Abstract
The patient was a 70-year-old woman in whom examination revealed a high level of carbohydrate antigen 19-9. Abdominal ultrasonography and computed tomography (CT) revealed a multilocular cystic lesion compressing the gallbladder. CT indicated the presence of a multilocular cystic tumor (67 × 68 × 72 mm) in contact with the right hepatic lobe. Intraoperative findings indicated that the cyst diameter was 8.5 × 6.0 cm, and the cyst was continuous with the gallbladder. The gallbladder was resected along with the cyst. The cyst was multilocular and originated from the cystic duct and gallbladder wall. The cyst wall contained cuboidal to columnar mucin-producing epithelial cells and ovarian-like stroma (OS). The final diagnosis was mucinous cystic neoplasm (MCN) of the gallbladder with low-grade dysplasia. In the 2010 WHO classification of tumors of the digestive system, MCN have been newly defined as a type of hepatobiliary tract epithelial neoplasms. MCN of the gallbladder with OS is extremely rare. Only three cases have been published in the literature. The presence of OS is necessary for diagnosis of MCN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization (WHO) classification of digestive system tumors was revised in 2010, and mucinous cystic neoplasms (MCN) have been newly defined as a type of hepatobiliary tract epithelial neoplasms. Biliary MCNs have recently been defined as a subset of the previously known biliary cystadenoma/cystadenocarcinoma category [1, 2]. Biliary cystadenomas/cystadenocarcinomas usually occur in the liver. Moreover, a MCN of the gallbladder is a cystic lesion resembling a similar lesion of the pancreas, which produces mucins and shows an ovarian-like stroma (OS) [2]. Few reports have described MCNs of the gallbladder that demonstrate OS [3, 4]. We report an extremely rare case of a patient who presented with a gallbladder tumor that was diagnosed as a MCN with OS.
Case report
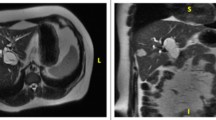
A 70-year-old woman was treated by a local physician for a high level of carbohydrate antigen 19-9 (CA19-9, 46.9 U/mL), which was detected during examination. She was asymptomatic with an unremarkable medical and family history. Abdominal ultrasonography and computed tomography (CT) revealed a multilocular cystic lesion compressing the gallbladder, and the patient was referred to Yamagata University Hospital. Examination upon admission did not reveal abdominal tenderness or the presence of a palpable mass. Biochemical blood tests revealed a mildly increased CA19-9 level (38.7 U/mL, reference range 0–37 U/mL). Abdominal ultrasonography revealed a multilocular cyst located in the right upper abdominal wall (50 mm in diameter with septation). Endoscopic ultrasonography indicated that the cyst that was compressing the gallbladder neck contained a 3-mm septation within its cavity (Fig. 1). No clear communication was identified between the cyst and the gallbladder. The common bile duct measured approximately 8 mm in diameter, and no intraductal cholelith or stenosis was noted. We noted cholelithiasis and diffuse thickening of the gallbladder wall. Selective contrast enhancement of the common bile duct could not be performed using endoscopic retrograde cholangiopancreatography, and dilatation of the ampulla of Vater was not observed. CT indicated the presence of a multilocular cystic tumor (67 × 68 × 72 mm) in contact with the right hepatic lobe. The gallbladder was ventrally compressed by the cyst, and cholelithiasis was noted (Fig. 2). Magnetic resonance imaging revealed that the cyst protruded inferiorly from the liver (segment 5), and the cystic contents showed an isosignal with water without solid components (Fig. 3). Based on the results of the above-mentioned evaluation, we suspected a biliary cystadenoma of the liver (segment 5). Preoperatively, our surgical plan included performing a cholecystectomy, right hepatic lobectomy, bile duct resection, as well as segmentectomies of the liver depending upon the extent of tumor infiltration.
Intraoperatively, we observed that the cyst was continuous with the gallbladder and measured 8.5 × 6.0 cm in diameter. The cyst was attached by loose connective tissue and could be easily dissected away from the liver. The cyst was observed to be compressing the common bile duct to the left without any invasion into the surrounding region. A small amount of ascites was observed, and cytological examination was negative for cancer. The cyst was attached only to the gallbladder; thus, the gallbladder was resected along with the cyst. The specimen weighed 179 g, and intraoperative histopathological examination of the cystic duct showed findings negative for cancer. Imaging of the excised gallbladder revealed no communication between the gallbladder and the cyst (Fig. 4).
