Abstract
We encountered a rare case of a pancreatic head tumor protruding into the portal vein, later diagnosed histopathologically as primary leiomyosarcoma of the portal vein. A 59-year-old woman visited our hospital because of an elevated amylase level during a medical checkup. Computed tomography showed a moderately contrasted, well-defined mass of 35-mm diameter in the pancreatic head with protrusion into the portal vein. Endoscopic ultrasonography revealed a well-defined and hypoechoic mass. Fluorodeoxyglucose-positron emission tomography showed a high accumulation of fluorodeoxyglucose in the pancreas head. We performed a subtotal stomach-preserving pancreaticoduodenectomy with portal vein resection. Gross findings of the fixed specimen showed a white solid, multinodular mass in the pancreatic parenchyma with protrusion into the portal vein. Histopathological examination showed proliferation of spindle-shaped eosinophilic cells with intricate bundle-like growth, indicating leiomyosarcoma. Examining the tumor location and invasion suggested portal vein as the origin. Although portal vein primary leiomyosarcoma is rare, leiomyosarcoma should be considered as a differential diagnosis in pancreatic head tumors with protrusion into the portal vein. Precise macroscopic and histopathological examinations can help determine the definitive diagnosis and origin of leiomyosarcoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Leiomyosarcoma is a soft tissue tumor arising from smooth muscle cells with significant metastatic potential and poor prognosis, accounting for approximately 5–7% of soft tissue sarcoma cases [1]. Leiomyosarcoma predominantly affects women in their sixth decade of life [2]. Cases involving vascular structures represent only 2% of the cases and are primarily localized to the inferior vena cava (IVC) [3, 4]. Vascular leiomyosarcoma has been reported to affect minor vessels. However, only a few cases of portal vein (PV) leiomyosarcoma are reported in the literature [5,6,7,8,9,10,11,12,13,14,15,16,17]. Herein, we report a case of primary leiomyosarcoma originating from the PV, which presented as a pancreatic head tumor with protrusion into the PV.
Case presentation
A 59-year-old woman visited our hospital because of an elevated amylase level during a medical checkup. She had no subjective symptoms or abdominal masses. Blood tests showed the following vitals—white blood cell count, 5000/μL; hemoglobin level, 12.9 g/dL; aspartate transaminase level, 21 U/L; alanine transaminase level, 17 U/L; γ-glutamyl transpeptidase level, 26 U/L; amylase level, 210 U/L (normal range: 54– 168 U/L); carcinoembryonic antigen level, 1.1 ng/mL; and carbohydrate antigen 19–9 level, 2.5 U/mL. There were no abnormalities, except for an elevated amylase level.
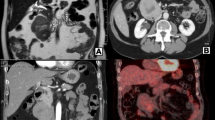
Dynamic computed tomography showed a 35 × 30-mm well-demarcated lobulated mass in the pancreatic head, which had iso-, low-, low-, low- density in plain, arterial, portal, and equilibrium phase, respectively. The tumor was adjacent to the right wall of the PV and the superior mesenteric vein (SMV) and protruded into the PV without calcification or fatty component (Fig. 1). There was no dilatation of the main pancreatic or common bile ducts. Extracorporeal ultrasonography showed a 35 × 29-mm hypoechoic mass compressing the SMV in the pancreatic head (Fig. 2). Endoscopic ultrasonography (EUS) showed a well-defined nodular heterogeneous hypoechoic mass in the pancreatic head. The tumor expanded outside of the pancreas. Contrast-enhanced EUS using Sonazoid showed early staining with a partially poor enhancement in one area (Fig. 3). The T1-weighted image of magnetic resonance imaging (MRI) showed that the tumor had a signal almost equal to that of the muscle, while the T2-weighted image showed the tumor was mildly higher in signal than the muscle. MRI could not identify any difference in septa or internal properties. Magnetic resonance cholangiopancreatography (MRCP) did not show stenosis or dilatation of the main pancreatic duct or common bile duct (Fig. 4). Fluoro-deoxyglucose-positron emission tomography-computed tomography (FDG-PET-CT) showed hyper-accumulation of FDG in the pancreatic head with a SUVmax of 6.52 (Fig. 5). There was no abnormal FDG hyper-accumulation in other organs. Our preoperative differential diagnosis included gastrointestinal stromal tumor, neuroendocrine neoplasm, solid pseudopapillary neoplasm, acinar cell carcinoma, and anaplastic ductal carcinoma based on the imaging characteristics. Endoscopic ultrasound-fine-needle aspiration was not performed because of the necessity of pancreatoduodenectomy (PD). Subtotal stomach-preserving PD was performed with PV resection. The SMV was resected annularly 2 cm in length and anastomosed. The splenic vein was preserved (Fig. 6). The duration of surgery was 7 h, and the total blood loss was 360 mL.
