Abstract
A 70-year-old man underwent endoscopy, which revealed a slightly depressed and elevated gastric cancer with suspected submucosal invasion of the mid gastric body. Biopsy specimens revealed differentiated tubular adenocarcinoma. We also detected lung and esophageal cancer and prioritized treatment of these lesions, and the patient underwent three endoscopies to monitor changes in gastric cancer. The tumor size and color remained unchanged; however, the marginal ridge was prominent, and the depressed area was deeper on subsequent evaluation. Total gastrectomy was performed 9 months after the first endoscopy. Histopathological examination of the resected specimens showed muscularis propria invasion, well-differentiated tubular adenocarcinoma involving the superficial mucosa, and tumor cells showing clear cytoplasm and a columnar or three-dimensional structure, between the deep mucosa and submucosa. The cells were immunopositive for Sal-like protein 4 and glypican 3; therefore, the patient was diagnosed with gastric adenocarcinoma with enteroblastic differentiation (GAED). This rare gastric cancer variant constituted approximately 70% of the entire lesion, and we observed significant lymphovascular invasion and lymph node metastasis. GAED is a rare histopathological subtype of gastric cancer described in recent years. Few cases of this tumor are reported to date; therefore, our study significantly contributes to the literature.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the 15th edition of the Japanese Classification of Gastric Carcinoma, gastric cancers that were functionally classified as alpha-fetoprotein (AFP)-producing gastric cancer are currently histopathologically classified as gastric adenocarcinoma with enteroblastic differentiation (GAED) or gastric hepatoid adenocarcinoma (HAC) [1]. Reportedly, GAED accounts for 2.2% of all gastric cancers [2]. GAED is histopathologically characterized by cells with glycogen-rich clear cytoplasm that structurally resemble fetal gastrointestinal epithelium. Diagnostic confirmation is based on immunohistochemical evaluation using a fetal gastrointestinal epithelial marker. Clinically, even early-stage GAED is a highly malignant tumor associated with venous and lymphatic invasion and liver metastasis [3, 4].
We report a case of GAED in a patient who was initially diagnosed with conventional differentiated gastric adenocarcinoma and underwent 8-month follow-up for the gastric malignancy while he was treated for other cancers. Endoscopic images obtained immediately preoperatively were compared with initial images; therefore, in our view, this report makes a significant contribution to the literature.
Case report
A 70-year-old man, who had a history of right lung cancer surgery at 66 years of age, underwent esophagogastroduodenoscopy (EGD) for the first time in 2 years for follow-up of Helicobacter pylori (HP) gastritis; HP eradication was not performed. A superficial depressed and elevated type gastric cancer was detected in the anterior wall of the greater curvature of the gastric body along with superficial depressed-type esophageal cancer. The gastric lesion measured 30 mm in size and was irregularly depressed with a reddish marginal ridge (Fig. 1a, b). Biopsy of resected gastric and esophageal cancer specimens revealed moderately to well-differentiated tubular adenocarcinoma and squamous cell carcinoma, respectively. Endoscopic ultrasonography performed with a 20 MHz ultrasonic probe revealed deep submucosal (SM) invasion of the gastric (Fig. 1c) and esophageal cancer. Computed tomography performed for detection of metastases revealed primary lung cancer involving the right upper lobe, therefore, we initially performed thoracoscopic right partial lung resection three months after initial EGD. Subsequently, the patient received combination chemoradiotherapy (CRT) comprising intravenous 5-fluorouracil and cisplatin with irradiation (70 Gy) for esophageal cancer five months after initial EGD (Fig. 2).
Initial endoscopic images showing findings of gastric cancer. a White light image showing a reddish lesion in the anterior wall of the midbody of the stomach. b Histopathological findings in an indigo carmine-stained specimen. c Narrowband imaging (NBI) did not reveal microvascular patterns, but irregular microsurface patterns were observed. However, we did not find anything specific in the NBI findings. d Endoscopic ultrasonography image showing a relatively uniform hypoechoic mass extending between the mucosa and the deep submucosa
While he was treated for esophageal and lung cancer, the patient underwent two EGDs over a period of 8 months prior to surgery to monitor gastric cancer; second EGD conducted five months after initial EGD and six days before the CRT for esophageal cancer, third EGD conducted 12 days before the surgery of gastric cancer. Endoscopy performed before the surgery revealed that the tumor was unchanged in size and color, although the marginal ridge was more prominent, and the depressed area was slightly deeper (Fig. 3a, b). We performed laparoscopic distal gastrectomy with D1+ (D1 plus) lymph node dissection and Billroth-I reconstruction for gastric cancer, 9 months after the patient underwent the first EGD (Fig. 4). We did not measure preoperative serum AFP levels.
