Abstract
Introduction
Patients with advanced cutaneous squamous cell carcinoma (CSCC) have a poor prognosis. Blocking the PD-1–PD-L1 axis has shown promising activity in this patient population. We assessed the safety and antitumor activity of PD-1 inhibitor pembrolizumab in patients with refractory advanced CSCC.
Methods
This was a prespecified subgroup analysis of patients with advanced CSCC who enrolled in an open-label, phase II clinical trial for pembrolizumab in patients with refractory rare cancers during 2016–2018. Patients received pembrolizumab 200 mg intravenously every 21 days until progressive disease, unacceptable adverse event, or completion of 24 months of treatment. The primary endpoint was nonprogression rate (NPR) at 27 weeks; secondary endpoints included safety, objective response rate (ORR) per irRECIST, clinical benefit rate (CBR), progression-free survival, and overall survival.
Results
Twenty patients with refractory CSCC enrolled; 19 were evaluable for efficacy. Median follow-up time was 44.1 months. The NPR at 27 weeks was 37% (95% CI 0.16–0.62). Three patients had a complete response (CR), three had a partial response, and one had stable disease, for an ORR of 32% and a CBR of 37%; median duration of response was 27.3 months. All three patients with a CR remained free of recurrence at the time of writing. Severe treatment-related adverse events (grade ≥ 3) occurred in 10% of patients (2/20). PD-L1 expression was not correlated with response to pembrolizumab.
Conclusion
A long-term follow-up confirms pembrolizumab’s antitumor activity and safety profile in patients with refractory CSCC. Patients with a CR may experience cure.
Trial Registration
ClinicalTrials.gov, NCT02721732, Registered March 29, 2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cutaneous squamous cell carcinoma (CSCC) is one of the most common cancers worldwide. Approximately, 5% of patients presents locally advanced or metastatic disease. |
Patients with advanced CSCC have a poor prognosis |
This phase II trial with long-term follow-up (median 44.1 months) confirms that pembrolizumab has a promising antitumor activity and is safe in patients with refractory CSCC. |
Patients who achieve a complete response to pembrolizumab may experience cure. |
Introduction
Cutaneous squamous cell carcinoma (CSCC) is one of the most common cancers worldwide. The head and neck harbor nearly 80% of cases [1, 2]. Fortunately, almost all patients with CSCC are diagnosed with early-stage CSCC and are cured with simple surgical procedures. However, approximately 5% of patients present with locally advanced or metastatic disease not amenable to local treatment; those patients require palliative systemic therapy [3].
Until 2018, chemotherapy and epidermal growth factor receptor (EGFR) inhibitors were the only systemic treatment options for patients with advanced CSCC. Platinum-based regimens were preferred because small prospective studies and retrospective series showed that such regimens produced responses in approximately 44% of patients [4], albeit of short duration and with significant toxicity [4,5,6]. In prospective studies, EGFR inhibitors were associated with an objective response rate (ORR) of 10–32% and were better tolerated than chemotherapy regimens, but duration of response to EGFR inhibitors was limited, and the 5-year survival rate after EGFR inhibitor treatment was less than 30% [7,8,9,10].
Because of the effects of chronic ultraviolet light exposure, CSCCs are hypermutated tumors with a complex molecular landscape [11, 12]. The risk of development of CSCC is 65–250 times as high in immunosuppressed patients as in the general population, indicating that the immune system plays a crucial role in CSCC prevention [13]. Both of these facts support the efficacy of PD-1 inhibitors against CSCC [14, 15].
In 2018, a phase I study of anti-PD-1 monoclonal antibody cemiplimab in locally advanced or metastatic CSCC showed safety and encouraging antitumor activity, which led to US Food and Drug Administration (FDA) approval of cemiplimab for CSCC treatment [16]. In 2020, anti-PD-1 monoclonal antibody pembrolizumab was also approved for CSCC treatment on the basis of interim results of a single-arm phase II trial, which demonstrated meaningful antitumor activity comparable to that of cemiplimab and adequate tolerability in patients with recurrent or metastatic CSCC [17]. Here, we report the efficacy and safety of pembrolizumab in patients with refractory CSCC with long-term follow-up and report the results of an exploratory biomarker analysis.
