Abstract
The pathophysiology of intraductal papillary neoplasm of the bile duct (IPNB) remains unclear. We report a case of a Japanese man in his 70s with this disease, which we first diagnosed as a liver cyst. The patient was followed at our hospital for a 10-mm liver cyst and a 10-mm pancreatic cyst for 4 years. Four years later, tumor markers including CA19-9 were elevated in his blood tests. Abdominal ultrasonography showed a heterogeneous hyper-echoic mass with an anechoic area, 25 × 25 mm, in the S2 liver segment and showed posterior echo enhancement. Contrast-enhanced computed tomography showed that the tumor was gradually enhanced slightly. Magnetic resonance imaging showed a lesion of T1 low, T2 high around the cyst. Endoscopic retrograde cholangiopancreatography did not show an abnormality, including findings of the duodenal papilla. We suspected an IPNB and performed left lobe hepatectomy. The resected whitish tumor around the cyst was 25 × 23 mm. The tumor contained an intraductal papillary mass with an adjacent invasive adenocarcinoma. The papillary mass with fine vascular cores was lined by foveolar-type epithelium. Our diagnosis was IPNB with invasive adenocarcinoma. This case indicates that IPNB should be considered in the differential diagnosis of liver cysts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
IPNB (intraductal papillary neoplasm of the bile duct) is classified as a precancerous lesion in the WHO (World Health Organization) 2010 classification. The 2010 WHO classification states that IPNBs are characterized by dilated bile ducts filled with a papillary or villous biliary neoplasm covering delicate fibrovascular stalks [1,2,3]. However, cases of IPNB are rare, and disease characteristics are still unclear. There are few reports about the natural history of IPNB. We experienced a case of cystic IPNB that had been observed for 4 years. We report a case of a Japanese man in his 70s with this disease, which we first diagnosed as a liver cyst 4 years ago.
Case report
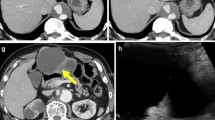
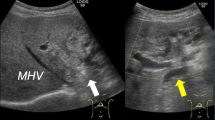
The patient was a man in his 70s. He had been followed at our hospital for a 10-mm liver cyst and a 10-mm pancreatic tail cyst for 4 years. He underwent gastrectomy for gastric cancer 13 years prior, and he had smoked 15 cigarettes/day since the age of 30 years. He had no history of drinking alcohol and no family history of cancer. He was 163 cm tall and weighed 64 kg. His blood pressure was 113/69 mmHg, and his pulse was 75 beats/min. He had neither anemia nor jaundice, and he had no abdominal pain. The tumor marker CA19-9 was elevated to 165.5 U/ml from the normal range in his blood tests. No other abnormalities were apparent on blood tests. Abdominal ultrasonography (US) showed a heterogeneous hyper-echoic mass with an anechoic area, 25 × 25 mm, in the S2 liver segment and showed posterior echo enhancement (Fig. 1). Contrast-enhanced computed tomography (CT) showed that the tumor was gradually enhanced slightly and the inside of tumor was stronger in the contrast effect than the periphery (Fig. 2). Magnetic resonance imaging (MRI) showed a lesion of T1 low, T2 high around the cyst. Contrast-enhanced MRI showed that the tumor was gradually enhanced slightly. The tumor was a multilocular cystic lesion with septa including solid parts. The border of the tumor was relatively clear (Fig. 3). Endoscopic retrograde cholangiopancreatography (ERCP) did not show an abnormality, including findings of the duodenal papilla. The bile cytology diagnosis was negative (Fig. 4). We suspected the tumor as a cystic tumor from the findings of T2-weighted MRI. It was thought that the pattern of contrast effect in the tumor expressed the density of cystic tumor cells or part of liver invasion. We suspected existence of fibrovascular stalks from septa findings in T2-weighted MRI. We suspected IPNB from various imaging findings and performed left lobe hepatectomy. The resected whitish tumor around the cyst was 25 × 23 mm (Fig. 5). The tumor contained a high-grade dysplastic intraductal papillary mass with an adjacent invasive adenocarcinoma. A part of the tumor contained low-grade dysplasia. The papillary mass with fine vascular cores was lined by foveolar-type epithelium. Our diagnosis was IPNB with invasive adenocarcinoma. The tumor had liver invasion about 7 mm (arrow). The surgical margin was negative (Fig. 6). Final pathological stage was T2, N0, M0, stage II. The postoperative course was good; the patient was discharged and has been followed in the outpatient department. This patient has had a 25 mm recurrence to the S6 liver segment 34 months after surgery. US showed a hyper-echoic mass, 25 × 25 mm, in the S6 liver segment (Fig. 7). MRI showed a lesion of T1 low, T2 high in the S6 liver segment. The tumor had septa (Fig. 8). There were not lymph node and distal organ metastases. We diagnosed the intrahepatic recurrence tumor as stage N0, M0. He received first-line chemotherapy with S1 and second-line chemotherapy with gemcitabine, and is currently alive after a recurrence in 12 months.
