Abstract
Diabetic kidney disease (DKD) is one of the most important diabetic complications. DKD is also the most common cause of chronic kidney disease (CKD) and end-stage renal disease. This review focused on potential therapeutic drugs for which there is established evidence of treatment for DKD. The earliest evidence for DKD treatment was established with renin–angiotensin system (RAS) inhibitors; however, their efficacy was partial. Recently, the sodium-glucose co-transporter 2 (SGLT2) inhibitors, including empagliflozin (EMPA-REG Outcome), canagliflozin (CREDENCE trial), and dapagliflozin (DAPA-CKD), demonstrated a significant and clinically relevant reduction in the risks of albuminuria and progression of nephropathy, doubling of serum creatinine levels, and initiation of renal replacement therapy. Additionally, incretin-based therapeutic agents, such as glucagon-like peptide 1, liraglutide (LEADER), and dipeptidyl peptidase 4 inhibitors, linagliptin (CARMERINA) have elicited vasotropic actions, suggesting a potential for reducing the risk of DKD. Until recently, mineralocorticoid receptor antagonists (MRAs) have not been suitable for DKD treatment because of their adverse effect of hyperkalemia. In contrast, finerenone, a non-steroidal MRA, significantly reduced renal composite endpoint without severe hyperkalemia that would force its discontinuation (FIDELIO-DKD). Thus, the mainstay treatments of DKD are RAS inhibitors, SGLT2 inhibitors, incretin-based therapeutic agents, and non-steroidal MRA, or in other words, the DKD “fantastic four”.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The incidence of diabetes is rapidly increasing in the population; therefore, therapeutic agents that meet the medical needs of its complications (such as diabetic kidney disease) must be identified. |
The combination of ACEIs and ARBs did not improve outcomes and was linked to an increased risk of serious adverse events; thus, it is not recommended in DKD. |
SGLT2 inhibitors have a protective effect on renal outcomes in DKD, including decreased albuminuria, increased serum creatinine levels, and induced renal replacement therapy. |
Beyond their effects on glycemic control, incretin-based therapeutic agents have potent pleiotropic effects in patients with DKD. |
Non-steroidal mineralocorticoid receptor antagonists (MRAs) have been developed to selectively increase benefits and decrease adverse effects via changes in receptor affinity and tissue tropism. |
Introduction
The number of patients with diabetes worldwide is rapidly increasing. Additionally, type 2 diabetes is reported as the seventh leading cause of mortality in the USA (http://www.cdc.gov). According to the recent report published by International Diabetes Foundation, the number of patients with diabetes worldwide is approximately 380 million, and the total number of patients will reach 590 million by 2035. Moreover, most new patients with diabetes will emerge from Southeast Asia and West Pacific regions (http://www.idf.org/). Two large clinical trials, the Diabetes Control and Complications Trial in type 1 diabetes and the United Kingdom Prospective Diabetes Study in type 2 diabetes, clearly indicated that intensive glycemic control slows the progression of diabetic complications, including diabetic kidney disease (DKD). These clinical studies suggest that hyperglycemia is a major factor in developing DKD [1, 2]. In addition to hyperglycemia, activation of the renin–angiotensin system (RAS) plays a significant role in the pathogenesis of DKD [3,4,5].
Many studies have reported that the blockade of RAS using angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin I receptor blockers (ARBs) slows the progression of DKD [6,7,8,9,10]. However, recent studies suggest that ACEIs and ARBs could not stop the progression of DKD.
The Empagliflozin and Progression of Kidney Disease in type 2 diabetes (EMPA-REG Renal outcome) trial, the Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trial, and the Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) trial revealed that sodium-glucose co-transporter 2 (SGLT2) inhibitors have a protective effect on renal outcomes in DKD, including decreased albuminuria, doubled serum creatinine levels, and induction of renal replacement therapy [11,12,13].
