Abstract
Hemosuccus pancreaticus is a gastrointestinal hemorrhage through the main pancreatic duct. Here, we report a rare case of hemosuccus pancreaticus due to a mucinous cystic neoplasm of the pancreas. A 62-year-old woman who had been followed for a branch duct intraductal papillary mucinous neoplasm visited our emergency room due to severe abdominal pain and bloody discharge. Computed tomography revealed that the pancreatic cyst increased the tension of the wall and a high-density area indicative of bleeding into the cyst was observed. Endoscopy showed opening of and hemorrhaging from the papilla of Vater. The patient was diagnosed with hemosuccus pancreaticus caused by hemorrhaging into the cyst from the branch duct intraductal papillary mucinous neoplasm. Based on this diagnosis, elective distal pancreatectomy was performed. The histopathological diagnosis was a mucinous cystic neoplasm with intermediate-grade dysplasia based upon the pathological findings that fibrous ovarian-type stroma existed abundantly and the stroma cells were positive for progesterone receptor and inhibin. Hemosuccus pancreaticus caused by a mucinous cystic neoplasm is extremely rare and there has been only one case reported to date. In conclusion, it should be recognized that pancreatic cystic neoplasms including mucinous cystic neoplasms may cause hemosuccus pancreaticus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemosuccus pancreaticus (HP) is defined as a gastrointestinal hemorrhage through the main pancreatic duct and is a rare cause of gastrointestinal bleeding [1]. HP is mostly caused by hemorrhage into the cyst due to the rupture of the pseudoaneurysm followed by acute or chronic pancreatitis. It has been reported that pancreatic tumors or procedures associated with endoscopic ultrasound-guided fine-needle aspiration induce HP [2, 3]. However, HP complicated by pancreatic tumors, especially pancreatic cystic neoplasms, is very rare. Here, we report a case of HP due to a mucinous cystic neoplasm (MCN) of the pancreas.
Case report
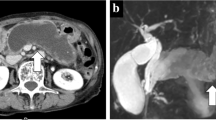
A 62-year-old woman with a pancreatic tail cyst, which was found during a medical checkup 3 years earlier, was referred to our hospital for further examination. Abdominal computed tomography (CT) demonstrated a 4-cm oval-shaped cyst in the tail of the pancreas, and magnetic resonance imaging (MRI) revealed septum and no mural nodules in the cyst (Fig. 1a,1b). Accordingly, she was diagnosed with a branch duct intraductal papillary mucinous neoplasm (BD-IPMN) and followed up regularly by imaging studies.
a, b Abdominal computed tomography (CT) (upper left) and magnetic resonance imaging (MRI) (upper right) performed 3 years before the the most recent admission. CT demonstrated a 4-cm oval-shaped cyst in the tail of the pancreas (arrow). MRI revealed septum (arrow head) and no mural nodules in the cyst. c, d Contrast-enhanced abdominal CT (bottom left) and MRI (bottom right) performed 4 months before the most recent admission. CT showed reduction in the size of the pancreatic cyst and septal thickening (arrow). MRI revealed a high-intensity site representing the pancreatic cyst in a T1-emphasized image (arrow head)
The patient had suffered intermittent abdominal pain for the past 4 months and laboratory examination revealed anemia. Therefore, an esophagogastroduodenoscopy (EGD), colonoscopy, capsule endoscopy of the intestine, abdominal CT, and MRI were performed. Although the endoscopy revealed gastrointestinal bleeding, the site of the bleeding in the gastrointestinal tract was not determined. Contrast-enhanced abdominal CT showed a reduction in the size of the pancreatic cyst and thickening of the septum. Abdominal MRI showed the pancreatic cyst as a high-intensity area in T1-emphasized imaging (Fig. 1c, d). Therefore, we considered that the gastrointestinal bleeding and anemia were caused by bleeding from the BD-IPMN, and surgical therapy was subsequently planned.
