Abstract
Introduction
Long-term, real-world safety and effectiveness data are required to support biosimilar use. This analysis pooled 5-year findings from observational studies of infliximab biosimilar CT-P13 treatment in patients with rheumatoid arthritis (RA), inflammatory bowel disease (IBD), and ankylosing spondylitis (AS).
Methods
Patients enrolled in the CT-P13 4.2, 4.3, or 4.4 Korea/European Union registries were analysed if they had initiated infliximab treatment with CT-P13 (CT-P13 group) or had switched from reference infliximab to CT-P13 (switched to CT-P13 group). The primary objective was to investigate long-term safety by evaluating adverse events of special interest (AESIs) per the CT-P13 risk-management plan. Incidence rates per 100 patient-years (PYs) were calculated. Additional long-term safety endpoints, immunogenicity (assessments optional), and effectiveness were evaluated.
Results
Overall, 736 patients (642 CT-P13; 94 switched to CT-P13) were analysed. Median (range) exposure to CT-P13 was 19.433 (0.03–63.11) months overall. The incidence of treatment-emergent adverse events was 69.0% (CT-P13 group) and 60.6% (switched to CT-P13 group). Infusion-related reaction/hypersensitivity/anaphylactic reaction was the most frequent AESI overall, with an incidence of 4.3828 per 100 PY (95% confidence interval: 3.3603–5.6185). For most AESIs, incidence rates per 100 PY were broadly comparable between treatment groups, considering overlapping 95% confidence intervals. At baseline, 42/445 (9.4%) and 21/59 (35.6%) evaluable patients in the CT-P13 and switched to CT-P13 groups, respectively, were antidrug antibody (ADA)-positive. After CT-P13 treatment during the study, 188/425 (44.2%) evaluable patients had ≥ 1 ADA-positive result, including 147/425 (34.6%) patients with negative or no ADA results reported at baseline. Effectiveness tended to increase over time for all indications.
Conclusion
The analysis did not identify any new safety findings for patients with RA, IBD, and AS treated with CT-P13 for up to 5 years in those who were infliximab-naïve at CT-P13 initiation, or those who had switched from reference infliximab to CT-P13.
Trial Registration
ClinicalTrials.gov identifiers: NCT02557295 (CT-P13 4.2; retrospectively registered on 23 September 2015); NCT02326155 (CT-P13 4.3; retrospectively registered on 25 December 2014); NCT02557308 (CT-P13 4.4; retrospectively registered on 23 September 2015).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Biosimilars can benefit healthcare systems by reducing the cost of biologic treatment, and long-term data are required to support their use. |
This analysis collected long-term safety and effectiveness data for CT-P13, the first biosimilar of infliximab, in patients with rheumatoid arthritis, inflammatory bowel disease, or ankylosing spondylitis in the real-world setting. |
The hypothesis was that there would be no safety issues for CT-P13, in comparison with established data for reference infliximab, whether patients were infliximab-naïve when initiating CT-P13 (CT-P13 group) or whether they had switched from reference infliximab to CT-P13 (switched to CT-P13 group). |
What was learned from the study? |
The analysis did not identify any new safety findings for patients treated with CT-P13 for up to 5 years in either the CT-P13 or switched to CT-P13 group, and there was a positive trend in effectiveness. |
Results were as anticipated, supporting the long-term safety of CT-P13 treatment in clinical practice; however, limitations of the observational studies (such as optional immunogenicity testing and variable numbers of evaluable patients) mean that further studies are warranted. |
Introduction
CT-P13 is an approved infliximab biosimilar. The intravenous (IV) formulation of CT-P13, CT-P13 IV, initially received marketing authorisation in the Republic of Korea (Korean Ministry of Food and Drug Safety; 2012), Europe [European Medicines Agency (EMA); 2013], and the US (US Food and Drug Administration; 2016) [1,2,3,4]. It is currently approved in 95 countries under the trade names Remsima®, Flammegis®, Inflectra®, Flixceli®, and Emisima® (all Celltrion, Incheon, Republic of Korea). CT-P13 IV is authorised for the same indications as reference infliximab: rheumatoid arthritis (RA), inflammatory bowel disease [IBD; encompassing adult and paediatric Crohn’s disease (CD) and ulcerative colitis (UC)], ankylosing spondylitis (AS), psoriatic arthritis (PsA), and plaque psoriasis (PsO) [1,2,3, 5,6,7]. A subcutaneous (SC) formulation of CT-P13, CT-P13 SC, has also been developed [8], and has received regulatory approval from the EMA for the treatment of RA, CD, UC, AS, PsA, and PsO in adult patients [2]. CT-P13 SC is currently approved in 32 countries worldwide.
Regulatory submissions for CT-P13 IV were based on the findings of two pivotal, randomised controlled trials (RCTs). The phase 1 PLANETAS study compared CT-P13 with reference infliximab in patients with active AS and found CT-P13 to be well tolerated, with a pharmacokinetic profile equivalent to that of reference infliximab; comparable efficacy was also observed [9]. In the phase 3 PLANETRA study, in which CT-P13 was compared with reference infliximab in patients with RA, CT-P13 was well tolerated and demonstrated equivalent efficacy to reference infliximab, with a comparable pharmacokinetic profile and immunogenicity [10].
