Abstract
Introduction
Sclerosing mesenteritis includes a spectrum of inflammatory disorders involving the adipose tissue of the bowel mesentery.
Aim
To perform a systematic review of previously reported cases of sclerosing mesenteritis (SM) to determine the epidemiology, risk factors, methods of diagnosis, treatment patterns and outcomes for this disease.
Methods
Medline, PubMed, Google Scholar and Cochrane database were searched using keywords mesenteric panniculitis, retractile mesenteritis, mesenteric lipodystrophy and sclerosing mesenteritis. Data was collated into a single excel database, transferred into SPSS (Version 21.0) and analyzed.
Results
Patients diagnosed with SM were between ages of 3 and 88 with a mean age of 55 ± 19.2 years. SM was more common in Caucasians (n = 28, 60.8% of those reporting ethnicity) and men (n = 133, 69.3%) with a male to female ratio of 2.3:1. 28.6% (n = 55) of patients reported a prior abdominal surgery or abdominal trauma, 8.9% (n = 17) had a history of malignancy, and 5.7% (n = 11) of autoimmune disease. 85.4% (n = 164) underwent surgical abdominal exploration (open or laparoscopic); 41.7% (n = 80) had surgery with resection of the involved bowel and mesentery. 34.9% (n = 67) of patients received medical treatment with the majority of them receiving steroids (n = 56, 83.5%). Symptom duration of more than a month (66.7% vs 40.4%, p < 0.05), underlying autoimmune disorder (14.3% vs 4.0%, p < 0.05) or low protein (14.3% vs 4.0%, p < 0.05) at presentation were seen more frequently in those with poor treatment response whereas patients with tender abdomen (45.0% vs 19.0%, p < 0.05) or leukocytosis (20.5% vs 0.0%, p < 0.05) at presentation were likely to have good response to therapy. The most common complications included bowel obstruction/ileus/ischemia (n = 10, 23.8%) and obstructive uropathy/renal failure (n = 10, 23.8%). There were a total of 14 deaths, 12 (85.7%) of which were secondary to SM related complications.
Conclusion
SM is a poorly understood chronic inflammatory disease. Our study is the first systematic review of the published cases of SM. Future work is required to better understand this disease and its optimal therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sclerosing mesenteritis (SM) encompasses a spectrum of rare idiopathic diseases characterized by fibrotic and inflammatory changes in the adipose tissue of the bowel mesentery. The disease has had several names including retractile mesenteritis in 1924 [1], “mesenteric lipodystrophy” by Crane et al. in 1955 who characterized 5 cases with firm, thick plaque of the bowel mesentery [2] and finally in the 1960s, Ogden introduced the term mesenteric panniculitis [3]. With technological advancement and better disease recognition, Mindelzun et al. described computed tomography (CT) findings of SM as “misty mesentery” [4]. The umbrella term sclerosing mesenteritis (SM) can be used for all of these sub-divisions, but overlap of clinical and pathological features has resulted in many names based on the predominant feature or inflammatory pattern (Table 1) [5, 6]. In 1980, Cherayil et al. analyzed mesenteric fat tissue at autopsy of six patients with mesenteric panniculitis differentiating those samples by identifying abnormal lipid composition with increased cholesterol esters, free cholesterol and free fatty acids [7]. The pathological finding with a predominance of inflammation over fibrosis is classified as mesenteric panniculitis while predominance of fibrosis and retraction is commonly termed sclerosing mesenteritis or retractile mesenteritis. Fat necrosis suggests mesenteric lipodystrophy.
With advancements in CT scan quality and more frequent imaging studies, this rare condition is being encountered and reported more often; most cases are incidentally noted and less relevant to the original indication for the CT scan. Given the frequency with which this is now seen and with a shortage of large-scale studies, we performed a systematic review to pool the available data from previous studies to better understand the epidemiology, clinical presentation, modalities for diagnosis and treatment. Our knowledge of this condition is currently based on case reports, case-series and retrospective data analysis. One retrospective case series of 7620 CT scans estimated a prevalence of 0.6% while an assessment of autopsies estimated a prevalence of 1.0% [8].
Previous publications have shown a male predominance with Caucasian men being affected most frequently. SM seems to affect all age groups but the incidence increases with age, peaking in the 6th and 7th decade of life. Symptoms and signs previously reported were non-specific but included abdominal pain, fever, weight loss, anorexia and abdominal tenderness. SM is believed to periodically present clinically with an abdominal mass incorrectly raising concern for neoplasia. Many patients subsequently have surgical exploration as a result. SM seems to have a benign clinical course and chronic non-resolving symptoms or complications rarely occur.