Of note, 130 mL of milky white cystic fluid was obtained, and cytological examination revealed that the cystic fluid could be classified as class II. Macroscopically, the cystic fluid did not resemble typical mucin, as would be observed in intraductal papillary mucinous neoplasms or pancreatic MCNs and appeared to be serous in nature. Biochemical examination of the cystic fluid revealed that the total bilirubin and pancreatic amylase levels were within the reference range. However, the carcinoembryonic antigen (CEA) and CA19-9 levels were high (149.6 ng/mL and 404.5 U/mL, respectively) (Fig. 5).
Macroscopic and histopathological findings of the resected specimen have been shown in Fig. 6. The multilocular cyst was observed to originate from the cystic duct and the gallbladder wall. The wall of the cyst was lined by cuboidal to columnar mucin-producing epithelial cells, which demonstrated low-grade dysplasia. Furthermore, no severe papillary hyperplasia and remarkable mucin production was noted. Additionally, most portions of the cyst wall showed OS (estrogen receptor negative, progesterone receptor positive). Based on these findings, she was diagnosed with a MCN of the gallbladder with low-grade dysplasia. To date (8 years postoperatively), no recurrence has been observed. To date, only 1 case of a MCN of the gallbladder has been observed at our institution.
a The resected specimen shows a multilocular cyst originating from the gallbladder and the cystic duct. b Most segments of the cystic wall contain ovarian-like stroma. c The cyst is lined by a single layer of mucin-producing epithelial cells showing low-grade dysplasia. d Immunohistochemical assessment shows positive staining for progesterone receptors in the ovarian-like stroma
Discussion
MCN is a mucin-producing cystic tumor that typically demonstrates the following features: it usually develops in the pancreas, is commonly observed in middle-aged women, it does not communicate with the pancreatic duct, and is characterized by the presence of OS [5, 6]. Based on the revised 2010 WHO classification of tumors of the digestive system, MCNs have been newly defined as hepatobiliary tract epithelial neoplasms. The previously accepted biliary cystadenoma/cystadenocarcinoma classification has recently been revised to define these lesions as MCNs and intraductal papillary neoplasms of the bile duct (IPNB). Notably, lesions demonstrating OS are defined as MCNs and those without OS, which communicate with the bile duct, are defined as IPNB [1, 2]. Although the etiology and incidence of biliary MCNs remain unknown, the clinical characteristics of these tumors resemble those of pancreatic MCNs.
We treated a middle-aged woman in whom the cyst wall of the MCN was lined by mucin-producing columnar epithelial cells, histopathologically showed the presence of OS, and no communication was noted between the cyst and the gallbladder. Thus, this patient was diagnosed with a MCN of the gallbladder.
Simmons et al. first reported a biliary cystadenoma of the gallbladder in 1989 [7]. The occurrence of a biliary cystadenoma in the gallbladder is rarer than that in the liver. A PubMed search for the keywords “biliary cystadenoma of the gallbladder” and “mucinous cystic neoplasm of the gallbladder” between 1977 and 2017 revealed 10 reports published in English [3, 4, 7,8,9,10,11,12,13,14]; however, only 3, including ours reported the presence of OS in the lesion. The details pertaining to our literature search have been presented in Table 1. A case study reported by Spector et al. in 2003 described a tumor that developed in the lumen of the gallbladder and progressed into the common bile duct causing jaundice [3]. Furthermore, in 2014, Zevallos et al. described a patient who presented with jaundice secondary to a tumor in the gallbladder lumen [4]. Both patients were diagnosed with a MCN of the gallbladder with OS, which was confirmed following immunohistochemical evaluation for estrogen receptors. All patients were women, and no malignancy was reported in any patient. Unlike the 2 previously reported patients, our report is unique because the patient presented with a MCN that developed on the serosal aspect of the gallbladder, she was asymptomatic and did not present with jaundice. When a MCN occurs in the gallbladder lumen, (as was observed in the 2 patients who showed jaundice), it tends to obstruct the bile flow. Therefore, a MCN of the gallbladder may be classified as an intracystic growth type, which causes jaundice, or an extracystic growth type, which is usually asymptomatic.
Based on the revised 2010 WHO classification of tumors of the digestive system, the presence of OS is a prerequisite to diagnose MCN. Currently, a mucin-producing cyst without OS is classified as IPNB with high mucin production [15]. Previous reports that have described cystadenomas of the gallbladder have included reports without any mention of OS—these tumors were likely to have been IPNB. However, Mano et al. have indicated that it is difficult for imaging modalities and histopathological analyses to conclusively demonstrate bile duct communication, and that the definition and definitive character of OS remains unclear. They indicated the possibility of MCN without OS and IPNB without bile duct communication [16].
