Abstract
A 56-year-old man was referred to our hospital for fever and back pain. Contrast-enhanced computed tomography, magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound revealed marked dilatation of the main pancreatic duct from head to tail and surrounding cysts with no evidence of pancreatic masses or obstructive causes. Endoscopic retrograde pancreatography (ERP) from the major duodenal papilla showed a short and narrow ventral pancreatic duct and ERP from the minor duodenal papilla revealed a dilated dorsal pancreatic duct with a narrow branch which connected to the ventral pancreatic duct. Intra-ductal ultrasound showed no nodules in the main pancreatic duct, and pancreatic cytology was negative. Peroral pancreatoscopy showed that the main pancreatic duct was covered with normal epithelium without tumors. Biopsy from the pancreatic duct showed no neoplastic changes. He was diagnosed with incomplete pancreas divisum accompanied by dilatation of dorsal pancreatic duct. Sphincterotomy of the minor duodenal papilla was performed. Seven months later, MRCP re-examination showed that the main pancreatic duct dilatation was relieved. Review of the literature identified 10 cases of pancreas divisum accompanied by dilatation of main pancreatic duct to date. To our knowledge, this is the first reported case of pancreas divisum with pancreatic duct dilatation without Santorinicele.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Main pancreatic duct dilatation is often a clinical problem. The most common causes of main pancreatic duct dilatation include pancreatic tumors, such as pancreatic cancer and intraductal papillary mucinous neoplasm (IPMN), and chronic pancreatitis.
Here we present an extremely rare case of incomplete pancreas divisum accompanied by marked dilatation of dorsal pancreatic duct. To our knowledge, this is the first reported case of pancreas divisum with dorsal pancreatic duct dilatation without Santorinicele.
Case report
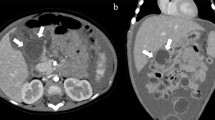
A 56-year-old man was referred to our hospital for fever and back pain. He had a medical history of type 2 diabetes mellitus and HbA1c had increased from around 7.5 to 9.1%, indicating worsening of diabetes mellitus. Blood tests showed no elevation of pancreatic enzymes or tumor markers. The values of CEA, CA19-9, SPAN-1, DUPAN2, Elastase1, SLX and IgG4 were within the normal range. There were no findings that were suspicious of pancreatitis. Contrast-enhanced computed tomography (CT) revealed marked dilatation of the main pancreatic duct from head to tail and surrounding small cysts (Fig. 1). Magnetic resonance cholangiopancreatography (MRCP) showed that the main pancreatic duct was dilated up to 18 mm from head to tail (Fig. 2). The surrounding area showed multifocal cystic changes, and there were no obvious sites of obstruction in the main pancreatic duct. Fluorodeoxyglucose-positron emission tomography (FDG-PET) showed no abnormal accumulation in the pancreas. Convex type endoscopic ultrasound (EUS) showed that the main pancreatic duct was dilated to a maximum size of 19 mm, and there were numerous cysts in the pancreas, but there were no obvious nodules within the duct or cysts. Convex type EUS also showed that there was no mass that caused obstruction of the main pancreatic duct around the major and minor duodenal papilla (Fig. 3).