Several studies have reported that glucagon-like peptide 1 (GLP-1) receptor agonists and dipeptidyl peptidase 4 (DPP4) inhibitors exhibit potent pleiotropic effects against DKD beyond their effects on glycemic control. The pre-specified secondary analysis of the Liraglutide Effect and Action in Diabetes: Evaluation of cardiovascular outcome Results (LEADER) trial revealed that the rates of the development and progression of DKD were lower in the liraglutide-treated group than in the placebo group [14]. Furthermore, the Cardiovascular and Renal Microvascular Outcome Study With Linagliptin (CARMELINA) trial indicated that linagliptin, a DPP4 inhibitor, decreased the risk of progression of microvascular diseases, including albuminuria, in patients with DKD [15].
Recently, third-generation mineralocorticoid receptor antagonists (MRAs) using non-steroidal molecules have been developed to selectively increase benefits and decrease adverse effects through changes in receptor affinity and tissue tropism; The Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease (FIDELIO-DKD) trial and the Finerenone in Reducing Cardiovascular Mortality and Morbidity in Diabetic Kidney Disease (FIGARO-DKD) trial revealed favorable properties of renal protection [16, 17]. Thus, finerenone may be a promising drug for the unmet medical need of DKD. This review aims to discuss the latest DKD treatment using four types of drugs, which can be called the “fantastic four”. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by the author.
Effects of ACEIs and ARBs on DKD
The RAS plays a significant role in the development of DKD. The angiotensin-converting enzyme converts angiotensin I to angiotensin II, which increases aldosterone secretion, antidiuretic hormone (vasopressin) secretion, microvascular vasoconstriction, and sympathetic nerve activity, leading to inflammation and activation of fibrosis signaling. Activation of the angiotensin II–protein kinase C (PKC) pathway in the glomeruli is associated with processes that increase the extracellular matrix, thicken the basement membrane, increase endothelial dysfunction, and activate cytokines or transforming growth factor-β (TGFβ) [18, 19]. Furthermore, we have reported that the angiotensin II-activated TGFβ/Smad1 pathway increases the extracellular matrix in mesangial cells. Olmesartan, an ARB, directly inhibits Smad1 expression, thereby decreasing mesangial expansion in DKD [3, 5].
The Reduction of Endpoints in Non-insulin-dependent diabetes mellitus with the Angiotensin II Antagonist Losartan (RENAAL) trial is a randomized comparison of the losartan-treated group (50–100 mg/day) versus the placebo group. The primary endpoints of the study were creatinine doubling, end-stage kidney disease (ESKD), or death. Administration of losartan decreased the risk of creatinine doubling and ESKD by 25% and 28%, respectively [9] (Table 1). The Irbesartan Diabetic Nephropathy Trial (IDNT) had three arms: irbesartan, amlodipine, and placebo, and the primary endpoints were creatinine doubling, ESKD development, and death. The primary endpoints, particularly creatinine doubling, demonstrated a relatively lower risk with the irbesartan group than with the placebo group [10] (Table 1). However, despite this promising progress, DKD still exhibits residual cardiorenal morbidity and mortality. Thus, the next obvious question was whether the combination of ACEIs and ARBs would provide additional benefits. The Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) compared telmisartan, ramipril, or both in patients at high risk for vascular events and RAS inhibition. The combination of ACEIs and ARBs did not improve outcomes and was associated with an increased risk of serious adverse events such as acute kidney injury, hyperkalemia, or syncope, and therefore cannot be recommended in DKD [20].
Effects of SGLT2 Inhibitors on DKD
The EMPA-REG Outcome trial compared empagliflozin with placebo in patients with type 2 diabetes who were at high risk for cardiovascular events. The primary composite outcomes were death from cardiovascular diseases, nonfatal myocardial infarction, or nonfatal stroke. The pre-specified secondary analysis of the EMPA-REG Renal outcome trial revealed that empagliflozin decreased the risk of incident or worsening DKD by 39% (hazard ratio (HR) in the empagliflozin group, 0.61; 95% confidence interval (CI) 0.53–0.70; P < 0.001); the risk of creatinine doubling reduced significantly by 44%. Moreover, the risk of renal replacement therapy, including hemodialysis initiation, was significantly decreased by 55% in the study [11]. The subgroup findings of the EMPA-REG Renal outcome trial, including the patients with overt DKD (defined as a urinary albumin-to-creatinine ratio greater than 300 mg/g creatinine), revealed that empagliflozin significantly decreased the risk of the hard renal composite endpoint (defined as an estimated glomerular filtration rate (eGFR) of less than 15 mL/min/1.73 m2, sustained creatinine doubling from baseline levels, induction of renal replacement therapy, or renal death (HR in the empagliflozin group, 0.40; 95% CI 0.21–0.77) [21] (Table 1).