Materials and methods
We performed an initial literature search of Medline, PubMed, Google Scholar and the Cochrane database using the keywords mesenteric panniculitis, retractile mesenteritis, mesenteric lipodystrophy and sclerosing mesenteritis. Inclusion criteria included any case report, letter to the editor, photo report or case series that was in English, available in electronic format that included a detailed summary on each patient’s clinical course. Manuscripts were excluded if an electronic version was unavailable, it was a review article with no new patients presented and if it was not written in English (Fig. 1). Following the literature search, all references were reviewed and from those that met inclusion criteria, data was extracted including demographic factors (e.g., age, gender, sex, ethnicity), medical comorbidities, prior surgeries, clinical features at presentation (e.g., acuity, symptoms, physical exam findings), workup (e.g., serologies and imaging), treatments (e.g., medical, surgical) and outcomes (e.g., complications, death). This systematic review was performed based on PRISMA guidelines [9].
430 publications were initially identified; 168 met our inclusion criteria accounting for 192 total cases of SM between 1960 and 2015. The bulk of publications (n = 99) were between 2006 and 2015. Most of the publications originated from the United States and Canada (37.5%), followed by Europe (28.1%), Asia (19.8%) and other locations (14.6%). Case reports were most frequently seen (n = 123, 73.2%), followed by quiz, clinical challenges and images (n = 20, 11.9%), letters to the editor (n = 14, 8.3%) and brief reports or brief communications (n = 11, 6.6%).
Definitions
Acute disease was defined as presentation with symptoms occurring for less than 30-days while chronic disease was defined by symptoms for more than 30-days. When considering serology, leukocytosis was defined by white blood cell (WBC) count greater than 11.0 × 109 per liter (L); Anemia was hemoglobin less than 11 g/dL; Low protein included total protein less than 6.3 g/dL and/or albumin level less than 3.5 g/dL. Abnormal liver tests referred to any elevation from normal levels of either aspartate aminotransferase (AST), alanine aminotransferase (ALT), or alkaline phosphatase (ALP).
Abdominal exploration included any laparotomy or laparoscopy of the abdominal cavity. Surgical resection or surgical excision included resection or excision of a mesenteric mass or portion of bowel, either complete or partial. Medical treatment referred to the use of steroids, antibiotics and/or other anti-inflammatory medications whereas conservative treatment was symptomatic management of the patients. Patients who had complete resolution of symptoms and imaging findings during the follow up treatment were identified as responders whereas those who did not have resolution were considered non-responders.
Statistics
Data from each study was extracted into a Microsoft excel database. Once the data extraction was complete, the data was transcribed into SPSS (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp) and analyzed. Continuous variables were reported as means with standard deviations or as medians, while categorical variables were reported as proportions. Fisher’s exact test was used to compare categorical variables while student’s t test was used to compare means. Sub-group column proportions were compared for categorical variables using z-test and Bonferroni correction was used to adjust for p values. All tests were two-sided and statistical significance was assumed at a p value of less than 0.05. Due to the short follow up period, mortality was reported as a proportion rather than performing a time to event analysis.
Results
The median age at diagnosis of SM was 61 years with a range of 3–88 years. Men were affected 2.3 times more frequently than women. In approximately three-fourth of the cases, information on ethnicity of the patient was not available (n = 146, 76.0%). Among the 46 patients where this information was provided, the majority (n = 28, 60.8%) were Caucasians (Table 2).
Past medical/surgical history
Past medical history was not reported in 59 (30.7%) patients and 41 (21.4%) did not have any significant past medical history. The most common medical co-morbidities included hypertension (n = 22, 11.5%), malignancy (n = 17, 8.9%), coronary artery disease (n = 14, 7.3%) and autoimmune disease (n = 11, 5.7%). Information on surgical history was not available for a majority (n = 103, 53.7%) of patients and a minority (n = 34, 17.7%) had no prior abdominal surgery or trauma. 55 (28.6%) patients had a prior history of abdominal surgery or abdominal trauma; of these, the most common previous abdominal surgeries included hysterectomy or Caesarean section (n = 13, 21.8%), appendectomy (n = 11, 20.0%), cholecystectomy (n = 10, 18.2%) and herniorrhaphy (n = 4, 7.3%).
