Abstract
Neuroendocrine neoplasms, including neuroendocrine tumors (NETs) and neuroendocrine carcinomas (NECs), are rare epithelial tumors with a predominant neuroendocrine differentiation. Compared with NETs, NECs have been reported to be rarer and have a poorer prognosis. We present a rare case of small bowel NEC diagnosed using double-balloon endoscopy (DBE) and the long-term survival accomplished via intensive therapy. DBE revealed an ulcerative tumor in the deep jejunum, and biopsy specimens showed large and highly dysplastic tumor cells; immuno-histological synaptophysin and chromogranin A tests were positive, and the Ki-67 index was more than 90%. Partial intestinal resection without complete lymph node dissection was performed and, postoperatively, chemotherapy was administered. The patient was observed for 3 years after chemotherapy, and complete remission was maintained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasms (NENs) are fairly rare epithelial tumors with a predominant neuroendocrine differentiation [1]. In 2010, the WHO presented a new classification of NENs, where the term NENs described all tumors with a neuroendocrine differentiation. Furthermore, neuroendocrine tumors (NETs) and neuroendocrine carcinomas (NECs) were graded into three types, grades 1 (G1), 2 (G2) and 3 (G3), according to different definitions of proliferation using the mitotic count and/or the Ki-67 index [2, 3]. In general, both G1 and G2 NENs are considered as NETs, and G3 NENs are considered as NECs. Among all cases of NENs, NECs were reported at a lower frequency in comparison to NETs and they were associated with a poorer prognosis [4, 5].
We present a rare case of small bowel NEC diagnosed via double-balloon endoscopy (DBE), and the long-term survival accomplished with intensive therapy.
Case report
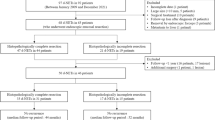
A 65-year-old healthy gentleman had been aware of general fatigue and tarry stool for the previous 2 months. He was admitted to the previous hospital and presented with severe anemia. He had no abnormal findings detectable via esophagogastroduodenoscopy and colonoscopy. Conversely, increased wall thickness of the jejunum and mesenteric lymph node swelling were detected on abdominal computed tomography (CT) scans, and he was suspected to have a small intestinal malignant tumor. Thus, he was referred to our hospital for further investigation. He had a hard mass without tenderness, almost the same size as an egg, in the left lower abdomen.
Laboratory findings revealed severe iron deficiency anemia, but his tumor markers were normal (Table 1). Abdominal CT revealed irregular wall thickness (approximately, 50 mm in size) with multiple mesenteric lymph node swellings (Fig. 1a, b).
DBE, via the per-oral approach, revealed elevated lesion like a submucosal tumor with ulceration in the deep jejunum (Fig. 2). The tumor was elastic hard and about 50 mm in size with a white thick coating and coagula at the surface. An ulcer mound could not be observed clearly, and the border line between the tumor and normal mucosa was clear and sharp. Therefore, GIST was first suspected, rather than carcinoma.
Biopsy specimens obtained via DBE showed large and highly dysplastic tumor cells, which proliferated with an alveolar structure. Immuno-histological synaptophysin and chromogranin A tests were positive, and his Ki-67 index was more than 90% (Fig. 3). According to the above histological results, this patient was diagnosed with neuroendocrine carcinoma originating from the small intestine. Finally, stage III small intestinal NEC (as per the clinical staging according to AJCC/UICC 2017) [6] was diagnosed. After DBE, capsule endoscopy was performed and total small intestine was observed. No other lesion was detected.
Partial intestinal resection without complete lymph node dissection was performed to control continuous anemia (Fig. 4), and postoperatively chemotherapy using CDDP 90 mg/m2 and VP-16 70 mg was administered. No severe side effects were caused by chemotherapy, and after the completion of 10 courses, complete remission (CR) was accomplished (Fig. 5). Follow up CT every six months has been performed after chemotherapy, and CR has been maintained.
Discussion
Small intestinal adenocarcinomas, the most common histological subtype of small bowel malignant tumors, are rare, accounting for 3–5% of all gastrointestinal tumors [7], and small intestinal NENs are regarded as even rarer. Ito et al. reported that the incidence rate of GI-NETs in 2010 was estimated to be 3.51 per 100,000 people, and mid-gut tumors in this group were only 0.15 [8]. Furthermore, small intestinal NECs are considered as extremely rare. Yamaguchi et al. reported that the ratio of mid-gut origin tumors was 2% (6/258) in all gastrointestinal and pancreatic NECs [9].
On the other hand, in all NENs, NECs were reported to be rarer and as having a poorer prognosis than NETs because of rapid growth development, metastasis, and recurrence. Xianbin et al. reported 168 gastroenteropancreatic NENs, and among them small intestine NETs only consisted of 5 cases and no NECs were included [5]. They also revealed that tumor type was the only independent prognostic factor for overall survival.