While RCTs are the gold standard for assessing healthcare intervention efficacy and safety [11, 12], non-randomised, observational studies conducted in larger, more heterogenous cohorts can provide valuable additional information. Long-term safety and effectiveness data can be collected with cohort sizes sufficient to detect rare adverse events (AEs) [13, 14]. A pooled analysis of data from six observational studies of CT-P13 IV in patients with RA, IBD, AS, PsA, and PsO, with a mean CT-P13 exposure of 267 days, demonstrated that CT-P13 IV had a similar safety profile to that reported in previous studies of reference infliximab [15]. However, there remains a need to establish the long-term safety profile of CT-P13 IV, and to evaluate its long-term effectiveness, in real-world practice, both for patients who initiate infliximab therapy with CT-P13 IV and for those who switch to CT-P13 IV from the reference product. Indeed, recommendations from the Task Force on the Use of Biosimilars to Treat Rheumatological Diseases have noted the value of registry data on the outcomes of switching, and how such data can support healthcare professionals when making treatment decisions about biosimilars in clinical practice [16]. This report evaluates the long-term safety and effectiveness of CT-P13 IV in the post-marketing setting, with the primary objective to investigate its safety profile. We report final analyses for three observational studies of CT-P13 IV (hereafter referred to as CT-P13) in patients with RA, IBD, and AS, treated for up to 5 years.
Methods
Patients and Treatment
Patients included in this analysis were enrolled in one of three phase 4, longitudinal, observational studies of up to 5 years’ duration. The CT-P13 4.2 Korea/European Union (EU) registry (NCT02557295) evaluated patients with RA between November 2013 and March 2020. The study compared the safety and effectiveness of CT-P13 with other anti-tumour necrosis factor (TNF) agents or non-biologic therapies. The CT-P13 4.3 Korea/EU registry (NCT02326155) evaluated the safety and effectiveness of CT-P13 in patients with IBD (active CD, fistulising CD, or UC) between April 2014 and February 2020. The CT-P13 4.4 Korea/EU registry (NCT02557308) compared the safety and effectiveness of CT-P13 with other anti-TNF agents in patients with AS between August 2014 and February 2020. Full eligibility criteria for each study are provided in the Supplementary Methods. Ethics approval information is included in the ‘Compliance with ethics guidelines’ section and in Table S1.
The present analysis included only those patients enrolled in the CT-P13 4.2, 4.3, or 4.4 studies who had been treated with CT-P13. CT-P13 was administered intravenously according to the prescribing recommendations contained in the relevant country-/region-specific authorised product information for each indication. Permitted concomitant medications included pretreatment with antihistamines, hydrocortisone, and/or paracetamol. For patients with RA (in the CT-P13 4.2 study), methotrexate was co-administered with CT-P13.
Objectives
The primary objective of this analysis was to investigate the long-term safety of CT-P13 by evaluation of adverse events of special interest (AESIs) up to 5 years. Secondary objectives were to evaluate additional long-term safety endpoints, and the immunogenicity and effectiveness of CT-P13, over up to 5 years.
Endpoints and Assessments
Duration of exposure to CT-P13 was calculated as follows: (date of last CT-P13 dose – date of the first CT-P13 dose + 1)/365.25 × 12, regardless of dose modifications or interruptions. For patients switching to CT-P13 from reference infliximab, the date of the first CT-P13 dose was recorded as the first dosing date.
Safety endpoints included the proportion of patients with AESIs (Supplementary Methods; Table S2), which were selected based on the CT-P13 risk-management plan [17, 18]. AESIs comprised congestive heart failure, opportunistic infections (excluding tuberculosis), serious infections including sepsis (excluding opportunistic infections and tuberculosis), tuberculosis, haematological reactions, systemic lupus erythematosus (SLE)/lupus-like syndrome, lymphoma [excluding hepatosplenic T-cell lymphoma (HSTCL)], hepatobiliary event, sarcoidosis/sarcoid-like reactions, malignancies (excluding lymphoma), pregnancy exposure, infusion-related reactions (IRRs)/hypersensitivity/anaphylactic reactions, hepatitis B reactivation, serum sickness (delayed hypersensitivity reaction), demyelinating disorders, HSTCL, leukaemia, skin cancer, and serious infusion reactions during a re-induction regimen following disease flare. Any AESIs not captured in all three studies (Table S2) were excluded from the pooled analysis.
Additional safety endpoints included CT-P13-associated treatment-emergent adverse events (TEAEs), serious TEAEs, TEAEs leading to permanent study drug discontinuation, and TEAEs leading to death. TEAEs were defined as AEs that occurred after the first dose of CT-P13, or that occurred before the first dose of CT-P13 but worsened in severity after the first dose. Safety data were retrieved from patient medical records collected as part of routine clinical practice. Data were collected from commencement of treatment with CT-P13 to the end of study (EOS). If a patient withdrew from the study prior to completion, an EOS visit was made 8 weeks after the last dose; if the full 5-year study period was completed, EOS was considered the last visit. All TEAEs were coded using the Medical Dictionary for Regulatory Affairs, version 22.1.
For patients who opted in by completing an additional informed consent form for sample collection, blood samples were collected prior to study drug administration for immunogenicity testing at baseline, every 6 or 12 months, and at the EOS visit. Serum anti-drug antibodies (ADAs) were measured using a validated enzyme-linked immunosorbent assay.
In terms of effectiveness, in patients with RA, disease activity score in 28 joints (DAS28) by erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were assessed at day 0 and then every 6 months. For patients with IBD, effectiveness assessments were performed using indication-specific tools at day 0 and then every 6 months. These tools were the Crohn’s Disease Activity Index (CDAI; adult patients with moderate to severe active CD), the Paediatric Crohn’s Disease Activity Index (PCDAI; paediatric patients with severe active CD), the number of draining fistulas (adult patients with fistulising active CD), total and partial Mayo scores (adult patients with moderate to severe active UC), and the Paediatric Ulcerative Colitis Activity Index (PUCAI; paediatric patients with severe active UC). For patients with AS, effectiveness was assessed using the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) at day 0 and then every 6 months.