In the CREDENCE trial in DKD, long-term treatment with canagliflozin demonstrated renal protection effects in patients with eGFR between 30 and 90 mL/min/1.73 m2 (mean eGFR 56 mL/min/1.73 m2), urinary albumin-to-creatinine ratio between 300 and 5000 mg/g, and receiving the maximum dose of RAS inhibitors. Canagliflozin decreased the risk of a primary outcome, which was defined as ESKD (initiation of dialysis, renal transplantation, or sustained eGFR of less than 15 mL/min/1.73 m2), creatinine doubling, or death from renal or cardiovascular causes by 30% (HR in the canagliflozin group, 0.70; 95% CI 0.59–0.82; P = 0.00001) [12] (Table 1). Furthermore, the DAPA-CKD trial has recently evaluated dapagliflozin in patients with CKD, regardless of the presence or absence of diabetes. In this study, dapagliflozin significantly reduced the risk of the composite endpoint by a 50% reduction in eGFR, ESKD, and renal or cardiovascular death in patients with or without diabetes (HR in the dapagliflozin group, 0.50; 95% CI 0.35–0.72) [13] (Table 1).
Several reno-protective mechanisms by SGLT2 inhibitors have been proposed. The regulation of tubuloglomerular feedback, which maintains the eGFR by adjusting the preglomerular arteriole tone; a high concentration of sodium chloride constricts afferent arterioles, thereby decreasing the eGFR [22]. Administration of SGLT2 inhibitors increases sodium supply to the macula densa. Subsequently, tubuloglomerular feedback modulates arteriolar tone and decreases glomerular flow, thereby normalizing glomerular hyperfiltration [23,24,25].
Inflammation and oxidative stress play a significant role in the development and progression of CKD [19, 26, 27]. Additionally, they can increase mesangial expansion and interstitial fibrosis. The nuclear factor, NF-kappa-B has been reported to stimulate cytokine expression via reactive oxygen species and PKCβ [18, 28]. Furthermore, we have reported that tumor necrosis factor-α has a crucial role in the development of microvascular complications including DKD [29, 30]. Treatment with empagliflozin reduced inflammation and subsequently decreased glomerular extracellular matrix accumulation-related signaling pathway, TGFβ, and connective tissue growth factor [31]. However, the precise mechanism underlying the anti-inflammatory effect of SGLT2 inhibitors is unclear. One possible explanation is that SGLT2 inhibitors increase mild ketosis; β-hydroxybutyrate, a type of ketone body, interacts with G-protein-coupled receptors or activates other signaling pathways [32]. Interestingly, intravenously administered β-hydroxybutyrate significantly increases the expression of catalase, FOXO3a, and manganese dioxide, which are anti-inflammatory and anti-oxidative stress molecules in rodents’ kidneys [33].