In our patient, histopathological examination of the specimen showed flat mucin-producing epithelial cells, without severe papillary hyperplasia and remarkable mucin production. Macroscopically, the cystic fluid did not typically resemble mucin, as is observed in IPMN or pancreatic MCN, and was of a serous nature. Notably, in regard to this observation, based on the revised 2010 WHO classification of tumors of the digestive system, fluid obtained from biliary MCNs is described as mucinous or serous, and the presence or absence of mucin in the fluid dose not affect the definition [2]. Although MCN includes the term “mucinous,” the presence of mucin is not important to define MCNs. Considerable controversy and variability persists regarding the nomenclature of MCN. It has been reported that mucin production is observed in approximately one-thirds of IPNB lesions [1], whereas the remaining two-thirds of these tumors do not contain mucin. Therefore, IPNB and biliary MCN may need to be further classified based on the presence/absence of mucin. However, presently, these disease entities are rarer than pancreatic IPMN and MCN; thus, additional cases studies are needed in future in this context.
References
Nakanuma Y, Curabo MP, Franceschi S, et al. Intrahepatic cholangiocarcinoma. In: Bosman FT, Carneiro F, Hruban RH, et al., editors. WHO classification of tumours of the digestive system; World Health Organization of Tumours. 4th ed. Lyon: IARC; 2010. p. 217–24.
Albores-Saavedra J, Adsay NV, Crawford JM, et al. Carcinoma of the gallbladder and extrahepatic bile ducts. In: Bosman FT, Carneiro F, Hruban RH, et al., editors. WHO classification of Tumours of the digestive system; World Health Organization of Tumours. 4th ed. Lyon: IARC; 2010. p. 266–73.
Spector SA, Fernandez VE, Vernon SE, et al. Gallbladder cystadenoma and common bile duct obstruction. Int J Gastrointest Cancer. 2003;34:151–5.
Zevallos QJC, Jiménez AR, Garmendi IM, et al. Mucinous cystic neoplasm of the gallbladder obstructing the common bile duct, a rare entity with a new name. Cir Esp. 2014;92:567–9.
Compagno J, Oertel JE. Mucinous systic neoplasms of the pancreas with overt and latent malignancy (cystadenocarcinoma and cystadenoma). A clinicopathologic study of 41 cases. AM J Clin Pathol. 1978;69:573–80.
Yamao K, Yanagisawa A, Takahashi K, et al. Clinicopathological features and prognosis of mucinous cystic neoplasm with ovarian-type stroma: a multi-institutional study of the Japan Pancreas Society. Pancreas. 2011;40:67–71.
Simmons TC, Miller C, Pesigan AM, et al. Cystadenoma of the gallbladder. Am J Gastroenterol. 1989;84:1427–30.
Devaney K, Goodman ZD, Ishak KG. Hepatobiliary cystadenoma and cystadenocarcinoma: a light microscopic and immunohistochemical study of 70 patients. Am J Surg Pathol. 1994;18:1078–91.
Terada T, Takeuchi T, Taniguchi M. Hepatobiliary cystoadenocarcinoma with cystadenoma elements of the gallbladder in an old man. Pathol Int. 2003;53:790–5.
Rooney TB, Schofer JM, Stanley MD, et al. Biliary cystadenoma of the gallbladder. AJR Am J Roentgenol. 2005;185:1571–2.
Waldmann J, Zielke A, Moll R, et al. Cystadenocarcinoma of the gallbladder. J Hepatobiliary Pancreat Surg. 2006;13:594–9.
McCague A, Rosen M, O’Malley K. Laparoscopic cholecystectomy of a polypoid gallbladder cystadenoma obstructing the common bile duct. Surg Laparosc Endosc Percutan Tech. 2008;18:209–12.
Sistla SC, Sankar G, Basu D, et al. Biliary cystadenocarcinoma of the gall bladder: a case report. J Med Case Rep. 2009;3:75.
Gokalp G, Dusak A, Topal NB, et al. Cystadenoma originating from the gallbladder. J Ultrasound Med. 2010;29:663–6.
Fukuo Kondo. Pathology of epithelial tumors of bile duct: diagnostic criteria and their problems. J Jpn Biliary Assoc. 2013;27:680–8.
Mano Y, Aishima S, Fujita N, et al. Cystic tumors of the liver: on the problems of diagnostic criteria. Pathol Res Pract. 2011;207:659–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shuichiro Sugawara, Ichiro Hirai, Toshihiro Watanabe, Koji Tezuka, and Wataru Kimura declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Sugawara, S., Hirai, I., Watanabe, T. et al. A case of mucinous cystic neoplasm of the gallbladder. Clin J Gastroenterol 11, 428–432 (2018). https://doi.org/10.1007/s12328-018-0850-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-018-0850-8