a, a’ The arterial phase. b, b’ The portal phase. c, c) The equilibrium phase. Contrast-enhanced computed tomography (CT) of the abdomen shows marked ductal dilatation (red arrow heads) and thinning of the pancreatic parenchyma from the body of the pancreas to the tail. No tumor causing obstruction can be noted
Convex type EUS imaging. a The main pancreatic duct is remarkably dilated (asterisk). There are numerous cysts in the body and tail pancreas, but there are no obvious nodules within the duct or cysts. b There is no mass around the major and minor duodenal papilla. The terminal portion of the dorsal pancreatic duct near the minor duodenal papilla is not dilated (2.6 mm. red arrow heads). Bile duct (yellow arrow heads)
For the definitive diagnosis, endoscopic retrograde cholangiopancreatography (ERCP) was performed. On side-viewing endoscope, neither the major duodenal papilla nor minor duodenal papilla were dilated due to mucinous secretion from the orifice. There was no mass around the major and minor duodenal papilla (Fig. 4). Pancreatography from the major duodenal papilla showed a short and narrow ventral pancreatic duct (Fig. 5a). Pancreatography from the minor duodenal papilla showed a markedly dilated dorsal pancreatic duct (Fig. 5b) and a narrow branch which connected to the ventral pancreatic duct (Fig. 5c). Whole pancreatography from the minor duodenal papilla depicted multiple cystic lesions of the pancreas body and tail (Fig. 6). Intraductal ultrasound (IDUS) showed no nodules in the main pancreatic duct, and pancreatic cytology was negative. Based on these findings, he was diagnosed with incomplete pancreas divisum with dilatation of dorsal pancreatic duct. Since main pancreatic duct was considered to be dilated due to incomplete pancreas divisum, sphincterotomy of the minor duodenal papilla was performed. To rule out the possibility of a mixed type IPMN with dilatation of the main pancreatic duct, a peroral pancreatoscopy (POPS) from the minor duodenal papilla was performed (Fig. 7). The main pancreatic duct was covered with normal epithelium, and there were no papillary elevated lesions which were suspicious of tumor. Narrow-band imaging (NBI) observation showed no atypical vessels, and biopsy from the pancreatic duct showed no neoplastic changes. Seven months later, MRCP re-examination showed that dilatation of the main pancreatic duct was relieved (Fig. 8). The patient’s condition was fairly good. There were no abdominal pain, other symptoms or elevated pancreatic enzymes suggestive of pancreatitis. HbA1c had decreased from 9.1 to 7.0% without changing the treatment, indicating improvement of diabetes mellitus. He has been under careful follow-up.
On ERCP examination, a contrast from the major duodenal papilla shows a dendritic appearance of the ventral pancreatic duct. Bile duct (red arrow heads), ventral pancreatic duct (blue arrow heads). b, c Contrast from the minor duodenal papilla reveals a dilated dorsal pancreatic duct, and a thin ventral pancreatic duct can also be seen. The diagnosis of incomplete pancreas divisum is made. Dorsal pancreatic duct (red arrow heads), ventral pancreatic duct (blue arrow heads), a narrow branch between dorsal and ventral pancreatic duct (yellow arrow heads)
a, b Observation of the pancreatic tail using a peroral pancreatoscopy (POPS) shows that the pancreatic duct is covered with flat normal epithelium, and there are no papillary elevated lesions like a salmon roe, which is suspicious for IPMN. c No atypical vessels can be detected by narrow band imaging (NBI) observation
Discussion
Here we reported an extremely rare case of incomplete pancreas divisum accompanied by marked dilatation of dorsal pancreatic duct. When we excluded cases of pancreas divisum with pancreatic duct dilatation due to pancreatic tumors and chronic pancreatitis, our literature review yielded only 10 cases of pancreas divisum accompanied by dilatation of dorsal pancreatic duct (Table 1). However, all these 10 cases were coexistent with Santorinicele. To our knowledge, this is the first reported case of pancreas divisum with pancreatic duct dilatation without Santorinicele.
Santorinicele is defined as a focal cystic dilatation at the termination of the dorsal pancreatic duct near the minor duodenal papilla and was first reported by Eisen et al. in 1994 [1]. Santorinicele is caused by stenosis of the minor duodenal papilla and wall weakness in the same area, and is sometimes seen in cases of pancreas divisum. It is extremely rare for pancreas divisum to be accompanied by dilatation of dorsal pancreatic duct without pancreatic tumors, such as pancreatic cancer and IPMN, or chronic pancreatitis. Since our case did not present with focal cystic dilatation at the termination of the dorsal pancreatic duct near the minor duodenal papilla, it did not meet the criteria for Santorinicele. We speculate the reason why Santorinicele was not seen in this case is because the ventral and dorsal pancreatic ducts were connected with each other at the relatively caudal site, and because the increase in intraductal pancreatic pressure was not confined to the area close to the minor duodenal papilla, but was extended to the caudal side. It is speculated that the multiple cystic changes of pancreas were caused by impaired pancreatic drainage and increased intra-ductal pressure due to impaired papillary function resulting from pancreas divisum. As a result, the caudal pancreatic duct was markedly dilated and multiple cystic changes of the body and tail pancreas were observed. Thus, we consider the diagnosis of multiple cysts was retention cysts. When encountering a similar case, it is important to exclude the tumor around the minor duodenal papilla.