Effects of Incretin-Based Therapeutic Agents on DKD
GLP-1, a type of intestinal incretin hormone, stimulates a glucose-dependent insulin response [34]. GLP-1 acts via GLP-1 receptors, which are abundant in the gastrointestinal tract and in many other tissues, including glomerular endothelial cells [18, 35,36,37]. We reported that exendin-4, a GLP-1 receptor agonist, activates the cyclic adenosine monophosphate/protein kinase A pathway, increases phosphor-c-Raf (Ser259) levels, and potentially inhibits phosphor-c-Raf (Ser338)/phosphor-Erk1/2/plasminogen activator inhibitor-1 signaling activated by angiotensin II and PKCβ. Furthermore, PKCβ increases levels of ubiquitinated GLP-1 receptor and decreases protein levels of GLP-1 receptor in the glomeruli [18]. Additionally, we revealed that GLP-1 receptor agonists decreased inflammatory markers such as CD68 and CXCL2 in the renal cortex of diabetic mice. GLP-1 decreases albuminuria and ameliorates mesangial expansion, which is a typical pathological feature of DKD [18, 38]. GLP-1 also inhibits TGFβ signaling, which is related to mesangial expansion or interstitial fibrosis in DKD [18, 38]. Interestingly, we have confirmed that protein levels of GLP-1 receptor were significantly decreased in the renal cortex of patients with long-term type 1 diabetes (The Joslin medalist Program at Harvard University; Mima A and King GL, unpublished observation). The LEADER trial is a large clinical study that assesses the long-term effects of liraglutide on renal outcomes in patients with type 2 diabetes, and this supports the results of the basic experiments in this study. The renal outcome was a composite of new-onset persistent macroalbuminuria, persistent serum creatinine doubling, ESKD, or death due to renal disease. Changes in the eGFR and albuminuria were also analyzed. Renal outcomes occurred in fewer patients in the liraglutide group than in the placebo group (268 of 4668 versus 337 of 4672, HR 0.78; 95% CI 0.67–0.92; P = 0.003). This was mainly due to new onset of persistent macroalbuminuria, which occurred in fewer patients in the liraglutide group than in the placebo group (161 versus 215 patients, HR 0.74; 95% CI 0.60–0.91; P = 0.004) [14] (Table 1).
We reported that inhibition of insulin/insulin receptor substrate-1 signaling was recognized in the glomeruli of patients with DKD [26, 39]. In our previous study, diabetes increased podocyte apoptosis in DKD through the activation of the Src homology-2 domain containing phosphatase-1, resulting in vascular endothelial growth factor (VEGF) resistance [40]. Insulin enhances VEGFA expression; thus, the loss of insulin signaling on glomeruli may contribute to the development of DKD. It is reported that several DPP4 inhibitors improved renal pathology in DKD. However, as GLP-1 is rapidly degraded by DPP4, DPP4 inhibitor-induced reno-protective effects could be a function of their pleiotropic actions. Interestingly, a DPP4 inhibitor, linagliptin, improved insulin-induced phosphorylation of insulin/insulin receptor substrate-1 and Akt, which was inhibited in the glomeruli of DKD, improving both renal pathology and function. The Kelch-like ECH-associated protein 1 or nuclear factor erythroid 2-related factor 2 (Nrf2) pathway is one of the most important intrinsic anti-oxidative systems [39]. Furthermore, our previous study revealed that linagliptin increased Nrf2 levels in podocytes, partially contributing to the reduction of podocyte apoptosis [39]. Another important mechanism of developing DKD is the endothelial-to-mesenchymal transition (End-MT) in glomerular endothelial cells [41, 42]. Linagliptin has been reported to decrease renal fibrosis following DKD-induced End-MT through an effect mediated by microRNA [41]. A recently published large clinical trial, CARMELINA, established that renal endpoints using linagliptin revealed that linagliptin administration prevented the progression of microalbuminuria in overt proteinuria in patients with type 2 diabetes; the linagliptin group (763/2162; 21.4 per 100 person-years) versus the placebo group (819/2129; 24.5 per 100 person-years; HR 0.86; 95% CI 0.78–0.95; P = 0.003) [15] (Table 1).