However, prior to the operation, the patient visited our emergency room because of severe abdominal pain and bloody discharge and was admitted to our hospital. At that time, the patient’s blood pressure was 82/41 mmHg and her palpebral conjunctiva was pale. The abdomen was flat, soft, no tenderness and showed no overt signs of a tumor. In a laboratory examination performed on admission, the hemoglobin level was low (8.9 g/dL), but liver and renal function, pancreatic enzyme levels, coagulation test results, and tumor markers were within the normal range (Table 1). The patient received a red blood cell transfusion because of anemia and low blood pressure. Abdominal pain subsided in response to pentazocine hydrochloride. Emergent abdominal CT revealed that the size of the pancreatic cyst had increased slightly and that the wall exhibited tension, and a high-density area suspected to represent bleeding into the cyst was observed (Fig. 2a). An EGD showed opening of and hemorrhaging from the papilla of Vater. Consequently, the patient was diagnosed with HP due to hemorrhage into a cyst from the BD-IPMN. She underwent an elective distal pancreatectomy and D2 lymph node dissection 9 days after admission (Fig. 2b). A macroscopic examination of a freshly resected specimen showed that bloody liquid had accumulated in the cyst which was covered by a capsule. Following formaldehyde fixation of the resected specimen, septum and mural nodules were confirmed in the cyst (Fig. 3a, b). Histopathological examinations revealed that the epithelium was hyperplastic at the site of mural nodules. The epithelial cells exhibited severe atypia with nuclear stratification. There were also mucus-producing goblet cells present. In another resected specimen, the epithelium was peeled off and ovarian-type stroma exposed. In the cyst there was blood due to rupture of rich blood capillaries in ovarian-type stroma. In this section, collagenous fiber covered the lumen of the cyst and it was presumed that the epithelium of this section had fallen off previously. No communication between the cystic tumor and the pancreatic duct on the resected specimen was detected histopathologically. Moreover, fibrous ovarian-type stroma existed abundantly, and immunohistochemistry revealed that the stroma cells were positive for progesterone receptor and inhibin. Thus, the pancreatic cystic lesion was ultimately diagnosed as an MCN with intermediate-grade dysplasia (Fig. 4). The patient’s postoperative course was uneventful and she is now asymptomatic.
a Emergent abdominal CT (left) revealed that the pancreatic cyst (arrow) showed no change in size, but there was an increase in tension of the wall and a high-density area (arrow head) suspected to represent bleeding into the cyst was observed on admission. b Upper gastrointestinal endoscopy showed opening of and hemorrhaging from the papilla of Vater (arrow)
a A loupe image of the site of mural nodules. The epithelium was hyperplastic. b Magnified view of the region in the left square of the microscopic image in Fig. 4a. The epithelial cells showed severe atypia with stratification and localization of nuclei. Mucus-producing goblet cells were also observed. c Magnified view of the region in the right square of the microscopic image in Fig. 4a. Fibrous ovarian-type stroma were abundant. d, e Immunohistochemical analyses revealed that the stroma cells were positive for progesterone receptor (d) and inhibin (e)
Discussion
To our knowledge, HP caused by MCN is extremely rare, and there has been only one case reported in the literature. Shinzeki et al. reported a case of a 71-year-old woman who presented with HP due to carcinoma in mucinous cystadenoma with ovarian-type stroma [4]. Our case resembles the previous case with respect to sex, age, anemia, detection by EGD, pancreatic cystic lesion of the tail, and operative technique. On the other hand, our case differs from the previous report as no malignant lesion was detected histopathologically in our case. This rare case reported by Shinzeki et al. also raised the possibility that the existence of malignancy could induce HP in patients with MCN; however, the authors mentioned that the cancer cells in mucinous cystadenoma did not infiltrate into the parenchyma or the duct of the pancreas. Therefore, it is assumed that the existence of malignancy would not be associated with the onset of HP.
Although communication between the pancreatic duct and the MCN was not detected histologically in the report by Shinzeki et al., it was demonstrated by direct pancreatography in a resected specimen. Therefore, the authors concluded that tumor hemorrhaging via communication between tumor cysts and the pancreatic duct may lead to HP. On the other hand, communication between the pancreatic duct and the MCN was not seen histologically in our case. However, it has been reported that communication between MCNs and pancreatic ducts is rarely observed [5]. In this context, it is plausible that the MCN might have communicated with the pancreatic duct in our case. Based on postoperative histopathological findings, hemorrhaging into the MCN cyst in our case was thought to result from exposure of ovarian-type stroma, which had many vessels. Moreover, HP continued intermittently because of repeated exposure of ovarian-type stroma in other parts of the MCN, which could have accounted for the patient's persistent anemia during the preceding 4 months.