Clinical features
In 44.2% (n = 85) of patients, the symptoms were classified as chronic while 35.4% (n = 68) presented acutely; 4.2% (n = 8) were classified as having an acute on chronic presentation and 1.6% (n = 3) were incidentally identified. The chronicity was not reported in the remaining 14.6% (n = 28). The most common presenting symptom was abdominal pain (n = 150, 78.1%), followed by fever (n = 50, 26.0%), weight loss (n = 44, 22.9%), diarrhea (n = 37, 19.3%), vomiting (n = 35, 18.2%), anorexia (n = 26, 13.5%), constipation (n = 21, 10.9%), bloating (n = 18, 9.4%), malaise (n = 11, 5.7%), nausea (n = 11, 5.7%), pain with eating (n = 9, 4.7%) and fatigue (n = 4, 2.1%). When examined, abdominal tenderness was noted in 38.0% (n = 73) of patients, an abdominal mass was present in 34.4% (n = 66) and 15.1% (n = 29) had a distended abdomen.
Laboratory parameters
C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) values were available for 52 and 43 patients, respectively. Of these, CRP was elevated in 86.5% (n = 45) and ESR was elevated in 88.4% (n = 38) of patients. Leukocytosis (n = 33, 17.2%), anemia (n = 31, 16.1%) and low protein levels (n = 9, 4.7%) were the other common laboratory abnormalities. Abnormal liver tests were noted in 6 (4.3%) patients. Among 13 patients in which IgG4 level was reported, 4 (30.7%) had an elevation.
Workup
Prior to making the diagnosis of SM, the most commonly suspected diagnosis was malignancy (n = 49, 25.5%). Despite a majority of patients undergoing CT scan (n = 148, 77.1%), the diagnosis was most commonly made via histopathology (n = 163, 84.9%), most frequently via open abdominal exploration (n = 132, 80.4%) and uncommonly laparoscopically (n = 26, 15.9%). Although a CT scan was performed in the majority of patients, only 15.1% (n = 29) were diagnosed based on imaging studies. The most common area of the bowel involved by SM was the small bowel mesentery/root of mesentery (n = 83, 43.2%), followed by the mesocolon (n = 33, 17.2%); however, the location was not specified in 39.6% (n = 76) of patients (Table 3). There were no statistically significant differences in the location of the mesentery and bowel involved when comparing different ethnicities.
Treatment, complications and follow up
Following diagnosis of SM, 41.7% (n = 80) were surgically resected, 34.9% (n = 67) underwent medical treatment and 17.2% (n = 33) were managed conservatively. 6.3% (n = 12) had no data on treatment. When medical treatment was chosen, steroids (prednisone or methylprednisolone) (n = 56, 83.5%) were most commonly used followed by colchicine (n = 8, 11.9%), tamoxifen (n = 8, 11.9%), 6-mercaptopurine (n = 8, 11.9%), antibiotics (n = 8, 11.9%), azathioprine (n = 7, 10.5%), methotrexate (n = 3, 4.5%), infliximab (n = 2, 2.9%) and the remainder (e.g., cyclophosphamide, IVIG, dipenicillamine and tacrolimus) were rarely used. Overlap between the various agents of medical treatment was not consistent and therefore unable to be assessed in our study.
20.8% (n = 40) developed complications with the most common being bowel obstruction/ileus/ischemia (n = 10, 23.8%), obstructive uropathy/renal failure (n = 10, 23.8%), steroid related complications (n = 6, 14.3%), sepsis/respiratory failure (n = 6, 14.3%) and venous thromboembolism (n = 4, 10.0%). Other complications which included pericardial effusion (n = 2, 5.0%) and pulmonary edema (n = 1, 2.5%) were seen less frequently.
78.6% (n = 151) of patients ultimately had complete resolution of symptoms and imaging findings during the follow up period (overall median: 10 months, overall mean: 17.6 ± 21.9 months) while 10.9% (n = 21) did not. No follow up was reported in the remaining 10.5% (n = 20) patients. There was no statistically significant difference in mean age, sex, presenting symptoms or treatment method between the responders and non-responders. However, the responders were more likely to have a tender abdomen (45.0% vs 19.0%, p < 0.05) or leukocytosis (20.5% vs 0.0%, p < 0.05) at presentation compared with non-responders. In contrast, the non-responders were more likely to have symptom duration of more than a month (66.7% vs 40.4%, p < 0.05), underlying autoimmune disorder (14.3% vs 4.0%, p < 0.05) or low protein (14.3% vs 4.0%, p < 0.05) at presentation (Table 4). Among all patients, 20.3% (n = 39) required more than one treatment and, of these, 20.5% (n = 8) required additional treatment in the form of surgical intervention. When additional medical therapy was given, steroids (n = 18, 46.1%), azathioprine (n = 8, 20.5%), colchicine (n = 5, 12.8%) and cyclophosphamide (n = 3, 7.7%) were the most frequently used medications.