Effects of MRAs on DKD
Overactivation of mineralocorticoid receptors causes inflammation and fibrosis in DKD [43]. Furthermore, long-term administration of ACEIs and ARBs paradoxically increases aldosterone levels. This phenomenon is termed aldosterone breakthrough, leading to renal injury. Thus, combination therapy using ACEIs and ARBs with MRAs seems to be promising for DKD treatment [44]. Previous meta-analyses have revealed that the addition of MRAs to RAS inhibitors significantly decreased blood pressure and proteinuria in DKD. However, there was an increased risk of hyperkalemia [45, 46]. In contrast to steroidal MRAs such as spironolactone or eplerenone, selective non-steroidal MRAs such as finerenone act as an inverse agonist, inhibiting cofactor mobilization to the mineralocorticoid receptor in the absence of aldosterone [47]. In addition, the gene regulation profile by finerenone is different from that of steroid-based MRAs; finerenone has more potent antifibrotic effects than eplerenone [48].
Finerenone prevents heart and renal damage in hypertensive or chronic heart failure after coronary artery ligation in rodent models. Furthermore, these cardiorenal protective effects were independent of finerenone’s ability to reduce blood pressure [49]. An increase in oxidative stress plays a significant role in the development of DKD [19, 50, 51]. Importantly, finerenone significantly reduced oxidative stress and TGFβ expression and suppressed tubulointerstitial fibrosis in an ischemia–reperfusion rodent model [52]. Finerenone reduces oxidative stress by inhibiting Rac1 activation and subsequent mineralocorticoid receptor signaling pathway in vascular smooth muscle cells [53]. Several clinical studies indicate favorable results for DKD treatment, supporting the results of basic research. The Mineralocorticoid Receptor Antagonist Tolerability Study-Diabetic Nephropathy (ARTS-DN) enrolled 823 patients with type 2 diabetes with a urinary albumin-to-creatinine ratio greater than 30 mg/g creatinine, eGFR of more than 30 mL/min/1.73 m2, and treated with RAS inhibitors [54]. These patients were randomly assigned to the finerenone (1–25 mg/day) or placebo groups and were followed up for 90 days. Finerenone significantly reduced the urinary albumin-to-creatinine ratio compared to placebo as follows: 0.76 (90% CI 0.65–0.88; P = 0.001; 10 mg/day) and 0.62 (90% CI 0.54–0.72; P < 0.001; 20 mg/day) (Table 1). Additionally, the decrease in albuminuria was not associated with eGFR and blood pressure [54]. Thus, finerenone-induced reno-protective effects may be independent of its hemodynamic effects. The FIDELIO-DKD trial assessed whether finerenone slows CKD progression or reduces cardiovascular morbidity and mortality in patients with type 2 diabetes treated with a maximal dose of ACEIs or ARBs [16].
Primary endpoints included renal failure (defined as ESKD or eGFR of less than 15 mL/min/1.73 m2), a decrease in eGFR of more than 40% from baseline, and death due to renal causes. The primary outcome was significantly lower in the finerenone group (HR 0.82; 95% CI 0.73–0.93; P = 0.001). The adverse effects of hyperkalemia occurred in 11.8% of patients in the finerenone group compared to 4.8% in the placebo group [16] (Table 1).
The FIGARO-DKD trial assessed the efficacy of finerenone on cardiovascular and renal outcomes and its safety in patients with type 2 diabetes with CKD [17]. Participants in this trial were grouped into urinary albumin-to-creatinine ratio greater than 30–300 mg/g creatinine with eGFR 25–90 mL/min/1.73 m2 and urinary albumin-to-creatinine ratio greater than 300–5000 mg/g creatinine with eGFR of more than 60 mL/min/1.73 m2, indicating that FIGARO-DKD included more patients with early-stage CKD and type 2 diabetes than FIDELIO-DKD. The secondary composite outcome, similar to the primary composite endpoint of FIDELIO-DKD, was 9.5% and 10.8% in the finerenone and placebo groups, respectively (HR 0.87; 95% CI 0.76–1.01). These findings clearly indicate that finerenone has reno-protective effects in DKD [17] (Table 1).