Magnetic resonance imaging (MRI) showed a lesion of T1 low (arrow) (a), T2 high around the cyst (arrow) (b). Contrast-enhanced MRI showed that the tumor was gradually enhanced slightly. The tumor was a multilocular cystic lesion with septa including solid parts. The border of the tumor was relatively clear (c)
The tumor contained a high-grade dysplastic intraductal papillary mass with an adjacent invasive adenocarcinoma. A part of the tumor contained low-grade dysplasia. The papillary mass with fine vascular cores was lined by foveolar-type epithelium. The tumor had liver invasion about 7 mm (arrow) (HE staining, ×4) (a), (HE staining, ×10) (b), (HE staining, ×20) (c), (HE staining, ×10) (d)
Discussion
Chen and Nakanuma pointed out that intraductal papillary growth of neoplastic biliary epithelia with a fine fibrovascular stalk (intraductal papillary neoplasia of the liver) resembling an intraductal papillary mucinous neoplasm of the pancreas is occasionally associated with hepatolithiasis [4]. In the WHO 2010 classification, IPNB was defined as a precancerous lesion. IPNB is characterized by dilated bile ducts that are filled with noninvasive papillary or villous biliary neoplasms covering delicate fibrovascular stalks. IPNB has been increasingly recognized as a unique type of biliary neoplasm. However, IPNB has a variety of presentations, and its clinical features are not well understood [1,2,3].
Nakanuma and colleagues reported on type 1 IPNB (classical IPNB) and Type 2 IPNB (so-called papillary carcinoma or cholangiocarcinoma) in 2018. The location of type 1 IPNB is intrahepatic, and type 2 IPNB is extrahepatic. Gross mucin of type 1 IPNB is common (approximately 80%) and of type 2 is rare (approximately 10%). With regard to histological architecture, type 1 IPNB has well-organized papillary growth with thin fibrovascular stalks, and type 2 IPNB has complex papillary growth with thick papillae or irregular branching with fine fibrovascular cores. For the incidence of associated invasive cancer, type 1 IPNB is approximately 50%, and type 2 IPNB is > 90%. In their report, they note an issue related to differentiation between type 2 IPNB and ordinary bile duct cancers. The discrimination between the two may not be clear in some cases [1].
On the other hand, IPNB shows various imaging findings, and there is a report about prognosis according to classification in various forms. The classification of IPNB was based on preoperative imaging and the pathological findings of surgical specimens. IPNBs were categorized into 5 classes: Class I—classical intrahepatic IPNB (i.e., presence of an intraductal tumor with unilateral intrahepatic duct dilatation); Class II—extrahepatic IPNB (i.e., presence of an intraductal tumor with bilateral intrahepatic duct dilatation); Class III—cystic variant (i.e., cystic tumor with a papillary tumor inside and presence of bile duct communication); Class IV—micro-papillary lesion (i.e., disproportional bile duct dilatation in the absence of any discernible tumor); and Class V—macroinvasion (i.e., presence of a mass-forming tumor incorporated with an intraductal tumor). The proposed classification predicted survival very well (p < 0.001). For patients with Class III and IV tumors, there were no tumor-related deaths within 3 years of surgery, and the median survival time was not reached during the follow-up period. The respective median survival time for Class I, II and V was 1888 (95% CI 1118–2657) days, 673 (95% CI 392–953) days, and 578 (95% CI 285–870) days. That report mentioned that this classification not only provides a view of the nature of the patients in terms of their radio-pathologic status, but also guides the planning of surgical procedures. The cystic variant of IPNB and the micro-papillary lesions have a better prognosis and lower rate of malignancy than the classical intrahepatic intraductal IPNB, whereas the extrahepatic intraductal mass and the intrahepatic macro-invasive lesions are more aggressive in nature [5]. Our case was equivalent to Class V. Our case experienced recurrence 34 months after surgery and had a poor prognosis. Therefore, we thought that this classification was useful for the prediction of prognosis for IPNB.
It is also very important to differentiate the subtype of IPNB because the prognosis is different according to its subtype. It has been reported that histologically, there are four subtypes: pancreaticobiliary, intestinal, gastric and oncocytic and patients with pancreaticobiliary type have significantly worse survival compared to those with gastric and intestinal types. Immunohistochemical (IHC) stainings such as MUC expression are characteristic markers for the IPNB subtypes [6]. But we did not perform IHC staining in this case, diagnosed this case as IPNB from hematoxylin–eosin (HE) staining and could not diagnose its subtype. In the future, we think that we should make an effort to perform IHC stain as much as possible for the accurate diagnosis of IPNB.