The overall all-cause mortality rate associated with SM was 7.3% (n = 14) during the follow-up period. 85.7% (n = 12) of these deaths were due to the complications of SM including postoperative complications (n = 2), bowel ischemia (n = 2), sepsis and bronchopneumonia (n = 2), malnutrition and protein losing enteropathy (n = 2), venous thromboembolism (n = 1), renal failure (n = 1), cardiac arrest and pulmonary edema (n = 2). In the remaining 2 cases, the death was unrelated to SM.
Discussion
Our study reinforces some of the basic concepts that were believed to be associated with SM in the past. The largest series of patients published so far on this topic is by Akram et al. that included 92 cases. They performed both prospective and retrospective analysis of patients with sclerosing mesenteritis [8]. Our results are consistent with majority of their findings including demographic factors, laboratory results, imaging findings, histopathology, treatment and outcome. Our study additionally highlights certain baseline characteristics and laboratory parameters that can predict treatment response among these patients and the size of our study is more than double that of Akram et al. SM is commonly seen and sometimes confused for malignancy. This confusion can sometimes result in operative interventions that are unnecessary. Overall, patients with this disorder typically have a benign course although complications can occur. With more information about this disease, it is our hope that we will be able to isolate those at higher risk for the complications and appropriately treat them. This will require further research.
The etiology and mechanism of disease for SM remains unknown. There have been a wide range of conditions that are believed to be associated with SM including infectious, autoimmune, vasculitides, trauma, paraneoplasia and medications (Table 5). The presence of tubuloreticular structures in the pathologic specimens of the mesenteric mass is believed to support an autoimmune etiology [15–26]. We found that a small group of patients (5.7%) had a concurrent history of autoimmune disease with 30.4% of those who had IgG4 reported having an elevation. SM is thought to be associated with solid tumor malignancies (e.g., colorectal, lymphoma, urogenital) raising a suspicion of a paraneoplastic phenomenon, but in our study, this too was less frequently seen (8.9%) [28–34]. The theory of abnormal post-surgical healing and ischemia to the mesentery as a source of SM seemed more plausible in our cohort given that a large proportion of our patients had either gynecological surgery, a prior appendectomy or cholecystectomy [35–37]. The presenting symptoms of SM are non-specific and can include abdominal pain, fever, weight loss, diarrhea and vomiting. It is believed that these symptoms result from compressive effects of the abdominal mass on the bowel, vessels and lymphatics [8]. Physical examination findings are also non-specific consisting of an abdominal mass, tenderness and distension. The non-specific nature, without clinical diagnostic criteria, makes it sometimes challenging to diagnose SM, requiring an astute clinician to add this to their differential diagnosis. Since biopsy with pathological analysis remains the gold standard for confirming the diagnosis, this will continue to require invasive methods for confirmation of disease.
There are currently no specific serologic alterations that can differentiate SM from others. Given the inflammatory nature, elevations of acute phase reactants such as ESR, CRP and WBC are consistent with the pathologic process. Our results reinforced this. Anemia, hypoalbuminemia, and abnormal liver tests are also seen with SM and our data reaffirmed this as well. One limitation of our systematic review was a lack of uniform serologic reporting. Future work comparing patients with SM with those with malignancy and inflammatory diseases would be beneficial to differentiate the disorders and guide assessment and management.
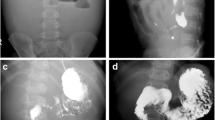
Ultrasonographic findings in SM are usually non-specific including a well-defined mass, non-deviated vessels within the mass and displaced bowel loops. These changes are similar to lipomatous tumors of the mesentery and commonly lead to further imaging with CT [42–46]. The most common finding seen on CT includes hyperattenuating fat (approximately −40 to −60 HU) with other less frequently seen non-specific findings, which include Fat-ring sign or Fatty halo, tumoral pseudocapsule and soft tissue nodules [47]. The “fatty ring” or “halo sign” (75–85% patients) is characterized by low-density normal fat surrounding the mesenteric mass of vessels and nodules [48, 49]. Tumoral pseudocapsule (50–59% patients) is characterized by a dense stripe (usually less than 3 mm) of soft tissue attenuation separating the normal fat surrounding a central inflamed mesenteric mass [47, 48]. Soft-tissue nodules (80% patients) are small nodules within the mesenteric mass that are usually less than 5 mm in diameter [47–49]. The characteristics of SM on MRI are contingent on the subset of disease. In mesenteric panniculitis, findings include an ill-defined T2 hyperintense signal in the mesenteric fat likely representing edema and prominent lymph nodes [50, 51]. In retractile mesenteritis, a T2 hypointense signal might be seen at the site of a localized mass of fibrous tissue also with delayed hyperenhancement of fibrous tissue [52, 53]. In fluorodeoxyglucose positron emission tomography (FDG-PET) scan, the most common finding is focal hypermetabolism in the mesenteric lesions of mesenteric panniculitis [54, 55]. Our study supports that none of the imaging methods, ultrasound, CT, MRI or FDG-PET changes the disease trajectory altering the progression to surgical exploration. Further research is needed to identify more pathognomonic or hallmark findings consistent with SM to allow imaging to easily diagnose SM compared with the more invasive histopathology that is currently required.