Conclusions
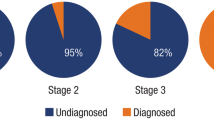
For many years, RAS inhibitors were the only treatment for DKD. However, recent studies indicate that SGLT2 inhibitors and incretin-based therapeutic agents can provide reno-protective effects, which may complement the efficacy of RAS inhibitors. In addition, finerenone, a non-steroidal MRA, is a promising drug owing to its ability to produce anti-inflammatory and antifibrotic effects. Therefore, the treatment of DKD in the future will include four types of drugs: RAS inhibitors, SGLT2 inhibitors, incretin-based therapeutic agents, and MRAs (Fig. 1). Possible administration methods of these four drugs in view of renal function are shown in Fig. 2.
Recommended drug combinations for DKD treatment. ARNI angiotensin receptor–neprilysin inhibitor, ESAs erythropoiesis-stimulating agents, HIF-PHIs hypoxia-inducible factor–prolyl hydroxylase domain inhibitors, HFrEF heart failure with reduced ejection fraction, ACEIs angiotensin-converting enzyme inhibitors, ARBs angiotensin I receptor blockers, SGLT2 sodium-glucose co-transporter 2, DKD diabetic kidney disease, MRAs mineralocorticoid receptor antagonists
Evidence supporting use of RAS inhibitors, SGLT2 inhibitors, incretin-based therapeutic agents, and MRAs for DKD treatment as represented on the KDIGO heat map. The color code indicates risk category according to KDIGO [55]: green “low risk”, yellow “moderate risk”, orange “high risk”, and red “very high risk”. RAS renin–angiotensin system, SGLT2 sodium-glucose co-transporter 2, MRAs mineralocorticoid receptor antagonists, KDIGO Kidney Disease: Improving Global Outcomes
References
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–53.
Mima A, Matsubara T, Arai H, et al. Angiotensin II-dependent Src and Smad1 signaling pathway is crucial for the development of diabetic nephropathy. Lab Investig. 2006;86(9):927–39.
Qian Y, Feldman E, Pennathur S, Kretzler M, Brosius FC 3rd. From fibrosis to sclerosis: mechanisms of glomerulosclerosis in diabetic nephropathy. Diabetes. 2008;57(6):1439–45.
Mima A, Arai H, Matsubara T, et al. Urinary Smad1 is a novel marker to predict later onset of mesangial matrix expansion in diabetic nephropathy. Diabetes. 2008;57(6):1712–22.
Blythe WB. Captopril and renal autoregulation. N Engl J Med. 1983;308(7):390–1.
Heeg JE, de Jong PE, van der Hem GK, de Zeeuw D. Reduction of proteinuria by angiotensin converting enzyme inhibition. Kidney Int. 1987;32(1):78–83.
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329(20):1456–62.
Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9.
Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–60.
Wanner C, Inzucchi SE, Zinman B. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375(18):1801–2.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306.
Heerspink HJL, Stefansson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383(15):1436–46.
Mann JFE, Orsted DD, Brown-Frandsen K, et al. Liraglutide and renal outcomes in type 2 diabetes. N Engl J Med. 2017;377(9):839–48.
Rosenstock J, Perkovic V, Johansen OE, et al. Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the CARMELINA Randomized clinical trial. JAMA. 2019;321(1):69–79.
Bakris GL, Agarwal R, Anker SD, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020;383(23):2219–29.
Pitt B, Filippatos G, Agarwal R, et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N Engl J Med. 2021;385(24):2252–63.
Mima A, Hiraoka-Yamomoto J, Li Q, et al. Protective effects of GLP-1 on glomerular endothelium and its inhibition by PKCbeta activation in diabetes. Diabetes. 2012;61(11):2967–79.
Mima A. Inflammation and oxidative stress in diabetic nephropathy: new insights on its inhibition as new therapeutic targets. J Diabetes Res. 2013;2013: 248563.
de Boer IH, Caramori ML, Chan JCN, et al. Executive summary of the 2020 KDIGO Diabetes Management in CKD Guideline: evidence-based advances in monitoring and treatment. Kidney Int. 2020;98(4):839–48.
Wanner C, Inzucchi SE, Zinman B, et al. Consistent effects of empagliflozin on cardiovascular and kidney outcomes irrespective of diabetic kidney disease categories: insights from the EMPA-REG OUTCOME trial. Diabetes Obes Metab. 2020;22(12):2335–47.