Endoscopic images obtained 8 months after the first endoscopy showing findings of gastric cancer. a The image was observed using a white light imaging. b The image was observed in an indigo carmine-stained. c Narrowband imaging showed irregular microsurface patterns and irregular microvascular patterns
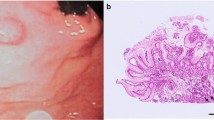
Histopathological examination of the resected specimens showed conventional differentiated tubular adenocarcinoma involving the mucosal surface, and special proliferating tumor cells extended between the deep mucosa and submucosa. These special tumor cells contained clear cytoplasm and formed columns and three-dimensional structures (Fig. 5a, b), suggesting features of GAED. Immunohistochemical evaluation showed that the cells were immunonegative for AFP, immunopostiive for sal-like protein 4 (SALL4, a fetal gastrointestinal epithelial marker), and partially immunopositive for glypican 3 (Fig. 6a-c). Based on these results, the patient was histopathologically diagnosed with GAED. The lesion invaded the muscularis propria with significant venous invasion and lymph node metastasis, and the clinical stage was confirmed as IIA. The patient was administered oral S-1 adjuvant chemotherapy. No recurrence was observed at his 5-month postoperative follow-up; however, the patient died of sepsis secondary to immunosuppression.
Histopathological findings of the resected lesion. a Loupe image of the gastric cancer. The GAED is visualized between the deep mucosa and submucosa (represented by black arrows). The surface of the lesion is covered with conventional differentiated adenocarcinoma. b Magnified image of the GAED component showing proliferating tumor cells with clear cytoplasm, arranged in columns and three-dimensional structures. GAED gastric adenocarcinoma with enteroblastic differentiation
Discussion
In this report, we describe a case of GAED, which was monitored by performing multiple endoscopic examinations before the definitive diagnosis was established, because the patient had lung cancer and esophageal cancer at the same time and was the last to be treated for it.
AFP-producing gastric cancer was first reported by Bourreille et al. [5] and accounts for 2.7–5.4% of all gastric cancers [6, 7]. This lesion is highly malignant and commonly metastasizes to lymph nodes or the liver [6,7,8,9,10]. This malignancy is diagnostically challenging because AFP-producing gastric cancer is not always associated with high serum AFP levels, and tumor cells do not always show positive results with AFP staining. Following the development of various immunohistochemical markers, gastric cancer that was functionally classified as AFP-producing gastric cancer is currently histopathologically classified as GAED and HAC, according to the 15th edition of the Japanese Classification of Gastric Carcinoma [1].
Matsunou et al. first coined the term GAED for an AFP-producing differentiated adenocarcinoma characterized by cells showing a glycogen-rich clear cytoplasm and structure resembling fetal gastrointestinal epithelium [11]. Subsequent studies reported that fetal gastrointestinal markers such as SALL4 and glypican three were useful to diagnose GAED [12,13,14]. Murakami et al. [4] reported that “GAED is an adenocarcinoma composed of cells resembling the fetal gastrointestinal epithelium, with a pale cytoplasm, with immunopositivity for AFP, glypican 3, or SALL4.” However, AFP production is not a prerequisite for the diagnosis of GAED; AFP production is observed in 45% of all GAED lesions [4].