Few studies have investigated the long-term outcomes and recurrence patterns of surgically resected IPNB. The long-term outcomes of surgically resected IPNB have recently been reported, and the 5-year overall survival rate ranged from 47.0–82.0%. R1 resection, invasive carcinoma, extraductal invasion, lymphovascular invasion, lymph node metastasis, positivity for MUC1, and positivity for carcinoembryonic antigen (CEA) have been reported to be poor prognostic factors after surgical resection of IPNB. IPNB that includes invasive carcinoma carries a risk of recurrence similar to that of bile duct cancer. Mucus production can occur after surgical resection, even if no malignant IPNB tissue remains [7].
Our case had an intrahepatic IPNB, and the surgical margin was negative. However, our case experienced recurrence in the liver parenchyma 34 months after surgery. It has been reported that IPNB has high recurrence rate after surgery. It has been also reported that intraductal visible mass, tumor size ≥ 2.5 cm, multiplicity of the tumor, bile duct wall thickening, and adjacent organ invasion were recurrence risk factor of IPNB. This case was IPNB with the liver invasion about 7 mm. It was thought that this case had high potential of recurrence [8]. Therefore, we diagnosed S6 liver lesion as the recurrence of IPNB. We should observe the progress of patients very carefully after surgery for IPNB. We suggested a surgery to remove the recurrent IPNB lesion, but the patient did not provide consent, so we treated him with chemotherapy with S1 and gemcitabine. There are few reports regarding chemotherapy for IPNB recurrence, and more cases are expected in the future. In addition, this case was diagnosed initially as a liver cyst. We should consider IPNB as a differential diagnosis. This case showed imaging changes to invasive carcinoma from cystic IPNB (Fig. 9), and we feel that this case provides valuable information. Our case was diagnosed as a liver cyst 4 years ago. We could get the natural course of cystic IPNB that the lesion develops gradually and progress to IPNB with liver invasion in the course of 4 years. There are few reports about the natural history of IPNB. Therefore, we think that our case is valuable. Periodic follow-up may be desirable for the liver cyst even small size because liver cystic lesions may be IPNB such as this case. The establishment of the appropriate follow-up method of the liver cystic lesion is expected in the future by the accumulation of this disease.
In conclusion, this case indicates that IPNB should be considered in the differential diagnosis of liver cysts. This report that shows natural history of cystic IPNB is valuable.
References
Nakanuma Y, Jang KT, Fukushima N, et al. A statement by the Japan-Korea expert pathologists for future clinicopathological and molecular analyses toward consensus building of intraductal papillary neoplasm of the bile duct through several opinions at the present stage. J Hepatobiliary Pancreat Sci. 2018;25:181–7.
Wu X, Li B, Zheng C, et al. Intraductal papillary neoplasm of the bile duct: a single-center retrospective study. J Int Med Res. 2018;46:4258–68.
Tan Y, Milikowski C, Toribio Y, et al. Intraductal papillary neoplasm of the bile ducts: a case report and literature review. World J Gastroenterol. 2015;21:12498–504.
Chen TC, Nakanuma Y, Zen Y, et al. Intraductal papillary neoplasia of the liver associated with hepatolithiasis. Hepatology. 2001;34:651–8.
Luvira V, Somsap K, Pugkhem A, et al. Morphological classification of intraductal papillary neoplasm of the bile duct with survival correlation. Asian Pac J Cancer Prev. 2017;18:207–13.
Kim KM, Lee JK, Shin JU, et al. Clinicopathologic features of intraductal papillary neoplasm of the bile duct according to histologic subtype. Am J Gastroenterol. 2012;107:118–25.
Hokuto D, Nomi T, Yasuda S, et al. Long-term observation and treatment of a widespread intraductal papillary neoplasm of the bile duct extending from the intrapancreatic bile duct to the bilateral intrahepatic bile duct: a case report. Int J Surg Case Rep. 2017;38:166–71.
Lee S, Kim MJ, Kim S, et al. Intraductal papillary neoplasm of the bile duct: assessment of invasive carcinoma and long-term outcomes using MRI. J Hepatol. 2018. https://doi.org/10.1016/j.jhep.2018.12.005.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Human/animal rights
All the procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from the patient for being included in this report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fujii, M., Okamoto, Y. & Shiode, J. A case of cystic intraductal papillary neoplasm of the bile duct with associated adenocarcinoma. Clin J Gastroenterol 13, 219–224 (2020). https://doi.org/10.1007/s12328-019-01040-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-019-01040-3