Statistical Analyses
The CT-P13 4.2 study aimed to recruit 450 patients with RA receiving CT-P13. The study also aimed to recruit 50 patients with RA receiving non-biologic treatment and 450 patients with RA receiving other anti-TNF drugs: these patients (receiving non-biologic treatment or other anti-TNF drugs) are not included in this analysis. The CT-P13 4.3 study aimed to recruit at least 500 patients with IBD receiving CT-P13, based on an exploratory descriptive approach. The CT-P13 4.4 study aimed to recruit approximately 500 patients with AS receiving CT-P13, based on an exploratory descriptive approach; the study also aimed to recruit 500 patients receiving other anti-TNF drugs (these patients are not included in the current analysis). The number of patients enrolled in each of the CT-P13 cohorts was sufficient to detect AEs occurring at a frequency of 1%.
Patients were included in either the CT-P13 group or the switched to CT-P13 treatment group. Patients treated with CT-P13 who had never received reference infliximab, including those who had initiated treatment with CT-P13 or who had switched to CT-P13 from a non-biologic treatment, were included in the CT-P13 group. Patients previously treated with reference infliximab who had switched to CT-P13 were analysed in the switched to CT-P13 group. For this analysis, the safety population comprised all patients who had received at least one dose of CT-P13 during the study. Safety data were analysed in the pooled safety population as well as by treatment group (overall, CT-P13, or switched to CT-P13) and by indication (RA, IBD, or AS). The effectiveness population comprised all patients who had received at least one dose of CT-P13 during any dosing period and had at least one post-treatment effectiveness result. Effectiveness data were analysed within each indication [RA, IBD (in one of five subgroups), or AS] by treatment group (overall, CT-P13, or switched to CT-P13).
Continuous variables were reported using descriptive statistics [n, mean (standard deviation; SD), median (range)]. Categorical variables were reported using frequencies and percentages. For each AESI, incidence rates per 100 patient-years (PYs) and corresponding 95% confidence intervals (CIs) were calculated as 100 × the number of patients with the AESI / the sum of treatment duration (years) for each patient. Formal hypothesis testing was not performed. Statistical analyses were conducted using SAS software, v.9.4 (SAS Institute, Cary, NC, USA).
Results
Patients
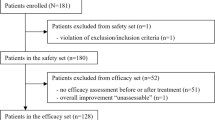
For the CT-P13 4.2 study, 119 patients who received CT-P13 (including 8 patients who switched from reference infliximab) were included in the analysis (Fig. 1a). For the patients included in this analysis, the first patient’s initial treatment visit was on 26 December 2013 and the last patient visit was on 2 March 2020. The median (range) time to study discontinuation for patients with RA was 413 (2–1640) and 382 (15–659) days in the CT-P13 and the switched to CT-P13 groups, respectively. In the CT-P13 4.3 study, a total of 470 patients with IBD were enrolled and received CT-P13; 63 patients had switched from reference infliximab (Fig. 1b). Patient disposition for the five separate IBD indications is shown in Fig. S1. The first patient’s initial visit was on 17 April 2014 and the last patient visit was on 28 February 2020. The median (range) time to study discontinuation for patients with IBD was 868 (1–1800) and 858 (39–1856) days in the CT-P13 and the switched to CT-P13 groups, respectively. For the CT-P13 4.4 study, 147 patients who received CT-P13 (including 23 patients who switched from reference infliximab) were included in the analysis (Fig. 1c). Of those included in this analysis, the first patient’s initial visit was on 13 August 2014 and the last patient visit was on 28 February 2020. The median (range) time to study discontinuation for patients with AS was 397 (20–1693) and 484 (57–680) days in the CT-P13 and the switched to CT-P13 groups, respectively. Overall, the most frequent reason for discontinuation was study closure, since all three studies were closed.
The median duration of CT-P13 exposure was comparable between the CT-P13 and the switched to CT-P13 groups at 19.811 and 16.476 months, respectively (Table 1). The median duration of CT-P13 exposure was also similar between treatment groups within each indication.
Overall, 736 patients were included in the analysis, with 642 in the CT-P13 group and 94 in the switched to CT-P13 group (Table 2). Baseline characteristics were generally well balanced between the CT-P13 and the switched to CT-P13 groups. Overall, the median (range) age was 38.0 (7–81) years; this was higher for patients with RA than IBD or AS. Just over half of the patients (57.9%) were male; however, the majority of patients with RA (76.5%) were female. Nearly two-thirds of patients (60.1%) were Asian, although 53.8% of patients with IBD were White. All patients were enrolled in the EU and Korea, with 39.9% from Europe. The median (range) time since diagnosis was 3.7 (0.0–42.2) years overall; this was longer in the switched to CT-P13 group versus the CT-P13 group. Overall, 44.2% of patients had received ≥ 1 prior biologic: 6.7%, 62.6%, and 15.6% of patients with RA, IBD, and AS, respectively.