Based upon gross pathologic findings, Kipfer et al. originally classified mesenteric panniculitis involving the small bowel mesentery into three types. “Type I” (42%) is the most common type with diffuse thickening of the mesentery, “Type II” (32%) has an isolated nodular mass at the mesenteric root and “Type III” (26%) contains multiple discrete mesenteric nodules [56]. Cherayil et al. characterized 3 histological stages of disease: (1) Chronic nonspecific inflammation (2) fat necrosis and (3) fibrosis [7]. Chronic non-specific inflammation characterizes the initial stage with mesenteric lipodystrophy and mesenteric fat being replaced by a layer of foamy macrophages. Fat necrosis can sometimes be termed mesenteric panniculitis, which is histologically identified by infiltration with plasma cells, foreign body giant cells, polymorphonuclear cells and foamy macrophages. Fibrosis associated with SM is also called retractile mesenteritis revealing collagen deposition, fibrosis and inflammation with scarring. The primary histologic criterion for SM is infiltration of the mesentery by foamy lipid-laden macrophages with clusters of lymphocytes and potential fibrosis [7, 20].
Histopathology remains the gold standard but it requires invasive testing and generating an appropriate differential diagnosis for SM is essential. Many conditions can mimic this disease. The broad differential diagnosis includes malignancy [non hodgkin’s lymphoma, lymphosarcoma, peritoneal carcinomatosis, carcinoid, desmoid tumor, lipoma, mesothelioma, metastasis (colon carcinoma, pancreatic carcinoma, ovarian carcinoma), adipose neoplasm (liposarcoma, myelolipoma, angiomyolipoma)], epiploic appendagitis, retroperitoneal fibrosis and other causes of mesenteric edema and inflammation (pancreatitis, appendicitis, cholecystitis, diverticulitis and inflammatory bowel disease). Our study cohort covered many decades, but the general tendency for surgical evaluation seemed consistent as this is the best way to rule out other sinister diseases that remain on the differential diagnosis.
There is no consensus for optimal treatment of SM and until there are better less invasive criteria for diagnosis, clinical trials considering its treatment will be limited to surgical interventions. Asymptomatic patients probably do not require any intervention. Various medications have been used to target symptomatic relief and/or reduce mesenteric inflammation including steroids [57], tamoxifen [58], colchicine [59], progesterone [60], pentoxifyline [61], thalidomide [41], azathioprine [62], antibiotics [57], infliximab [63], cyclophosphamide [64], among others. Surgery has a limited role and aides in selected cases in relieving obstruction and obtaining a pathologic specimen for diagnosis. Complete removal of the mass is usually not possible due to diffuse involvement of the bowel and mesentery along with vasculature. Akram et al. outlined a treatment algorithm for SM. The algorithm suggests no treatment for asymptomatic patients; For those who are symptomatic with bowel obstruction refractory to conservative therapy, surgery was the initial treatment of choice. If symptoms persist or if there was non-obstructive pathology, they recommended tamoxifen twice daily with a prednisone taper over 3 months. For those patients with non-obstructive pathology, they advised tamoxifen twice daily with a prednisone taper over 3 months. If patients responded, they recommended continuing the tamoxifen indefinitely. If tamoxifen is contraindicated, not tolerated or if there is lack of response, they advised considering colchicine, azathioprine or thalidomide [8].
SM tends to have a self-limiting course. However, a small percentage can experience prolonged debilitation, and in the most severe cases, death [8]. In our analysis, the majority (80%) had a slow disease progression with favorable outcome; however, 11% resulted in significant morbidity with a 7.3% associated all-cause mortality rate.
Our study has several limitations. These include those of a systematic review. The cases were reported from various sources and the publications lacked uniformity in the information reported. Therefore, we were only able to extract the information that was formally published and despite our pooling of 192 cases, the data set was incomplete in many categories that we tallied. In addition, we only included manuscripts published in English which can result in a selection bias. In lieu of these limitations, we believe our systematic review is the largest of its kind for this disease and provides the best and most up to date information for this disease state.
