colonic SFT presenting as submucosal lesion was reported in the cecum by one of the authors and also included in this short report [5]. Now, we expand our experience on this rare submucosal colonic lesion by describing an additional case diagnosed more recently in our institution and review the literature on this topic. So far, to our knowledge, only three cases of submucosal SFT have been described in the colon (Table 1).
Two of which occurred in male, with a mean age of 59 (range 54–66) years.
In all instances, they were identified in asymptomatic patients as an incidental finding during screening colonoscopy. Endoscopically, they appear as tan-pink fleshy submucosal nodules. Macroscopically, they are well-delineated, firm and lobulated solitary submucosal lesions with gray-white cut surface. The mean tumor size is 21 mm (range 10–35 mm). Microscopically, they are well circumscribed and demonstrate a haphazard “patternless” architecture, with hypercellular areas of spindle cells preferentially located at the periphery of the nodule, and hypocellular sclerotic centrally located areas containing keloid-like collagenous stroma and hemangiopericytoma-like vessels. No necrosis or hemorrhage was identified in any of the 3 cases. Cytologically, the cells are bland with oval to short spindled nuclei without cytological atypia and only rare mitoses.
Immunohistochemically, the tumor cells are usually positive for CD34 in 95% of cases; however, this marker is not specific, because it may be seen in other spindle cell lesions of the GI tract, such as gastrointestinal stromal tumors (GIST) and inflammatory fibroid polyps (IFP). The most specific marker is STAT6 which shows diffuse nuclear positivity [8].
CD99, Bcl2, and vimentin may be also positive but not specific, and S100, CD117, DOG-1, SMA, EMA, and Desmin are negative but useful in the differential diagnosis with other spindle cell lesions of the GI tract [9].
Molecular studies have demonstrated that the majority of SFTs are consistently associated with a gene fusion of the transcriptional repressor NAB2 with the transcriptional activator STAT6 gene [10] and an IHC stain for STAT6 protein has been shown to be a reliable surrogate marker for the detection of this fusion [9]. Our two cases were both positive for NAB2:STAT6 fusion and expressed STAT6 immunostaining.
Although, in other locations, SFT may occasionally demonstrate an unpredictable clinical behavior with local or distant recurrences even many years after resection [6], so far the prognosis of polypoid SFT of colon is excellent, and complete endoscopic removal appears curative.
A Pub-Med search on this topic was performed, and with the exception of the case previously reported by Katerji [7], no other cases were identified. In fact, to the best of our knowledge, the other SFTs of the GI tract reported in the literature were located in the deeper layers of the lower GI tract and did not appear as submucosal lesions, and consequently, they are not pertinent to our study. In fact, 3 SFTs arose from the serosal surface of the sigmoid, 3 from the mesentery of sigmoid and small bowel, and 2 from the muscularis propria of the small bowel and ascending colon [11]. Recently, a multivariate risk model proposed by Demicco et al. has resulted in improved prognostication over the traditional distinction between benign/malignant SFTs. In this model, using four variables including age, tumor size, mitotic count, and tumor necrosis, SFTs may been stratified into low, intermediate, or high-risk groups with a 5-year risk of metastatic disease of 0%, 10%, and 73%, respectively [12]. Appling this model in our two cases of SFT, the risk for metastatic disease would be 0%. However, this model has not been yet validated in such rare colonic submucosal SFTs and more cases are needed.
Mesenchymal lesions with spindle cell morphology are uncommon in the GI tract, and the differential diagnosis usually includes leiomyoma, schwannomas, GIST, fibromatosis, fibroblastic polyp/perineurioma, inflammatory myofibroblastic polyps, and inflammatory fibroid polyps. Table 2 summarizes the salient immunohistochemical features useful in distinguishing a SFT from other mimickers. In conclusion, with this short report, we would like to bring to the attention of the practicing surgical pathologist that SFT should also be included in the differential diagnosis of colonic submucosal mesenchymal lesions. The diagnosis is confirmed by positive immunohistochemical stains for CD34 and STAT6 protein, and endoscopic resection of the lesions appears to be curative.
References
Klemperer P, Rabin C. Primary neoplasms of the pleura. Arch Pathol. 1931;11:385–412.
Fletcher CDM, Bridge JA, Hogendoorn PCW, et al. WHO classification of tumors of soft tissue and bone. Lyon: IARC Press; 2013.
Bratton L, Salloum R, Cao W, Huber AR. Solitary fibrous tumor of the sigmoid colon masquerading as an adnexal neoplasm. Case Rep Pathol. 2016;2016:4182026.
Zhang GJ, Li RT, Zhou Y, Huang F, Zhao ZC, Li WD, Fu WH. Solitary fibrous tumor of small bowel mesentery with postoperative bowel obstruction: a case report and review of literature. Int J Clin Exp Pathol. 2015;8(9):11691.
Ligato S, Collins K, Song X. Solitary fibrous tumour presenting as a submucosal colonic polyp: a new addition to the family of mesenchymal polyps of the gastrointestinal tract. Histopathology. 2016;69(6):1088–90.
Demicco EG, Harms PW, Patel RM. Et al, Extensive survey of STAT6 expression in a large series of mesenchymal tumors. Am J Clin Pathol. 2015;143:672–82.
Katerji R, Agostini-Vulaj D. Solitary fibrous tumor presenting as a colonic polyp: report of a case and literature review. Human Pathol Case Rep. 2021;25: 200547.
Doyle LA, Vivero M, Fletcher CD, et al. Nuclear expression of STAT6 distinguishes solitary fibrous tumor from histological mimickers. Mod Pathol. 2014;27:390–5.
Yoshida A, Tsuta K, Ohno M, et al. STAT6 Immunohistochemistry is helpful in the diagnosis of Solitary Fibrous Tumor. Am J Surg Pathol. 2014;38:552–9.
Mohajeri A, Tayebwa J, Collin A, et al. Comprehensive genetic analysis identifies a pathognomonic NAB2-STAT6 fusion gene, nonrandom secondary genomic imbalances, and a characteristic gene expression profile in solitary fibrous tumor. Genes Chromosomes Cancer. 2013;52:873–86.
Hasegawa T, Matsuno Y, Shimonda T, et al. Extrathoracic solitary fibrous tumors : Their histological variability and potentially aggressive behavior: Hum Pathol. 1999;30:1464–73.
Demicco EG, Fritchie KJ, Han A. Solitary fibrous tumor. WHO Classification of Tumors of Soft Tissue and Bone. Lyon: IARC Press; 2020. p. 104–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Patient consent statement
Please note a portion of this material was published as a correspondence in Histopathology (volume 69, issue 6) in 2016.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akrmah, M., Ibrahim, E., Mnayer, L.O. et al. Solitary fibrous tumor occurring in the colon as submucosal mesenchymal lesion: report of two cases and review of the literature. Clin J Gastroenterol 17, 396–400 (2024). https://doi.org/10.1007/s12328-024-01936-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-024-01936-9