Safety
Overall, IRR/hypersensitivity/anaphylactic reaction was the most frequent AESI, with an incidence of 4.3828 per 100 PY (95% CI: 3.3603–5.6185) (Table 3). Congestive heart failure, opportunistic infections (excluding tuberculosis), SLE/lupus-like syndrome, lymphoma (excluding HSTCL), and sarcoidosis/sarcoid-like reactions each occurred in one patient only. The incidence of serious infections including sepsis (excluding opportunistic infections and tuberculosis) was comparable between the CT-P13 and the switched to CT-P13 groups. Haematological reactions, hepatobiliary events, malignancies (excluding lymphoma), and pregnancy exposure occurred slightly more frequently in the switched to CT-P13 versus the CT-P13 group, although 95% CIs for incidence per 100 PY overlapped. The converse was observed for tuberculosis and IRR/hypersensitivity/anaphylactic reaction. For the AESI of tuberculosis, patients with latent tuberculosis could be enrolled in the study on the condition that they had either completed or intended to complete the entire course of tuberculosis treatment. Therefore, some patients who had a positive interferon-γ release assay (IGRA) result at screening were enrolled. After the first dose of CT-P13 during the study, overall, 12 (10.1%) patients with RA experienced IGRA conversion, which was reported as a TEAE for 7 (5.9%) patients. Four (0.9%) and four (2.7%) patients with IBD and AS, respectively, experienced IGRA conversion during the study.
The incidence of AESIs was generally comparable between indications (Table 3). Serious infections including sepsis (excluding opportunistic infections and tuberculosis), tuberculosis, and IRR/hypersensitivity/anaphylactic reaction occurred more frequently in patients with RA than IBD or AS. Haematological reactions and IRR/hypersensitivity/anaphylactic reaction occurred less frequently in patients with AS, in comparison with other indications. However, in all cases, there was some overlap between indications in the 95% CIs for incidence per 100 PY.
Overall, slightly higher proportions of patients in the CT-P13 group versus the switched to CT-P13 group experienced TEAEs (69.0% vs. 60.6%) or study drug-related TEAEs (25.2% vs. 19.1%) (Table 4). The incidence of serious TEAEs and TEAEs leading to discontinuation was comparable between groups. Overall, there were six TEAEs leading to death. The incidences of TEAEs, serious TEAEs, and TEAEs leading to discontinuation were comparable between patients with RA and IBD, while rates were lower for patients with AS. The majority of TEAEs were grade 1–2 in intensity in both the CT-P13 and the switched to CT-P13 groups (Table S3). Most grade 4–5 TEAEs were considered to be unrelated to the study drug: one study drug-related grade 4 TEAE of IRR and one study drug-related grade 5 TEAE of sepsis were reported in the CT-P13 group.
Immunogenicity
Since immunogenicity testing was optional, ADA results were not available for all patients. In the pooled safety analysis population, most patients were ADA-negative at baseline [435/504 (86.3%) patients with ADA results] (Table S4). A lower proportion of patients were ADA positive at baseline in the CT-P13 group [42/445 (9.4%)] compared with the switched to CT-P13 group [21/59 (35.6%)]. After patients had received CT-P13 treatment during the study, 188/425 (44.2%) evaluable patients had ≥ 1 ADA-positive result, including 147/425 (34.6%) patients who had a negative ADA result or no result reported at baseline.
Across indications, most patients were ADA-negative at baseline, ranging from 81.6% (226/277) of evaluable patients with IBD to 94.9% (94/99) of evaluable patients with RA (Table S4). After patients had received CT-P13 treatment during the study, 65.4% (51/78), 31.3% (72/230), and 55.6% (65/117) of evaluable patients with RA, IBD, and AS, respectively, had ≥ 1 ADA-positive result.
Effectiveness
Patients with RA
Overall, mean DAS28-CRP and DAS28-ESR decreased from baseline to week 30 and remained relatively consistent throughout the study (Table S5). In general, the proportion of patients achieving remission according to DAS28-CRP (Fig. 2a) and DAS28-ESR (Fig. 2b) criteria increased over the study period. The overall results predominantly reflect findings in the CT-P13 group as there were only three evaluable patients in the switched to CT-P13 group. Few patients were evaluable from week 78 (none in the switched to CT-P13 group).
Disease activity in patients with rheumatoid arthritis (RA) by a disease activity score in 28 joints (DAS28)–C-reactive protein criteria and b DAS28–erythrocyte sedimentation rate criteria (RA effectiveness population). aFrom week 150 to week 198, one patient (in the CT-P13 group) was evaluated and maintained remission
Patients with IBD
The IBD effectiveness analysis population included 339 patients (CT-P13, n = 289; switched to CT-P13, n = 50), divided into five subgroups.
For patients with moderate to severe active CD, overall, mean CDAI scores tended to decrease from baseline to month 48 (Table S6). Mean CDAI scores were higher at months 54 and 60, when there were few evaluable patients. The proportion of patients achieving a decrease of ≥ 70 points from baseline in CDAI score (Fig. 3a) or a decrease of ≥ 100 points from baseline in CDAI score (Fig. 3b) increased over time overall and in the CT-P13 group. Similar trends were observed in the switched to CT-P13 group at earlier time points; from month 30 onwards, response rates fell. While response rates were lower in the switched to CT-P13 group, there were fewer evaluable patients than in the CT-P13 group.
Proportion of patients with moderate to severe active Crohn’s disease (CD) achieving a a decrease of ≥ 70 points from baseline in Crohn’s Disease Activity Index score (CDAI-70) and b a decrease of ≥ 100 points from baseline in CDAI score (CDAI-100) (moderate to severe active CD effectiveness population)
Mean PCDAI scores were reduced at month 6 compared with baseline for patients with paediatric severe active CD, remaining relatively consistent at most time points thereafter (Table S7). Overall and in the CT-P13 group, proportions of patients achieving a clinical response according to PCDAI criteria remained relatively consistent between months 6 and 24 (Fig. 4); there were fewer evaluable patients from month 30 onwards. There was a lower proportion of PCDAI responders in the switched to CT-P13 group throughout, although there were fewer evaluable patients than in the CT-P13 group.