GAED is considered as an aggressive cancer, similar to AFP-producing tumors and shows higher rates of lymphatic invasion (76% vs. 41%), venous invasion (72% vs. 31%), liver metastasis (31% vs. 6%), and lymph node metastasis (69% vs. 38%) compared with conventional differentiated adenocarcinoma [4]. Additionally, the mucosal surface of the GAED lesion is covered with a conventional differentiated adenocarcinoma component; therefore, endoscopic images are often indistinguishable from conventional differentiated adenocarcinoma. The clinicopathological findings of GAEDs reported previously and this case are shown in Table 1. In the present case, the mucosal surface of the lesion was covered by a conventional differentiated adenocarcinoma; therefore, GAED could not be diagnosed preoperatively. Moreover, the depth of invasion reported by previous studies is often lesser than the actual depth of invasion [3]. It is speculated that this is because a stromal reaction is unlikely to occur in the tumor; therefore, endoscopic softness remains. Notably, GAED often invades the underlying tissues deeper than the deep mucosa where a conventional differentiated adenocarcinoma component remains, and the percentage of GAED in one gastric cancer lesion was observed to be 30–90% [4]. Tumor cells were immunonegative for AFP in our case; however, significant lymphovascular invasion and lymph node metastasis were observed. Although the cancer invaded the muscularis propria, the area of invasion was not large. Nevertheless, severe lymphovascular invasion and lymph node metastasis were observed; these findings were consistent with a high-grade malignancy. A typical finding in this case was that the mucosal surface of the lesion showed a conventional differentiated adenocarcinoma component. With regard to the development and proliferation of GAED, Kinjo et al. [15] hypothesized that GAED might acquire AFP-producing ability from differentiated adenocarcinoma with intestinal-type mucin during invasion and proliferation. However, recent reports have described pure GAED without the conventional differentiated adenocarcinoma component [16], suggesting de novo development of GAED from the normal gastric mucosa. Moreover, as shown in Table 1, there was no clinical or pathological difference between AFP-negative and AFP-positive GAEDs. Further studies are warranted to gain a deeper understanding of the origin, growth, and morphology of this malignancy.
Regarding the treatment strategy of this case, the following discussion was held with the surgeon. First, there was a concern that subtotal esophagectomy and total gastrectomy, which involved the reconstruction of the jejunum or colon, would be highly invasive. The patient was also considered to be at higher risk for surgery because he was unable to stop drinking and smoking. Therefore, definitive chemoradiotherapy (dCRT) was selected as the treatment for the esophageal cancer, rather than surgery. Second, surgery of lung cancer after dCRT for the esophageal cancer was judged to have a high risk of respiratory complications. Third, dCRT for the esophageal cancer was prioritized over surgery for gastric cancer, with the expectation that chemotherapy might be effective for gastric cancer as well. However, this factor was based on the fact that we had diagnosed this lesion as a conventional differentiated adenocarcinoma with a tumor depth of up to SM, not GAED. Because of the poor prognosis of GAED, the treatment of gastric cancer should have been a priority if GAED could have been diagnosed in advance. Fortunately, the effect of chemotherapy might lead to the absence of significant changes in the endoscopic images of the GAED over eight-month-period.
In conclusion, we report a case of GAED, which could not be conclusively diagnosed preoperatively, and owing to comorbidities, endoscopic follow-up was performed for 8 months. GAED is often indistinguishable from conventional differentiated adenocarcinoma based on endoscopic images and biopsies. However, GAED has a poor prognosis. Therefore, further accumulation of cases describing GAED is essential for a better understanding of this malignancy.
References
The Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma. 15th ed. Tokyo: Kanehara; 2017.
Yao T, Akazawa Y, Murakami T, et al. HAC (hepatoid adenocarcinoma) and ACED (adenocarcinoma with enteroblastic differentiation). Stomach Intest. 2018;53:746–51 (in Japanese, abstract in English).
Matsumoto K, Ueyama H, Matsumoto K, et al. Clinicopathological features of alpha-fetoprotein producing early gastric cancer with enteroblastic differentiation. World J Gastroenterol. 2016;22:8203–10.
Murakami T, Yao T, Mitomi H, et al. Clinicopathologic and immunohistochemical characteristics of gastric adenocarcinoma with enteroblastic differentiation: a study of 29 cases. Gastric Cancer. 2016;19:498–507.
Bourreille J, Metayer P, Sauger F, et al. Existence of alpha fetoprotein during gastric-origin secondary cancer of the liver. Presse Med. 1970;78:1277–8.
Kono K, Amemiya H, Sekikawa T, et al. Clinicopathologic features of gastric cancers producing alpha-fetoprotein. Dig Surg. 2002;19:359–65.
Chang YC, Nagasue N, Abe S, et al. Comparison between the clinicopathologic features of AFP-positive and AFP-negative gastric cancers. Am J Gastroenterol. 1992;87:321–5.