Here, we describe a case of HP due to an MCN, which is a type of pancreatic cystic neoplasm. The incidence of pancreatic cystic neoplasms is increasing due to aging of the population and better detection as a result of improved diagnostic technology [6, 7]. We performed a literature search to identify cases of HP caused by pancreatic cystic neoplasms, excluding iatrogenic cases, and identified 5 case reports—1 case with IPMN [8], 3 cases with serous cystic neoplasm (SCN) [9–11], and 1case with MCN [4] (Table 2). Based upon these reports, and including our case, the site of the cystic lesion is almost always in the pancreatic tail and the size ranges from 2.5–12 cm. Most cases are associated with anemia, some of them resulting from shock and in some cases needing red blood cell transfusion. HP was detected by endoscopic examination in all cases. All cases underwent a pancreatectomy as treatment and are currently alive. Only 1 case showed a malignant lesion in the pancreatic cystic neoplasm histopathologically. Regarding the cause of hemorrhage, the bleeding originated from the tumors themselves in 4 cases and was caused by rupture of a splenic artery aneurysm in 1 case. However, when HP due to pancreatic cystic neoplasms is properly diagnosed and surgically treated, the prognosis seems to be relatively good.
In conclusion, we report a rare case of HP caused by MCN of pancreas. It should be recognized that pancreatic cystic neoplasms including MCN may cause HP.
References
Sandblom P. Gastrointestinal hemorrhage through the pancreatic duct. Ann Surg. 1970;171:61–6.
Keswani RN. Hemosuccus pancreaticus after endoscopic ultrasound-guided fine needle aspiration of a pancreatic cyst. Endoscopy. 2010;42:E79.
Kurland J, Matthews T, Hoff E, et al. Hemosuccus pancreaticus caused by metastatic renal cell carcinoma. Gastrointest Endosc. 2007;66:1241–2.
Shinzeki M, Hori Y, Fujino Y, et al. Mucinous cystic neoplasm of the pancreas presenting with hemosuccus pancreaticus: report of a case. Surg Today. 2010;40:470–3.
Le Borgne J, de Calan L, Partensky C. Cystadenomas and cystadenocarcinomas of the pancreas: a multiinstitutional retrospective study of 398 cases. French Surgical Association. Ann Surg. 1999;230:152–61.
Laffan TA, Horton KM, Klein AP, et al. Prevalence of unsuspected pancreatic cysts on MDCT. Am J Roentgenol. 2008;191:802–7.
de Jong K, Nio CY, Hermans JJ, et al. High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol. 2010;8:806–11.
Inoue H, Katsurahara M, Takei Y. Intraductal papillary mucinous neoplasm presenting as hemosuccus pancreaticus. Clin Gastroenterol Hepatol. 2015;13:e57–8.
Pinarbasi B, Poturoglu S, Yanar H, et al. A rare cause of hemosuccus pancreaticus: primary splenic artery aneurysm ruptured into pancreatic serous cystadenoma. Turk J Gastroenterol. 2008;19:57–63.
Kanno A, Satoh K, Hamada S, et al. Serous cystic neoplasms of the whole pancreas in a patient with von Hippel-Lindau Disease. Intern Med. 2011;50:1293–8.
Shan YS, Sy ED, Tsai HM, et al. Chronic hemosuccus pancreaticus: a rare complication of pancreatic microcystic adenoma successfully treated with Whipple’s procedure. Pancreas. 2000;20:416–8.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest:
All authors declare that they have no conflict of interest.
Human Rights:
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent:
Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Matsumoto, Y., Miyamoto, H., Fukuya, A. et al. Hemosuccus pancreaticus caused by a mucinous cystic neoplasm of the pancreas. Clin J Gastroenterol 10, 185–190 (2017). https://doi.org/10.1007/s12328-016-0711-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-016-0711-2