Several clinical case reports regarding small intestinal NECs were diagnosed by DBE or video capsule endoscopy (VCE). However, their endoscopic findings in detail could not be clearly mentioned, and more, detailed treatment progression was not clearly shown [10, 11]. In this case, detailed observation and clear image using DBE were obtained, and an accurate diagnosis based on biopsy specimens was determined. Moreover, CR was accomplished by adjuvant chemotherapy and was maintained for 3 years.
In recent reports (NORDIC NEC Study), GEP-NECs represented a heterogeneous group of neoplasms, which could be better classified in different prognostic categories using both tumor morphology (well vs. poorly differentiated) and the Ki-67 index (< 55 or ≥ 55%). In this study, the authors demonstrated that patients with a Ki-67 > 55% had a higher response rate for platinum-based chemotherapy, but poorer survival rate than patients with a Ki-67 < 55%. Furthermore, the most important prognostic factor for survival was performance status (PS) [12]. In this case, poorly differentiated large and highly dysplastic tumor cells proliferated the alveolar structure, and the Ki-67 index was more than 90%. Therefore, the prognosis of this case could be considered as poor. In treating advanced extra-pulmonary NEC, guidelines recommend chemotherapy regimens [13,14,15], suitable for small cell lung carcinoma (SCLC). Therefore, platinum-containing regimens, such as etoposide (VP-16) plus cisplatin (VP), have been commonly used for NEC arising from the digestive system in clinical practice worldwide. This patient had no specific underlying diseases and kept a good PS. Therefore, adjuvant chemotherapy combining CDDP was continued, and subsequently lymph node metastasis was reduced and complete remission was obtained for 3 years.
To the best of our knowledge, this is the first case of small intestinal neuroendocrine carcinoma that was diagnosed using DBE, in which a long survival was accomplished by intensive therapy. The most important factor was an accurate and early diagnosis of NEC using DBE. In the future, this could enable minimal operations and prompt adjuvant chemotherapy.
References
Modlin IM, Oberg K, Chung DC, et al. Gastroenteropancreatic neuroendocrine tumors. Lancet Oncol. 2008;9(1):61–72.
Bosman FT, Carneiro F, Hruban RH, et al. WHO classification of tumours of the digestive system. 4th edition. Lyon: International Agency for Research on Cancer; 2010.
Bosman FT, Carneiro F, Hruban RH, et al. WHO classification of tumours of the digestive system. Geneva, Switzerland: World Health Organization; 2010.
Current trends of the incidence and pathological diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in Korea 2000–2009: multicenter study. Cancer Res Treat. 2012;44(3):157–165.
Zhang X, Ma L, Bao H, et al. Clinical, pathological and prognostic characteristics of gastroenteropancreatic neuroendocrine neoplasms in China: a retrospective study. BMC Endocr Disord. 2014;8(14):54. https://doi.org/10.1186/1472-6823-14-54.
Brierley JD, Gospodarowicz MK, Wittekind C, et al. UICC TNM classification of malignant tumours. Eight Edition. Wiley Blackwell. 2016; 201:99–101.
Mitsui K, Tanaka S, Yamamoto H, et al. Role of double-balloon endoscopy in the diagnosis of small-bowel tumors: the first Japanese multicenter study. Gastrointest Endosc. 2009;70(3):498–504.
Ito T, Igarashi H, Nakamura K, et al. Epidemiological trends of pancreatic and gastrointestinal neuroendocrine tumors in Japan: a nationwide survey analysis. J Gastroenterol. 2015;50:58–64.
Yamaguchi T, Machida N, Morizane C, et al. Multicenter retrospective analysis of systemic chemotherapy for advanced neuroendocrine carcinoma of the digestive system. Cancer Sci. 2014;105:1176–81.
Chen J, Zhang L, Zhang W, et al. A case of neuroendocrine malignant tumor with capsule retention diagnosed by double-balloon enteroscopy. Case Rep Gastroenterol. 2010;4(1):52–6.
Martini C, Sturniolo GC, De Carlo E, et al. Neuroendocrine tumor of small bowel. Gastrointest Endosc. 2004;60(3):431.
Sorbye H, Welin S, Langer SW, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24(1):152–60.
National Comprehensive Cancer Network National. Comprehensive Cancer Network (NCCN) guidelines. Available from URL: www.nccn.org (Ver. 1 2013).
Pavel M, Baudin E, Couvelard A, et al. ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2012;95:157–76.
Strosberg JR, Coppola D, Klimstra DS, et al. The NANETS consensus guidelines for the diagnosis and management of poorly differentiated (high-grade) extrapulmonary neuroendocrine carcinomas. Pancreas. 2010;39:799–800.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Seiji Kawano, Yuichi Miyashima, Yoshio Miyabe, Toshihiro Inokuchi and Hiroyuki Okada declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments..
Informed consent
Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Kawano, S., Miyashima, Y., Miyabe, Y. et al. A case of small intestinal neuroendocrine carcinoma diagnosed using double-balloon endoscopy with long-term survival. Clin J Gastroenterol 11, 240–244 (2018). https://doi.org/10.1007/s12328-018-0834-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-018-0834-8