We summarized the review of the literature regarding 10 cases of pancreas divisum accompanied by dilatation of dorsal pancreatic duct. All these 10 cases had Santorinicele. The median age of these patients was 70 years old, with 3 males and 7 females. The main symptom was abdominal pain accompanied by recurrent acute pancreatitis. Eight cases were complete pancreas divisum and two cases were unknown. Our case was incomplete pancreas divisum without past history of acute pancreatitis. Regarding the endoscopic treatment, 2 cases underwent balloon dilatation of the minor duodenal papilla, whereas 6 cases underwent sphincterotomy of the minor duodenal papilla.
In conclusion, we presented an extremely rare case of incomplete pancreas divisum accompanied by dilatation of dorsal pancreatic duct. Only 10 cases of pancreas divisum accompanied by dilatation of dorsal pancreatic duct have been reported in the literature. To our knowledge, this is the first reported case of pancreas divisum with dorsal pancreatic duct dilatation without Santorinicele. When encountering the remarkable dilatation of the dorsal pancreatic duct, it is crucial to exclude the tumor around the minor duodenal papilla.
Abbreviations
- CT:
-
Computed tomography
- MRCP:
-
Magnetic resonance cholangiopancreatography
- FDG-PET:
-
Fluorodeoxyglucose-positron emission tomography
- EUS:
-
Endoscopic ultrasound
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- IDUS:
-
Intraductal ultrasound
- IPMN:
-
Intraductal papillary mucinous neoplasm
References
Eisen G, Schutz S, Metzler D, et al. Santorinicele: new evidence for obstruction in pancreas divisum. Gastrointest Endosc. 1994;40:73–6.
Seibert DG, Matulis SR. Santorinicele as a cause of chronic pancreatic pain. Am J Gastroenterol. 1995;90:121–3.
Manfredi R, Costamagna G, Brizi MG, et al. Pancreas divisum and “santorinicele”: diagnosis with dynamic MR cholangiopancreatography with secretin stimulation. Radiology. 2000;217:403–8.
Costamagna G, Ingrosso M, Tringali A, et al. Santorinicele and recurrent acute pancreatitis in pancreas divisum: diagnosis with dynamic secretin-stimulated magnetic resonance pancreatography and endoscopic treatment. Gastrointest Endosc. 2000;52:262–7.
Peterson MS, Slivka A. Santorinicele in pancreas divisum: diagnosis with secretin-stimulated magnetic resonance pancreatography. Abdom Imaging. 2001;26:260–3.
Chalazonitis NA, Lachanis BS, Laspas F, et al. Pancreas divisum: magnetic resonance cholangiopancreatography findings. Singapore Med J. 2008;49:951–4 (quiz 955).
Khan SA, Chawla T, Azami R. Recurrent acute pancreatitis due to a santorinicele in a young patient. Singapore Med J. 2009;50:e163-165.
Lutzak GD, Gluck M, Ross AS, et al. Endoscopic minor papilla sphincterotomy in patients with santoriniceles reduces pain and improves quality of life. Dig Dis Sci. 2013;58:2075–81.
Author information
Authors and Affiliations
Contributions
NA, YT, MW and TI: participated in diagnosis and drafted this manuscript. AF, YN and HS: supervised this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aoyama, N., Taniguchi, Y., Wada, M. et al. A case of pancreas divisum with marked dilatation of dorsal pancreatic duct. Clin J Gastroenterol 15, 1204–1209 (2022). https://doi.org/10.1007/s12328-022-01713-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-022-01713-6