Dynamic computed tomography images show a well-demarcated lobulated hypodense mass 35 mm in size in the pancreatic head (arrowhead). The tumor was adjacent to the superior mesenteric vein (SMV) and protruded into the portal vein (arrow). The tumor was mildly contrasted from the arterial phase to the equilibrium phase and is heterogeneously contrasted, with iso-, low-, low-, low- density in plain, arterial, portal, and equilibrium phase, respectively. a plain, b arterial, c portal, and d equilibrium phase
T1 weighted image (a) of magnetic resonance imaging shows that the tumor signal is almost equal to the muscle signal, while T2 weighted image (b) shows that the tumor is mildly higher in signal intensity than the muscle. Magnetic resonance cholangiopancreatography (c) showed neither stenosis nor dilatation of the main pancreatic duct and common bile duct
Macroscopic findings of the cut surface of the fixed resected specimen showed a white solid multinodular tumor protruding into the PV lumen on the right side of the PV (Fig. 7). Histopathologically, the tumor was composed of a palisade arrangement of spindle-shaped cells with nuclei of unequal size, cellular atypia, and eight mitoses in 10 high-magnification views (Fig. 8). Immunohistochemistry showed positive calponin, desmin, and α-SMA, and a 20% Ki-67 index (Fig. 9). In contrast, tests for CD34, c-Kit, and S-100 were negative. Elastica-Goldner staining showed well preserved PV elastic plate (Fig. 10). Considering the tumor location and protrusion into the PV lumen, the tumor was presumed to have originated from the connective tissue of the outer layer of the PV. The histopathological diagnosis was PV leiomyosarcoma invading the pancreatic head. The surgical margin was negative for leiomyosarcoma.
Because of the soft pancreas and undilated main pancreatic duct, she developed a refractory grade C pancreatic fistula (International Study Group grading system) [18]. Fistulo-jejunal anastomosis was performed on the 145th postoperative day. The patient was discharged from our hospital 171 days after the first surgery. Thirty-eight months after the first surgery, CT showed an irregular, low-density lesion around the SMV (Fig. 11), indicating local recurrence. Considering the difficulty of surgical resection, radiation therapy (50.4 Gy) was administered, and the patient has been alive for the last 46 months after the surgery with partial response to radiation therapy.
Discussion
Leiomyosarcoma is a relatively rare mesenchymal tumor originating from the smooth muscle. Most leiomyosarcomas are found in the uterus, retroperitoneum, mesentery, and omentum (40%–45%); leiomyosarcomas originating from the vascular structures are rare (2%) [19, 20]. Leiomyosarcomas of venous origin are five times more common than those of arterial origin, and leiomyosarcomas of the IVC account for approximately 50% of primary venous leiomyosarcomas [21, 22].
Because the preoperative imaging characteristics, in this case, suggested a well-demarcated solid tumor with partial degeneration, our preoperative differential diagnosis included gastrointestinal stromal tumor, neuroendocrine neoplasm, solid pseudopapillary neoplasm, acinar cell carcinoma, and anaplastic ductal carcinoma, retrospectively. However, a well-demarcated tumor with expansive growth, protrusion into the PV lumen, as well as neither stenosis nor dilatation of the main pancreatic duct and common bile duct despite a large tumor in the pancreas head can indicate a giant leiomyosarcoma of the PV. Because the tumor was diagnosed before the development of portal hypertension and collateral blood vessels, standard PD with PV resection was performed safely.
Our extensive search for the reports of leiomyosarcoma originating PV (using the search terms ‘Leiomyosarcoma’ and ‘Portal vein’ in the PubMed from 1950 to 2021, and Japana Centra Revuo Medicina from 1977 to 2021) found only 13 reports of surgically resected leiomyosarcoma of PV origin in English and Japanese literature, including our case (Table 1) [6,7,8,9,10,11,12,13,14,15,16,17]. Among these reports, the median age of patients was 62 years (range: 42–78 years), and the sex was predominantly female (69%). The most frequent symptom was upper abdominal pain. The most frequent locations were the pancreatic head and porta hepatis, followed by liver and mesentery. The growth pattern of PV leiomyosarcoma can be divided into three types: intraportal with tumor plugs, extraportal growth, and combined type [11]. The intraportal, extraportal, and combined type growth was observed in 2, 2, and 5 cases, respectively. In the intraportal and combined types, portal hypertension with the development of collateral blood vessels can occur due to PV obstruction, making the resection challenging [7, 12, 14, 16]. The median tumor size was 5.9 cm (range: 3–30 cm) among all the cases. The most frequent CT findings were well-demarcated, enhanced, heterogeneous tumor. There was no specific MRI finding among the studies. Preoperative biopsy, including endoscopic ultrasound-guided fine-needle aspiration, was performed in 6 cases, which led to the preoperative diagnosis of leiomyosarcoma in 5 cases. The most frequent surgical procedure was PD with PV resection followed by hepatectomy with PV resection. Recurrence was mostly local, although follow-up periods were limited (median: 20 months).
PV leiomyosarcoma should be considered as a differential diagnosis for pancreatic head tumors with protrusion into the PV. Precise macroscopic and histopathological examination, including immunohistochemistry, can help determine the definitive diagnosis and origin of leiomyosarcoma.