For patients with fistulising active CD, the mean number of draining fistulas tended to decrease over time (Table S8). Proportions of patients achieving a clinical response according to the number of draining fistulas tended to increase overall, as well as in the CT-P13 group, up to month 30 (Fig. 5). There were few evaluable patients from month 30 onwards.
Mean total and partial Mayo scores decreased from baseline to month 6 for patients with moderate to severe active UC, remaining relatively consistent thereafter (Table S9). The proportions of patients achieving a clinical response according to total Mayo score (Fig. 6a) and partial Mayo score (Fig. 6b) tended to increase over time overall and in the CT-P13 group. In the switched to CT-P13 group, there were few evaluable patients throughout the study.
There were two evaluable patients with paediatric severe active UC, both in the CT-P13 group. Mean PUCAI scores decreased between baseline and month 6 and between months 6 and 12 (Table S10). One of two evaluable patients achieved clinical response according to PUCAI at months 6 and 12, while at month 18, this was achieved by 1/1 evaluable patient.
Patients with AS
Overall, mean (SD) BASDAI scores decreased from baseline to month 6, with small further decreases observed over the study period (Table S11). Mean BASDAI scores were higher in the CT-P13 group than in the switched to CT-P13 group at baseline, with scores remaining slightly higher in the CT-P13 group up to month 18. The proportion of patients achieving a 50% decrease in BASDAI score from baseline (BASDAI-50) exceeded 50% at all time points evaluated overall and in the CT-P13 group (Fig. 7). There were fewer evaluable patients in the switched to CT-P13 group than the CT-P13 group throughout the study. Acknowledging this, proportions of patients achieving BASDAI-50 were lower in the switched to CT-P13 group at time points with evaluable patients (months 6 to 18).
Discussion
Safety and effectiveness data collected in real-world settings are needed to complement findings from RCTs. Findings from this analysis provide valuable insights into the long-term safety and effectiveness of the IV-administered infliximab biosimilar CT-P13 in clinical practice, across three immune-mediated inflammatory diseases (RA, IBD, and AS). These results reflect outcomes predominantly for patients who initiated infliximab treatment with CT-P13, with the analysis also including patients who switched from reference infliximab to CT-P13.
In this analysis, no safety findings were observed that have not been previously reported for the reference product, regardless of treatment group. This provides support for the long-term safety of CT-P13 treatment in routine clinical practice. Overall, long-term safety findings were comparable between the CT-P13 and the switched to CT-P13 groups, although a slightly higher proportion of patients experienced TEAEs in the CT-P13 group than in the switched to CT-P13 group. This is consistent with a post-marketing pooled analysis of CT-P13 treatment in patients with RA, IBD, AS, PsA, and PsO [15], which incorporated an earlier data-cut from the three registries contributing to the current analysis. The overall incidence of TEAEs was higher in the present analysis compared with the post-marketing pooled analysis (67.9% vs. 32.9%), reflecting the longer median duration of CT-P13 exposure (19.4 months vs. approximately 7.6 months) [15]. Most TEAEs recorded were grade 1–2 in intensity in the current analysis, consistent with results of the post-marketing pooled analysis in which most TEAEs were reported as ‘mild’ [15]. Overall, our findings were also consistent with conclusions drawn from the NOR-SWITCH trial, which noted that similar safety profiles could be expected for patients who had switched from reference infliximab to CT-P13 in comparison with those who had initiated and maintained treatment with either the reference product or the biosimilar [19].
The current analysis aimed to investigate the long-term incidence of AESIs identified based on the CT-P13 risk-management plan [17, 18]. Overall, the proportions of patients experiencing AESIs were not meaningfully different from results for TEAEs of special interest of IRR, tuberculosis, latent tuberculosis, and serious infections reported during the extension phases of the pivotal randomised controlled trials of CT-P13 in patients with AS or RA [20, 21]. This was also the case for the comparison with the proportions of patients experiencing AEs of IRR, tuberculosis, and infections during the extension phase of a study in Japanese patients with RA [22].
IRR/hypersensitivity/anaphylactic reaction was the most frequently recorded AESI in this study, with an incidence of 4.3828 per 100 PY (95% CI: 3.3603–5.6185) overall. This was higher in the CT-P13 group than the switched to CT-P13 group, although 95% CIs overlapped between groups. The incidence per 100 PY for IRRs was not calculated in the post-marketing pooled analysis; however, a greater proportion of patients who initiated infliximab treatment with CT-P13 compared with those who switched from reference infliximab to CT-P13 experienced IRRs (4.46% vs. 2.65%) [15], in keeping with the current findings. Infusion reactions also occurred more frequently in CT-P13-treated biologic-naïve patients with IBD, compared with patients undergoing a non-medical switch (i.e., switching for non-medical reasons such as institutional policy) from reference infliximab to CT-P13 (9.7% vs. 4.6%) in a Japanese post-marketing surveillance study [23]. In contrast, the PROSIT-BIO observational study of CT-P13-treated patients with IBD reported higher incidence rates for serious AEs of infusion reaction in patients who had switched from reference infliximab to CT-P13 when compared with biologic-naïve patients (14.3 vs. 9.6 per 100 PY), although an even higher incidence (49.6 per 100 PY) was reported for patients previously exposed to anti-TNF-α agents [24]. The overall incidence of IRR/hypersensitivity/anaphylactic reaction in the current study (8.4%) is similar to the ‘very common’ (≥ 1/10) incidence reported for IRRs in the EU reference infliximab prescribing information, which is based on clinical studies and post-marketing experience [6]. By indication, the proportions of patients with RA or IBD who experienced IRR/hypersensitivity/anaphylactic reaction in the current analysis were comparable to the proportions reporting infusion reactions with reference infliximab treatment in a Canadian registry, although, for AS, fewer patients reported these events in the current study [25]. The incidence rate for IRRs for biologic-naïve patients with RA from the same registry was 2.47 per 100 PY, lower than the corresponding rate in the current analysis [26]. By indication, the incidence of IRR/hypersensitivity/anaphylactic reaction was also broadly in keeping with previous real-world data for CT-P13 treatment. In a Korean registry of patients with RA and AS, 1.9% and 0.6% of patients, respectively, experienced IRRs (after a median CT-P13 treatment duration of 10.9 and 22.0 months, respectively) [27]. Similarly, 4.1% of patients with AS enrolled in the Korean College of Rheumatology Biologics registry reported CT-P13-related infusion or injection-site reactions after up to 4 years [28], compared with 2.0% in the current analysis. In IBD, the 9.1% of patients reporting IRR/hypersensitivity/anaphylactic reaction was comparable to overall findings from the PROSIT-BIO cohort for serious AEs of infusion reaction (6.9%) [24] and the Japanese post-marketing surveillance study (9.4%) [23]. However, such comparisons should consider that case definitions for IRRs are likely to vary between studies: for example, IRRs in clinical studies for reference infliximab were limited to AEs occurring during or within 1 h after infusion [6].