Methods
Study Design and Patients
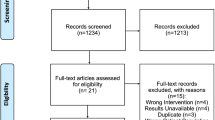
This was an open-label, single-arm, single-institution, investigator-initiated phase II basket trial of pembrolizumab in patients with rare cancers regardless of PD-L1 expression. The overall results were recently published [18]. In the analysis reported here, we focused on the prespecified CSCC cohort. Patients were enrolled from August 15, 2016 to July 27, 2018 (Fig. 1). Eligible patients were adults 18 years of age or older with histologically confirmed CSCC whose disease had progressed while on standard therapies within the previous 6 months. Additional inclusion criteria were an Eastern Cooperative Oncology Group (ECOG) performance status [19] of 0 or 1 and adequate organ function. Patients with active autoimmune disease, chronic immunosuppression, or previous treatment with anti-PD-1 or anti-PD-L1 therapy were excluded.
Patients had to have measurable disease per the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 [20] or immune-related RECIST (irRECIST) [21]. The irRECIST were developed to capture atypical response patterns from immunotherapy, such as pseudoprogression. The main difference between RECIST and irRECIST is that irRECIST takes into account new lesions and requires confirmation of progression to rule out or confirm pseudoprogression.
The protocol was approved by the US FDA and the Institutional Review Board at The University of Texas MD Anderson Cancer Center. The study was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice guidelines. All participants provided written informed consent before enrollment. The full protocol is available as supplementary material.
Study Schedule and Procedures
All patients received pembrolizumab 200 mg intravenously every 3 weeks until radiological or clinical evidence of progressive disease, unacceptable adverse event, patient withdrawal of consent, or completion of 24 months of pembrolizumab. Patients with a confirmed complete response could have pembrolizumab administration interrupted after receiving at least 27 weeks of treatment. No dose modifications were allowed, but dose delays for adverse events were permitted.
Imaging was performed at baseline, every 9 weeks for the first 6 months of treatment, and every 12 weeks thereafter at the physician’s discretion. Images were interpreted according to both irRECIST and RECIST. If baseline images showed progression, clinically stable patients were allowed to continue pembrolizumab for 4 weeks until confirmation of progression. Adverse events were graded according to the Common Terminology Criteria for Advent Events version 4.03 [22].
PD-L1 expression was assessed by immunohistochemistry at a central laboratory on formalin-fixed, paraffin-embedded tissue sections using the PD-L1 IHC 22C3 pharmDx assay (Agilent Technologies). A modified proportion score ranging from 0 to 100 was assigned, calculated as the proportion of PD-L1-positive mononuclear inflammatory cells plus the proportion of PD-L1-positive tumor cells within tumor nests.
On the basis of overall survival, recursive partitioning for classification and tree methods [23] were used to determine the optimal cutoff point for PD-L1 modified proportion score. The optimal cutoff point was a score of 57.5, i.e., 57.5 or greater indicated high PD-L1 expression. Tumor-infiltrating lymphocytes (TILs) within tumor nests were scored as 0 for absence of TILs, 1 for a few TILs, 2 for a moderate number of TILs, and 3 for intense intratumoral lymphocytic infiltration.
Planned Outcomes
The primary endpoint was nonprogression rate (NPR) at 27 weeks, defined as the proportion of patients alive and progression free at 27 weeks by irRECIST. This endpoint was chosen because it allowed observation of tumor behavior after three imaging cycles to permit proper estimation of the clinical activity and safety of pembrolizumab. Secondary endpoints were safety and tolerability of pembrolizumab, objective response rate (immune-related complete response [irCR] or immune-related partial response [irPR]), clinical benefit rate (irCR, irPR, or immune-related stable disease [irSD] ≥ 4 months), progression-free survival, and association of NPR at 27 weeks with PD-L1 status.
Statistical Analysis
Patient characteristics were summarized by descriptive statistics. The chi-square test or Fisher’s exact test was used to evaluate the association between two categorical variables. Wilcoxon rank-sum test was used to assess the difference in a continuous variable between patient groups. The Kaplan–Meier method was used for time-to-event analysis. The log-rank test was performed to assess the difference in time-to-event outcomes among different groups (PD-L1 expression high versus low). P values less than 0.05 were considered statistically significant. The analyses were performed using R version 3.6.3 (2020-02-29) and SAS 9.4.
Results
Patient Characteristics
Twenty patients with advanced CSCC were enrolled and received at least one dose of pembrolizumab. The data cutoff was November 10, 2020, and the median follow-up time was 44.1 months. Participants’ baseline characteristics and previous therapies are summarized in Table 1. The median age was 68 years; 19 patients had a baseline ECOG performance status of 1; 10 patients had head and neck primary disease site; and 10 patients had distant metastasis at enrollment.
In the curative setting, 11 patients had undergone two or more surgeries on the primary tumor, and 10 had received definitive (n = 3) or adjuvant (n = 7) radiotherapy. Two patients had received neoadjuvant chemotherapy before surgery with no response (Table 1).