Vallon V, Richter K, Blantz RC, Thomson S, Osswald H. Glomerular hyperfiltration in experimental diabetes mellitus: potential role of tubular reabsorption. J Am Soc Nephrol. 1999;10(12):2569–76.
Cherney DZ, Perkins BA, Soleymanlou N, et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129(5):587–97.
Mima A. Renal protection by sodium-glucose cotransporter 2 inhibitors and its underlying mechanisms in diabetic kidney disease. J Diabetes Complicat. 2018;32(7):720–5.
Mima A. Sodium-glucose cotransporter 2 inhibitors in patients with non-diabetic chronic kidney disease. Adv Ther. 2021;38(5):2201–12.
Mima A, Ohshiro Y, Kitada M, et al. Glomerular-specific protein kinase C-beta-induced insulin receptor substrate-1 dysfunction and insulin resistance in rat models of diabetes and obesity. Kidney Int. 2011;79(8):883–96.
Mima A, Qi W, King GL. Implications of treatment that target protective mechanisms against diabetic nephropathy. Semin Nephrol. 2012;32(5):471–8.
Mima A. Diabetic nephropathy: protective factors and a new therapeutic paradigm. J Diabetes Complicat. 2013;27(5):526–30.
Mima A, Qi W, Hiraoka-Yamomoto J, et al. Retinal not systemic oxidative and inflammatory stress correlated with VEGF expression in rodent models of insulin resistance and diabetes. Investig Ophthalmol Vis Sci. 2012;53(13):8424–32.
Mima A, Yasuzawa T, King GL, Ueshima S. Obesity-associated glomerular inflammation increases albuminuria without renal histological changes. FEBS Open Bio. 2018;8(4):664–70.
Gallo LA, Ward MS, Fotheringham AK, et al. Once daily administration of the SGLT2 inhibitor, empagliflozin, attenuates markers of renal fibrosis without improving albuminuria in diabetic db/db mice. Sci Rep. 2016;6:26428.
Gambhir D, Ananth S, Veeranan-Karmegam R, et al. GPR109A as an anti-inflammatory receptor in retinal pigment epithelial cells and its relevance to diabetic retinopathy. Investig Ophthalmol Vis Sci. 2012;53(4):2208–17.
Shimazu T, Hirschey MD, Newman J, et al. Suppression of oxidative stress by beta-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 2013;339(6116):211–4.
Drucker DJ. The biology of incretin hormones. Cell Metab. 2006;3(3):153–65.
Bullock BP, Heller RS, Habener JF. Tissue distribution of messenger ribonucleic acid encoding the rat glucagon-like peptide-1 receptor. Endocrinology. 1996;137(7):2968–78.
Park CW, Kim HW, Ko SH, et al. Long-term treatment of glucagon-like peptide-1 analog exendin-4 ameliorates diabetic nephropathy through improving metabolic anomalies in db/db mice. J Am Soc Nephrol. 2007;18(4):1227–38.
Erdogdu O, Nathanson D, Sjoholm A, Nystrom T, Zhang Q. Exendin-4 stimulates proliferation of human coronary artery endothelial cells through eNOS-, PKA- and PI3K/Akt-dependent pathways and requires GLP-1 receptor. Mol Cell Endocrinol. 2010;325(1–2):26–35.
Mima A. Incretin-based therapy for prevention of diabetic vascular complications. J Diabetes Res. 2016;2016:1379274.
Mima A, Yasuzawa T, Nakamura T, Ueshima S. Linagliptin affects IRS1/Akt signaling and prevents high glucose-induced apoptosis in podocytes. Sci Rep. 2020;10(1):5775.
Mima A, Kitada M, Geraldes P, et al. Glomerular VEGF resistance induced by PKCdelta/SHP-1 activation and contribution to diabetic nephropathy. FASEB J. 2012;26(7):2963–74.
Kanasaki K, Shi S, Kanasaki M, et al. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes. 2014;63(6):2120–31.