In this analysis, serious infections including sepsis (excluding opportunistic infection and tuberculosis) were experienced by 3.5% of patients overall, while opportunistic infections (excluding tuberculosis) were experienced by 0.1% of patients overall. The overall incidence per 100 PY (1.84) was consistent with real-world findings for CT-P13 from a Japanese post-marketing surveillance study of patients with IBD (2.26 [23]), and for reference infliximab, with an incidence of serious infections and infestations of 1.96 per 100 PY reported in a Canadian registry of patients with RA [26]. Overall, 2.0% of patients experienced tuberculosis in our analysis, with an incidence of 1.0603 per 100 PY (95% CI: 0.5935–1.7489). This is aligned with expectations based on the low frequency of tuberculosis or active tuberculosis reported in real-world studies of CT-P13 [23, 27,28,29] or reference infliximab [26, 29] treatment, and the reference infliximab EU prescribing information that describes tuberculosis as ‘uncommon’ (incidence ≥ 1/1000 to < 1/100) [6]. In this analysis, 0.8% of patients overall experienced malignancies (excluding lymphoma), 0.1% experienced lymphoma (excluding HSTCL), and there were no cases of HSTCL. This is consistent with the infrequent reports of malignancy in real-world studies of CT-P13 or reference infliximab in patients with RA or AS [27, 29], as well as the ‘rare’ (≥ 1/10,000 to < 1/1000) incidence of lymphoma reported in the EU reference infliximab prescribing information [6].
Immunogenicity is an important concern for biosimilars, particularly with respect to their potential interchangeability with their reference products [30]. Although ADA information was collected on an optional basis, limiting the conclusions that can be drawn about immunogenicity, most evaluable patients were ADA-negative both at baseline and after CT-P13 treatment during the study. Overall, 44.2% of evaluable patients had ADA-positive results after CT-P13 treatment during the study. To our knowledge, comparable long-term data for CT-P13 treatment in large observational studies are lacking. The ADA-positivity rate in this analysis was comparable to the 33.8% and 28.0% reported in two observational studies of CT-P13 treatment in patients with IBD after 54 and 30 weeks, respectively [31, 32]. Immunogenicity findings were also aligned with expectations based on the reference infliximab prescribing information, which reports an incidence of ADAs ranging from 2.9% to 38% in clinical trials, depending on the regimen and indication [6]. Consistent with an observational study of patients with IBD [33], overall, a greater proportion of patients with prior infliximab exposure versus those initiating infliximab treatment with CT-P13 were ADA-positive at baseline (35.6% vs. 9.4%) in the present analysis. The proportions of patients with ADA-positive results after CT-P13 treatment were similar between groups; thus, a greater proportion of patients in the CT-P13 group than in the switched to CT-P13 group became ADA-positive since their baseline assessments. Given the prior infliximab exposure of those in the switched to CT-P13 group, these findings are as anticipated. Therefore, the immunogenicity results from our analysis do not give rise to any safety concerns regarding switching from reference infliximab to CT-P13.
In general, effectiveness results tended to improve over time in RA, IBD, and AS indications. However, the observational study design limited the ability to collect additional information outside the routine procedures conducted during an office visit, meaning that the number of evaluable patients varied between effectiveness parameters and over time. For most effectiveness assessments, there were few evaluable patients in the switched to CT-P13 group. Overall, the number of evaluable patients decreased over time as patients discontinued the observational studies. These factors limit the conclusions that can be drawn about the long-term effectiveness of CT-P13, particularly for patients who had switched from reference infliximab to CT-P13.
The three longitudinal, prospective observational registry studies contributing to this analysis were conducted in heterogenous cohorts (comprising European and Korean patients) in real-world settings. Acknowledging the aforementioned limitations associated with observational studies, the analysis design allowed the primary objective of investigating the long-term safety profile of CT-P13 to be addressed. Pooling data from three observational studies, reflecting CT-P13 treatment in three different indications, means that our findings are representative of the real-world patient population for the majority of indications for CT-P13 treatment. However, all three studies were closed early, and the recruitment of patients with RA and AS did not meet the planned enrolment. In addition, immunogenicity results were available for relatively few patients. Therefore, further evaluation of the long-term safety and effectiveness of CT-P13 in these patient populations will be required.