Li XD, Wu CP, Ji M, et al. Characteristic analysis of α-fetoprotein-producing gastric carcinoma in China. World J Surg Oncol. 2013;11:246.
Adachi Y, Tsuchihashi J, Shiraishi N, et al. AFP-producing gastric carcinoma: multivariate analysis of prognostic factors in 270 patients. Oncology. 2003;65:95–101.
Chang YC, Nagasue N, Kohno H, et al. Clinicopathologic features and long-term results of alpha-fetoprotein-producing gastric cancer. Am J Gastroenterol. 1990;85:1480–5.
Matsunou H, Konishi F, Jalal RE, et al. Alpha-fetoprotein-producing gastric carcinoma with enteroblastic differentiation. Cancer. 1994;73:534–40.
Ushiku T, Uozaki H, Shinozaki A, et al. Glypican 3-expressing gastric carcinoma: distinct subgroup unifying hepatoid, clear cell, and a-fetoprotein-producing gastric carcinomas. Cancer Sci. 2009;100:626–32.
Ushiku T, Shinozaki A, Shibahara J, et al. SALL4 represents fetal gut differentiation of gastric cancer, and is diagnostically useful in distinguishing hepatoid gastric carcinoma from hepatocellular carcinoma. Am J Surg Pathol. 2010;34:533–40.
Ikeda H, Sato Y, Yoneda N, et al. α-Fetoprotein-producing gastric carcinoma and combined hepatocellular and cholangiocarcinoma show similar morphology but different histogenesis with respect to SALL4 expression. Hum Pathol. 2012;43:1955–63.
Kinjo T, Taniguchi H, Kushima R, et al. Histologic and immunohistochemical analyses of a-fetoprotein- producing cancer of the stomach. Am J Surg Pathol. 2012;36:56–655.
Yamada R, Horiguchi SI, Onishi T, et al. Early gastric cancer with purely enteroblastic differentiation and no conventional adenocarcinoma component. Case Rep Pathol. 2018;28:3620293.
Yamamura Y, Muto J, Kuroda A, et al. A case of multiple gastric cancer with duplicate histological types. J Japn College Surg. 2013;38:795–800.
Yube Y, Ishibashi Y, Kohira Y, et al. Two cases of primary gastric adenocarcinoma with enteroblastic differentiation (GAED). J Japn Soc Clin Surg. 2017;78:2652–7.
Ikezawa N, Tanaka S, Kaku H, et al. Early gastric cancer involving a pure enteroblastic differentiation component that was curatively resected via endoscopic submucosal dissection. Clin J Gastroenterol. 2020;13:512–6.
Acknowledgments
We wish to express our sincere gratitude and deep appreciation to Dr. Shinji Ohki, Dr. Suguru Hayase, Dr. Hisashi Onozawa, Dr. Hiroyuki Hanayama, Dr. Yohei Watanabe, Dr. Yasuyuki Kanke, Dr. Takuro Matsumoto, Dr. Hiroshi Nakano, Dr. Eisei Endo, Dr. Jun Wada for their assistance with surgical procedures and postoperative patient management in this case, to Prof. Yuko Hashimoto and Dr. Erina Suzuki for their assistance with histopathological evaluation, and to all medical staff at the endoscopy department for their assistance with endoscopic procedures.
Author information
Authors and Affiliations
Contributions
The conception and design of this report were carried out by TK and TH. Endoscopic procedures and patient management were performed by TK, TH, JN, MH, TK, TT, RS, MS, MT, YS, HI, and RK. Surgical operation was performed by ZS and KK. The first draft of the manuscript was written by TK and TH. MK and HO advised on the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Tomoya Kimura, Takuto Hikichi, Jun Nakamura, Mika Takasumi, Minami Hashimoto, Tsunetaka Kato, Ryoichiro Kobashi, Tadayuki Takagi, Rei Suzuki, Mitsuru Sugimoto, Yuki Sato, Hiroki Irie, Zenichiro Saze, Masao Kobayakawa, Koji Kono and Hiromasa Ohira declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from this patient for being included in the paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kimura, T., Hikichi, T., Nakamura, J. et al. Gastric adenocarcinoma with enteroblastic differentiation followed endoscopically: A case report. Clin J Gastroenterol 13, 1074–1082 (2020). https://doi.org/10.1007/s12328-020-01220-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-020-01220-6