Yasuzawa T, Nakamura T, Ueshima S, Mima A. Protective effects of eicosapentaenoic acid on the glomerular endothelium via inhibition of EndMT in diabetes. J Diabetes Res. 2021;2021:2182225.
Culver S, Li C, Siragy HM. Intrarenal angiotensin-converting enzyme: the old and the new. Curr Hypertens Rep. 2017;19(10):80.
Goenka L, Padmanaban R, George M. The ascent of mineralocorticoid receptor antagonists in diabetic nephropathy. Curr Clin Pharmacol. 2019;14(2):78–83.
Bolignano D, Palmer SC, Navaneethan SD, Strippoli GF. Aldosterone antagonists for preventing the progression of chronic kidney disease. Cochrane Database Syst Rev. 2014;4:CD007004.
Currie G, Taylor AH, Fujita T, et al. Effect of mineralocorticoid receptor antagonists on proteinuria and progression of chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol. 2016;17(1):127.
Grune J, Benz V, Brix S, et al. Steroidal and nonsteroidal mineralocorticoid receptor antagonists cause differential cardiac gene expression in pressure overload-induced cardiac hypertrophy. J Cardiovasc Pharmacol. 2016;67(5):402–11.
Grune J, Beyhoff N, Smeir E, et al. Selective mineralocorticoid receptor cofactor modulation as molecular basis for finerenone’s antifibrotic activity. Hypertension. 2018;71(4):599–608.
Kolkhof P, Delbeck M, Kretschmer A, et al. Finerenone, a novel selective nonsteroidal mineralocorticoid receptor antagonist protects from rat cardiorenal injury. J Cardiovasc Pharmacol. 2014;64(1):69–78.
Mima A. Hypoxia-inducible factor-prolyl hydroxylase inhibitors for renal anemia in chronic kidney disease: advantages and disadvantages. Eur J Pharmacol. 2021;912: 174583.
Mima A. Mitochondria-targeted drugs for diabetic kidney disease. Heliyon. 2022;8(2): e08878.
Lattenist L, Lechner SM, Messaoudi S, et al. Nonsteroidal mineralocorticoid receptor antagonist finerenone protects against acute kidney injury-mediated chronic kidney disease: role of oxidative stress. Hypertension. 2017;69(5):870–8.
Barrera-Chimal J, Andre-Gregoire G, Nguyen DinhCat A, et al. Benefit of mineralocorticoid receptor antagonism in AKI: role of vascular smooth muscle Rac1. J Am Soc Nephrol. 2017;28(4):1216–26.
Pitt B, Kober L, Ponikowski P, et al. Safety and tolerability of the novel non-steroidal mineralocorticoid receptor antagonist BAY 94-8862 in patients with chronic heart failure and mild or moderate chronic kidney disease: a randomized, double-blind trial. Eur Heart J. 2013;34(31):2453–63.
Kidney Disease Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter. 2013;(Suppl 3):1–150.
Acknowledgements
Funding
This work was supported by JSPS KAKENHI (Grant number 22K08368). The journal’s Rapid Service Fee was funded by the authors.
Authorship
The author meets the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, takes responsibility for the integrity of the work as a whole, and has given approval for this version to be published.
Author Contributions
The author contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by AM. The first draft of the manuscript was written by AM. The author read and approved the final manuscript.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by the author.
Disclosures
Akira Mima received a speaker honorarium from Kyowa Kirin, Mitsubishi Tanabe, Kowa, Bayer, Eli Lilly, Mochida, Sumitomo Pharma, Astra Zeneca, and Boehringer Ingelheim. Akira Mima also received research grants from Kyowa Kirin, Sumitomo Pharma, Otsuka, Torii, Daiichi-Sankyo, Mitsubishi Tanabe, Mochida, Boehringer Ingelheim, and Eli Lilly.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mima, A. A Narrative Review of Diabetic Kidney Disease: Previous and Current Evidence-Based Therapeutic Approaches. Adv Ther 39, 3488–3500 (2022). https://doi.org/10.1007/s12325-022-02223-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02223-0