Conclusions
This analysis did not identify any findings that would affect the risk–benefit balance for CT-P13. There were no safety findings that have not previously been observed for reference infliximab, both for patients who had initiated infliximab treatment with CT-P13 or who had switched from reference infliximab to CT-P13. Taken together, these findings provide further support for the long-term safety of CT-P13 treatment in routine clinical practice.
References
European Medicines Agency. Inflectra summary of product characteristics. 2020. https://www.ema.europa.eu/en/documents/product-information/inflectra-epar-product-information_en.pdf. Accessed 3 Jun 2021.
European Medicines Agency. Remsima summary of product characteristics. 2021. https://www.ema.europa.eu/en/documents/product-information/remsima-epar-product-information_en.pdf. Accessed 3 Jun 2021.
US Food and Drug Administration. Inflectra prescribing information. 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/125544s009lbl.pdf. Accessed 3 Jun 2021.
Ministry of Food and Drug Safety. Biological products: recombinant DNA products, Celltrion, Inc. https://www.mfds.go.kr/eng/brd/m_30/view.do?seq=69797. Accessed 3 Jun 2021.
Generics and Biosimilars Initiative. Biosimilar monoclonal antibody approved in Korea. 2012. http://www.gabionline.net/Biosimilars/News/Biosimilar-monoclonal-antibody-approved-in-Korea. Accessed 3 Jun 2021.
European Medicines Agency. Remicade summary of product characteristics. 2020. https://www.ema.europa.eu/en/documents/product-information/remicade-epar-product-information_en.pdf. Accessed 3 Jun 2021.
US Food and Drug Administration. Remicade prescribing information. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/103772s5389s5391s5394lbl.pdf. Accessed 3 Jun 2021.
Westhovens R, Wiland P, Zawadzki M, et al. Efficacy, pharmacokinetics and safety of subcutaneous versus intravenous CT-P13 in rheumatoid arthritis: a randomized phase I/III trial. Rheumatology (Oxford). 2021;60(5):2277–87.
Park W, Hrycaj P, Jeka S, et al. A randomised, double-blind, multicentre, parallel-group, prospective study comparing the pharmacokinetics, safety, and efficacy of CT-P13 and innovator infliximab in patients with ankylosing spondylitis: the PLANETAS study. Ann Rheum Dis. 2013;72(10):1605–12.
Yoo DH, Hrycaj P, Miranda P, et al. A randomised, double-blind, parallel-group study to demonstrate equivalence in efficacy and safety of CT-P13 compared with innovator infliximab when coadministered with methotrexate in patients with active rheumatoid arthritis: the PLANETRA study. Ann Rheum Dis. 2013;72(10):1613–20.
Odgaard-Jensen J, Vist GE, Timmer A, et al. Randomisation to protect against selection bias in healthcare trials. Cochrane Database Syst Rev. 2011;2011(4):MR000012.
Jones DS, Podolsky SH. The history and fate of the gold standard. Lancet. 2015;385(9977):1502–3.
Golder S, Loke YK, Bland M. Meta-analyses of adverse effects data derived from randomised controlled trials as compared to observational studies: methodological overview. PLoS Med. 2011;8(5):e1001026.
Ligthelm RJ, Borzi V, Gumprecht J, Kawamori R, Wenying Y, Valensi P. Importance of observational studies in clinical practice. Clin Ther. 2007;29 Spec No:1284–92.
Lee SJ, Baek K, Lee S, Lee YJ, Park JE, Lee SG. Post-marketing pooled safety analysis for CT-P13 treatment of patients with immune-mediated inflammatory diseases in observational cohort studies. BioDrugs. 2020;34(4):513–28.
Kay J, Schoels MM, Dörner T, et al. Consensus-based recommendations for the use of biosimilars to treat rheumatological diseases. Ann Rheum Dis. 2018;77(2):165–74.
European Medicines Agency. Remsima public assessment report. 2019. https://www.ema.europa.eu/en/documents/assessment-report/remsima-epar-public-assessment-report_en.pdf. Accessed 3 Jun 2021.
European Medicines Agency. Inflectra public assessment report. 2019. https://www.ema.europa.eu/en/documents/assessment-report/inflectra-epar-public-assessment-report_en.pdf. Accessed 3 Jun 2021.
Goll GL, Jørgensen KK, Sexton J, et al. Long-term efficacy and safety of biosimilar infliximab (CT-P13) after switching from originator infliximab: open-label extension of the NOR-SWITCH trial. J Intern Med. 2019;285(6):653–69.
Park W, Yoo DH, Miranda P, et al. Efficacy and safety of switching from reference infliximab to CT-P13 compared with maintenance of CT-P13 in ankylosing spondylitis: 102-week data from the PLANETAS extension study. Ann Rheum Dis. 2017;76(2):346–54.
Yoo DH, Prodanovic N, Jaworski J, et al. Efficacy and safety of CT-P13 (biosimilar infliximab) in patients with rheumatoid arthritis: comparison between switching from reference infliximab to CT-P13 and continuing CT-P13 in the PLANETRA extension study. Ann Rheum Dis. 2017;76(2):355–63.
Tanaka Y, Yamanaka H, Takeuchi T, et al. Safety and efficacy of CT-P13 in Japanese patients with rheumatoid arthritis in an extension phase or after switching from infliximab. Mod Rheumatol. 2017;27(2):237–45.
Nakagawa T, Kobayashi T, Nishikawa K, et al. Infliximab biosimilar CT-P13 is interchangeable with its originator for patients with inflammatory bowel disease in real world practice. Intest Res. 2019;17(4):504–15.