Conclusion
Sclerosing mesenteritis is a benign chronic inflammatory condition often confused with neoplastic process. With fear of missing the diagnosis of malignancy, patients often undergo invasive procedures such as exploratory laparotomy. With the advent of enhanced imaging techniques, this diagnosis can be inferred without exposing patients to surgical procedures with their associated postoperative complications but further research is needed to better codify criteria for radiologic diagnosis. Abdominal tenderness and leukocytosis are more frequently seen in those who respond to treatment of SM. There is a lot of information about this disease that needs clarification, and larger well-controlled analyses can better define the presentation, ways to differentiate this from other diseases serologically and via imaging, the optimal imaging techniques and the best treatment algorithm.
References
Jura V. Sulla mesenterite retratile e sclerosante. Policlinico (Sez. Chir.) 1924;31:575.
Crane JT, Aguilar MJ, Grimes OF. Isolated lipodystrophy, a form of mesenteric tumor. Am J Surg. 1955;90(2):169–79.
Ogden WW 2nd, Bradburn DM, Rives JD. Panniculitis of the mesentery. Ann Surg. 1960;151:659.
Mindelzun RE, Jeffrey RB Jr, Lane MJ, et al. The misty mesentery on CT: differential diagnosis. AJR Am J Roentgenol. 1996;167:61.
Emory TS, Monihan JM, Carr NJ, et al. Sclerosing mesenteritis, mesenteric panniculitis and mesenteric lipodystrophy: a single entity? Am J Surg Pathol. 1997;21:392.
Kelly JK, Hwang WS. Idiopathic retractile (sclerosing) mesenteritis and its differential diagnosis. Am J Surg Pathol. 1989;13:513.
Cherayil GD, Scaria KS, Hensley GT, et al. Abnormal lipid composition of fat tissue in human mesenteric panniculitis. Lipids. 1981;16(3):199–202.
Akram S, Pardi DS, Schaffner JA, et al. Sclerosing mesenteritis: clinical features, treatment, and outcome in ninety-two patients. Clin Gastroenterol Hepatol. 2007;5(5):589–96.
Prisma statement. http://www.prisma-statement.org/. Accessed 10 Aug 2016.
Roginsky G, Mazulis A, Ecanow JS, et al. Mesenteric panniculitis associated with vibrio cholerae infection. ACG Case Rep J. 2015;3(1):39–41.
Ege G, Akman H, Cakiroglu G. Mesenteric panniculitis associated with abdominal tuberculous lymphadenitis: a case report and review of the literature. Br J Radiol. 2002;75(892):378–80.
Alonso Socas MM, Valls RA, Gómez Sirvent JL, et al. Mesenteric panniculitis by cryptococcal infection in an HIV-infected man without severe immunosuppression. AIDS. 2006;20(7):1089–90.
Wang S, McKay GD, Vonthethoff L, et al. Latent schistosomiasis triggering mesenteric panniculitis. ANZ J Surg. 2013;83(5):396–7.
Venkataramani A, Behling CA, Lyche KD. Sclerosing mesenteritis: an unusual cause of abdominal pain in an HIV-positive patient. Am J Gastroenterol. 1997;92:1059.
Nomura Y, Naito Y, Eriguchi N, et al. A case of IgG4-related sclerosing mesenteritis. Pathol Res Pract. 2011;207(8):518–21.
Salvarani C, Valli R, Boiardi L, et al. IgG4-associated sclerosing mesenteritis. Clin Exp Rheumatol. 2011;29(1 Suppl 64):S79–80 (PMID: 21586200).
Belghiti H, Cazals-Hatem D, Couvelard A, et al. Sclerosing mesenteritis: can it be a IgG4 dysimmune disease?. Ann Pathol. 2009;29(6):468–74.
Chen TS, Montgomery EA. Are tumefactive lesions classified as sclerosing mesenteritis a subset of IgG4-related sclerosing disorders? J Clin Pathol. 2008;61(10):1093–7.
Kim EJ, Kim EY, Song JE, et al. A case of IgG4-related sclerosing mesenteritis associated with Crohn’s disease]. Korean J Gastroenterol. 2014;63(3):176–82.
Minato H, Shimizu J, Arano Y, et al. IgG4-related sclerosing mesenteritis: a rare mesenteric disease of unknown etiology. Pathol Int. 2012;62(4):281–6.