References
George S, Serrano C, Hensley ML, et al. Soft tissue and uterine leiomyosarcoma. J Clin Oncol. 2018;36:144–50.
Komatsu H, Tsuchiya T, Honda H, et al. Aggressive surgery aids long-term IVC leiomyosarcoma survival: report of a case. Jpn J Gastroenterol Surg. 2011;44:510–8.
Alkhalili E, Greenbaum A, Langsfeld M, et al. Leiomyosarcoma of the inferior vena cava: a case series and review of the literature. Ann Vasc Surg. 2016;33:245–51.
Gage MJ, Patel AV, Koenig KL, et al. Non-vena cava venous leiomyosarcomas: a review of the literature. Ann Surg Oncol. 2012;19:3368–74.
Wilson SR, Hine AL. Leiomyosarcoma of the portal vein. AJR. 1987;149:183–4.
Sundaresan M, Kelly SB, Benjamin IS, et al. Primary hepatic vascular leiomyosarcoma of probable portal vein origin. J Clin Pathol. 1990;43:1036.
Goldin SB, Webb TH, Lillemoe KD. Leiomyosarcoma arising from the superior mesenteric vein. Surgery. 2002;132:108–9.
Celdrán A, Frieyro O, del Río A, et al. Leiomyosarcoma of the portal venous system: a case report and review of literature. Surgery. 2004;135:455–6.
Leporrier J, Alkofer B, Lebreton G, et al. Leiomyosarcoma of the superior mesenteric vein: a diagnostic and therapeutic challenge. J Hepato-Bil Pancreat Surg. 2006;13:584–6.
Kominami A, Kawasaki K, Tanaka K, et al. A case of leiomyosarcoma arisen from the ascending mesocolon and enlarged rapidly. J Jpn Surg Assoc. 2013;74:226–32 (in Japanese with English abstract).
Boudjema K, Sulpice L, Levi Sandri GB, et al. Portal vein leiomyosarcoma, an unusual cause of jaundice. Dig Liver Dis. 2014;46:1053–4.
Nishida T, Yoshidome H, Shinmura K, et al. A rare resected leiomyosarcoma of the portal vein origin with well-developed collateral veins. Jpn J Gastroenterol Surg. 2016;49:819–26 (in Japanese with English abstract).
Gohrbandt AE, Hansen T, Ell C, et al. Portal vein leiomyosarcoma: a case report and review of the literature. BMC Surg. 2016;16:60.
Chiu WHK, Lo AW, Lee JK. Leiomyosarcoma of the portal vein: a case report and review of the literature. BJR Case Rep. 2016;3:20160125.
Gaignard E, Bergeat D, Stock N, et al. Portal vein leiomyosarcoma: a rare case of hepatic hilar tumor with review of the literature. Indian J Cancer. 2019;56:83–5.
Esposito F, Lim C, Baranes L, et al. Primary leiomyosarcoma of the liver: two new cases and a systematic review. Ann Hepatobiliary Pancreat Surg. 2020;24:63–7.
Tzedakis S, Jeddou H, Triki H, et al. Right hepatectomy with vascular and biliary reconstruction for a portal vein leiomyosarcoma. Ann Surg Oncol. 2021;28:1699.
Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–91.
Dzsinich C, Gloviczki P, van Heerden JA, et al. Primary venous leiomyosarcoma: a rare but lethal disease. J Vasc Surg. 1992;15:595–603.
Gage MJ, Newman E, Maldonado TS, et al. Leiomyosarcoma of the splenic vein. J Vasc Surg. 2012;55:1485–7.
Kevorkian J, Cento DP. Leiomyosarcoma of large arteries and veins. Surgery. 1973;73:390–400.
Killoran TP, Wells WA, Barth RJ, et al. Leiomyosarcoma of the popliteal vein. Skelet Radiol. 2003;32:174–8.
Funding
This work was supported by the Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital to HI (NFRCH 21-0012). The funder had no role in study design, data collection, data analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
HI was responsible for data collection, interpretation, and preparation of the manuscript. NY helped draft the manuscript. MO, HM, HN, and YY performed the diagnosis, surgery, and perioperative management of the patient. MF was responsible for pathological examination and diagnosis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Hiromitsu Imataki, Masataka Okuno, Hideo Miyake, Hidemasa Nagai, Yuichiro Yoshioka, Norihiro Yuasa, and Masahiko Fujino declare that they have no conflict of interest.
Ethical approval
All the procedures complied with the ethical standards of the responsible committees on human experimentation (institutional and national) and with the 2008 version of the Declaration of Helsinki.
Human rights
All the procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent for this report was obtained from the patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Imataki, H., Okuno, M., Miyake, H. et al. Portal vein leiomyosarcoma invading the pancreatic head. Clin J Gastroenterol 15, 484–492 (2022). https://doi.org/10.1007/s12328-022-01613-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-022-01613-9