Fiorino G, Manetti N, Armuzzi A, et al. The PROSIT-BIO cohort: a prospective observational study of patients with inflammatory bowel disease treated with infliximab biosimilar. Inflamm Bowel Dis. 2017;23(2):233–43.
Choquette D, Faraawi R, Chow A, Rodrigues J, Bensen WJ, Nantel F. Incidence and management of infusion reactions to infliximab in a prospective real-world community registry. J Rheumatol. 2015;42(7):1105.
Thorne C, Bensen WG, Choquette D, et al. Effectiveness and safety of infliximab in rheumatoid arthritis: analysis from a Canadian multicenter prospective observational registry. Arthritis Care Res. 2014;66(8):1142–51.
Kim TH, Lee SS, Park W, et al. A 5-year retrospective analysis of drug survival, safety, and effectiveness of the infliximab biosimilar CT-P13 in patients with rheumatoid arthritis and ankylosing spondylitis. Clin Drug Investig. 2020;40(6):541–53.
Kim HA, Lee E, Lee SK, et al. Retention rate and long-term safety of biosimilar CT-P13 in patients with ankylosing spondylitis: data from the Korean College of Rheumatology Biologics registry. Clin Exp Rheumatol. 2020;38(2):267–74.
Kim HA, Lee E, Lee SK, et al. Retention rate and safety of biosimilar CT-P13 in rheumatoid arthritis: data from the Korean College of Rheumatology Biologics registry. BioDrugs. 2020;34(1):89–98.
Kurki P, van Aerts L, Wolff-Holz E, Giezen T, Skibeli V, Weise M. Interchangeability of biosimilars: a European perspective. BioDrugs. 2017;31(2):83–91.
Gonczi L, Gecse KB, Vegh Z, et al. Long-term efficacy, safety, and immunogenicity of biosimilar infliximab after one year in a prospective nationwide cohort. Inflamm Bowel Dis. 2017;23(11):1908–15.
Bálint A, Rutka M, Végh Z, et al. Frequency and characteristics of infusion reactions during biosimilar infliximab treatment in inflammatory bowel diseases: results from Central European nationwide cohort. Expert Opin Drug Saf. 2017;16(8):885–90.
Gecse KB, Lovász BD, Farkas K, et al. Efficacy and safety of the biosimilar infliximab CT-P13 treatment in inflammatory bowel diseases: a prospective, multicentre, nationwide cohort. J Crohns Colitis. 2016;10(2):133–40.
Acknowledgements
We thank all patients involved in the studies. Patients were not involved in the study design or dissemination of the results.
Funding
The studies reported in this article were funded by Celltrion, Inc. (Incheon, Republic of Korea). The journal’s Rapid Service Fee was also funded by Celltrion, Inc.
Medical Writing and Editorial Assistance
Medical writing support (including development of a draft outline and subsequent drafts in consultation with the authors, assembling tables and figures, collating author comments, copyediting, fact checking, and referencing) was provided by Beatrice Tyrrell, DPhil, at Aspire Scientific (Bollington, UK), and funded by Celltrion, Inc. (Incheon, Republic of Korea).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Jae Hee Cheon, Seongsu Nah, Hyoun Woo Kang, Yun Jeong Lim, Sang-Hoon Lee, and Sung-Hwan Park contributed to patient enrolment and monitoring, and data collection and analysis. Sang Joon Lee, Sung Hyun Kim, Na Hyun Jung, Jeong Eun Park, Yeo Jin Lee, Da Bee Jeon, Yeon Mi Lee, and Jong Min Kim contributed to trial design and data analysis.
Prior Presentation
Pooled interim safety results from the studies reported in the present article have been published previously (Lee SJ, et al. BioDrugs. 2020;34:513–28). An e-poster reporting final results from the CT-P13 4.3 registry study will be presented virtually on 3 July 2021 at the 16th Congress of the European Crohn’s and Colitis Organisation (ECCO).
Disclosures
Jae Hee Cheon reports personal fees and non-financial support from Celltrion, Inc. during the conduct of the study and personal fees from AbbVie Korea, Ferring Korea, IQVIA, Janssen Korea, Shire Korea, and Takeda Korea outside the submitted work. Seongsu Nah reports non-financial support from Celltrion, Inc. during the conduct of the study. Sang Joon Lee and Sung Hyun Kim are employees of, and hold shares in, Celltrion, Inc. Na Hyun Jung, Jeong Eun Park, Yeo Jin Lee, Da Bee Jeon, Yeon Mi Lee, and Jong Min Kim are employees of Celltrion, Inc. Hyoun Woo Kang, Yun Jeong Lim, Sang-Hoon Lee and Sung-Hwan Park report no conflicts of interest. The current affiliation for Hyoun Woo Kang is the Division of Gastroenterology and Hepatology, Department of Internal Medicine, SMG-SNU Boramae Medical Center, Seoul, Republic of Korea.
Compliance with Ethics Guidelines
The studies were conducted in accordance with the Helsinki Declaration of 1964 and its later amendments, the International Conference on Harmonisation, and relevant region/country-specific regulations. Study protocols were approved by the relevant institutional/regional review boards/ethics committees (see Supplementary Methods, Table S1). All participants provided written, informed consent.
Data Availability
Most of the data generated or analysed during this study are included in this published article (and the accompanying Supplementary Material). Other datasets associated with the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheon, J.H., Nah, S., Kang, H.W. et al. Infliximab Biosimilar CT-P13 Observational Studies for Rheumatoid Arthritis, Inflammatory Bowel Diseases, and Ankylosing Spondylitis: Pooled Analysis of Long-Term Safety and Effectiveness. Adv Ther 38, 4366–4387 (2021). https://doi.org/10.1007/s12325-021-01834-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01834-3