Dor AM, Kohler JL, Aubrespy P, et al. Pseudo-tumorous panniculitis of the mesentery. An unusual initial stage of acute lupus erythematosus in a 10-year-old girl. Sem Hop. 1982;58(48):2847–50.
Makdsi F, Brit M. A case of sclerosing mesenteritis with rheumatoid arthritis. South Med J. 2010;103(1):96–7.
Garrido A, Verdejo C, Márquez JL, et al. Intestinal lymphoma and mesenteric panniculitis: complications of undiagnosed celiac disease. Gastroenterol Hepatol. 2008;31(4):221–4.
Ruiz P, Suarez M, Nishida S, et al. Sclerosing mesenteritis in small bowel transplantation: possible manifestation of acute vascular rejection. Transplant Proc. 2003;35(8):3057–60.
Watanabe I, Taneichi K, Baba Y, Sakai I, et al. A case of mixed connective tissue disease with mesenteric panniculitis. Nihon Naika Gakkai Zasshi. 1989;78(1):93–4.
Papadaki HA, Kouroumalis EA, Stefanaki K, et al. Retractile mesenteritis presenting as fever of unknown origin and autoimmune haemolytic anaemia. Digestion. 2000;61:145.
Martín-Suñé N, Ríos-Blanco JJ, Díaz-Menéndez M, et al. Mesenteric panniculitis as a first manifestation of Schönlein-Henoch disease. J Postgrad Med. 2010;56(4):303–4.
Wilkes A, Griffin N, Dixon L, et al. Mesenteric panniculitis: a paraneoplastic phenomenon? Dis Colon Rectum. 2012;55(7):806–9.
Gögebakan Ö, Albrecht T, Osterhoff MA, et al. Is mesenteric panniculitis truely a paraneoplastic phenomenon? A matched pair analysis. Eur J Radiol. 2013;82(11):1853–9.
Mella Laborde M, Ivorra Muñoz F, García García S, et al. Mesenteric panniculitis as the initial manifestation of a B cell lymphoma. Acta Gastroenterol Latinoam. 2015;45(2):137–9.
Lester L, Ewalt M, Warnke R, et al. Systemic panniculitis-like T-cell lymphoma with involvement of mesenteric fat and subcutis. J Cutan Pathol. 2015;42(1):46–9.
Güerri Fernández R, Villar García J, García Sirvent L, et al. Mesenteric panniculitis, first clinical manifestation of a disseminated B cell lymphoma. Rev Clin Esp. 2008;208(2):109–10.
Goh J, Otridge B, Brady H, et al. Aggressive multiple myeloma presenting as mesenteric panniculitis. Am J Gastroenterol. 2001;96(1):238–41.
Harris RJ, van Stolk RU, Church JM, et al. Thoracic mesothelioma associated with abdominal mesenteric panniculitis. Am J Gastroenterol. 1994;89:2240.
Lee KJ, Ehrenpreis ED, Greenberg J, et al. Mesenteric panniculitis following colonoscopy, polypectomy, and epinephrine injection. Endoscopy. 2010;42(Suppl 2):E44–5.
Canyigit M, Kara T. Mesenteric panniculitis: abdominal trauma or surgery as a causative factor. Rev Esp Enferm Dig. 2009;101(12):888 (author reply 888–9).
Michael P, Gratiot J. Mesenteric Panniculitis Associated With Trauma. Calif Med. 1964;100:285–7.
Van der Hulst RW, Rauws EA, Tytgat GN. Mesenteritis secondary to the use of a pneumatic jackhammer. Eur J Gastroenterol Hepatol. 1995;7(6):573.
Rozin A, Bishara B, Ben-Izhak O, et al. Fibrosing omental panniculitis and polyserositis associated with long-term treatment by paroxetine. Isr Med Assoc J. 2000;2(9):714–6.
Bharucha KJ, Blevins SM. Sclerosing mesenteritis: an ergot-related complication of pergolide therapy in Parkinson’s disease? Mov Disord. 2008;23(6):922–3.
Ginsburg PM, Ehrenpreis ED. A pilot study of thalidomide for patients with symptomatic mesenteric panniculitis. Aliment Pharmacol Ther. 2002;16(12):2115–22.
Rosón N, Garriga V, Cuadrado M, et al. Sonographic findings of mesenteric panniculitis: correlation with CT and literature review. J Clin Ultrasound. 2006;34(4):169–76.
Catalano O, Cusati B. Sonographic detection of mesenteric panniculitis: case report and literature review. J Clin Ultrasound. 1997;25(3):141–4.
Otero E, Pajaró A, Pardo P, et al. Mesenteritic panniculitis: detection by abdominal ultrasonography. Rev Esp Enferm Dig. 2003;95(5):338–42, 333–7.
Sato M, Ishida H, Konno K, et al. Mesenteric panniculitis: sonographic findings. Abdom Imaging. 2000;25(2):142–5.
van den Heuvel AG, Op den Orth JO. Nodular form of intra-abdominal panniculitis: sonographic features. Eur J Radiol. 1990;10(3):175–6.
van Breda Vriesman AC, Schuttevaer HM, Coerkamp EG, et al. Mesenteric panniculitis: US and CT features. Eur Radiol. 2004;14(12):2242–8.
Daskalogiannaki M, Voloudaki A, Prassopoulos P, et al. CT evaluation of mesenteric panniculitis: prevalence and associated diseases. AJR Am J Roentgenol. 2000;174(2):427–31.
Coulier B. Mesenteric panniculitis. Part 1: MDCT–pictorial review. JBR-BTR. 2011;94(5):229–40.
Fujiyoshi F, Ichinari N, Kajiya Y, et al. Retractile mesenteritis: small-bowel radiography, CT, and MR imaging. AJR Am J Roentgenol. 1997;169(3):791–3.
Kobayashi S, Takeda K, Tanaka N, et al. Mesenteric panniculitis: MR findings. J Comput Assist Tomogr. 1993;17(3):500–2.
Kronthal AJ, Kang YS, Fishman EK, et al. MR imaging in sclerosing mesenteritis. AJR Am J Roentgenol. 1991;156(3):517–9.
Ghanem N, Pache G, Bley T. MR findings in a rare case of sclerosing mesenteritis of the mesocolon. J Magn Reson Imaging. 2005;21(5):632–6.
Albano D, Bosio G, Bertagna F. Mesenteric panniculitis demonstrated on 18F-FDG PET/CT. Clin Nucl Med. 2016;41(3):e164–6.
Nguyen BD. F-18 FDG PET demonstration of sclerosing mesenteritis. Clin Nucl Med. 2003;28(8):670–1.
Kipfer RE, Moertel CG, Dahlin DC. Mesenteric lipodystrophy. Ann Intern Med. 1974;80:582.
Issa I, Baydoun H. Mesenteric panniculitis: various presentations and treatment regimens. World J Gastroenterol. 2009;15(30):3827–30.
Guest S. Tamoxifen therapy for encapsulating peritoneal sclerosis: mechanism of action and update on clinical experiences. Perit Dial Int. 2009;29(3):252–5.
Iwanicki-Caron I, Savoye G, Legros JR, et al. Successful management of symptoms of steroid-dependent mesenteric panniculitis with colchicine. Dig Dis Sci. 2006;51:1245.
Mazure R, Fernandez Marty P, Niveloni S, et al. Successful treatment of retractile mesenteritis with oral progesterone. Gastroenterology. 1998;114:1313.
Kapsoritakis AN, Rizos CD, Delikoukos S, et al. Retractile mesenteritis presenting with malabsorption syndrome. Successful treatment with oral pentoxifylline. J Gastrointestin Liver Dis. 2008;17(1):91–4.
Bala A, Codere SP, Johnson DR, et al. Treatment of sclerosing mesenteritis with corticosteroids and azathioprine. Can J Gastrenterol. 2001;15(8):533–5.
Miranda-Bautista J, Fernández-Simón A, Pérez-Sánchez I, et al. Weber-Christian disease with ileocolonic involvement successfully treated with infliximab. World J Gastroenterol. 2015;21(17):5417–20.
Colomer Rubio E, Blanes Gallego A, Carbonell Biot C, et al. Mesenteric panniculitis with retroperitoneal involvement resolved after treatment with intravenous cyclophosphamide pulses. An Med Interna. 2003; 20(1):31–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding:
This research received no specific grant or funds from any agency in the public, commercial or not-for-profit sectors.
Conflict of interest:
Prabin Sharma, Siddhartha Yadav and Christine Marie Needham have no affiliations with or involvement in any organization or entity with financial or non-financial interest in the subject matter or materials discussed in this manuscript. Paul Feuerstadt is on the speakers bureau and has consulted for Merck and Co., Enterahealth and Allergan.
Human Rights:
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent:
This study does not involve human subjects and does not apply to giving Informed Consent,
Rights and permissions
About this article
Cite this article
Sharma, P., Yadav, S., Needham, C.M. et al. Sclerosing mesenteritis: a systematic review of 192 cases. Clin J Gastroenterol 10, 103–111 (2017). https://doi.org/10.1007/s12328-017-0716-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-017-0716-5