Nineteen patients had received anticancer treatment for advanced disease before trial enrollment, including 13 who received systemic therapy. The two patients who received neoadjuvant chemotherapy before surgery as part of initial treatment were considered to have chemotherapy-refractory disease; therefore, they were not treated with further cytotoxic therapy upon recurrence. Eight patients (40%) received palliative radiotherapy (with or without concomitant chemotherapy), and 6 (30%) underwent palliative oncologic surgery. Baseline characteristics according to the best overall response are depicted in the supplementary material Table 1.
Efficacy
Nineteen patients had both baseline imaging and at least one on-treatment imaging study. One patient was lost to follow-up after one dose of pembrolizumab and excluded from the efficacy analysis.
The NPR at 27 weeks was 37% (7 of 19 patients; 95% CI 0.16–0.62). Nineteen patients were evaluable for radiologic response by irRECIST and included in the efficacy analysis, with 18 having measurable disease. The best overall response was CR in three patients (16%), PR in three patients (16%), SD in one patient (5%), and progressive disease in 12 patients (63%). Thus, the ORR was 32%, and the clinical benefit rate was 37% (95% CI 0.16–0.62) (Fig. 2a–c). Best overall response was similar for interpretation of images by irRECIST and interpretation of images by RECIST.
Response to treatment. a Waterfall plot shows dimensional change in target lesion as a percentage of baseline measurement using irRECIST. CR complete response, PR partial response, SD stable disease, PD progressive disease. b Representative PET-CT scans in a patient with a complete response. Left, baseline images show hypermetabolic enhancing soft tissue along the right platysma and thyroid lesion (arrows) representing biopsy-proven metastatic cutaneous squamous cell carcinoma. Right, scans after pembrolizumab show complete resolution of lesions (arrows). c Representative axial contrast-enhanced MRI scans in a patient with a complete response. Left, baseline scans show cordlike enhancing structures representing perineural tumor spread along the greater auricular, transverse cervical, and supraclavicular nerves (arrows). Right, scans after treatment show resolution of enhancement along the nerves (arrows). d Swimming plot shows the duration of response for each patient who achieved a partial or complete response (bars)
The median time to response was 2.04 months (range 2.00–4.14), and five of the six responders (83%) achieved at least a partial response at the first image assessment, although the median time to best overall response was 58 weeks (range 11–66). One patient experienced pseudoprogression, with target lesions enlarging and then shrinking. The median response duration was 27.37 months (95% CI 8.51–NA). Response duration exceeded 6 months in all six responders and exceeded 12 months in five responders (83%) (Fig. 2d). The 12- and 24-month disease control rates were 71% and 57%, respectively.
The median number of pembrolizumab cycles was 5 (interquartile range 2.75–8.75) for the entire population and 33 (range 3–35) among responders. Of the seven patients with clinical benefit, two completed 35 cycles and one completed 32 cycles of treatment; all three patients remain under surveillance with no evidence of disease progression at this writing (at 43.7, 41, and 39.6 months, respectively, after initiation of pembrolizumab).
At the data cutoff, 13 patients had died or experienced disease progression, three were lost to follow-up, and four were alive without disease progression at last follow-up. The median progression-free survival was 2.04 months (95% CI 1.84–29.37), and the progression-free survival rates at 12 and 24 months were 26% and 21%, respectively. The median overall survival was 8.31 months (95% CI 5.81–NA), and the overall survival rates at 12 and 24 months were 49% and 43%, respectively (Fig. 3).
Biomarker Analysis
Sixteen patients had biomarker assessment. The mean modified proportion score was 62.1 overall, 71.8 in patients progression free at 27 weeks, and 54.4 in patients with progressive disease at 27 weeks. Ten patients had high PD-L1 expression and six had low PD-L1 expression. Five patients (50%) with high PD-L1 expression versus two (33%) with low PD-L1 expression were alive and progression free at 27 weeks. The ORR and NPR at 27 weeks were also numerically higher among patients with high PD-L1 expression, but the differences were not statistically significant (Supplementary Fig. 1).
Interestingly, all analyzed samples had at least a few TILs. TIL score was not associated with NPR at 27 weeks or with other efficacy outcomes.
Safety
All 20 patients were evaluable for safety and toxicity. Twelve patients (60%) experienced a treatment-related adverse event (TRAE) (Table 2). The most common TRAEs were maculopapular rash (30%), fatigue (20%), and hypothyroidism (20%). Most TRAEs were mild to moderate. The two grade 3 TRAEs were arthralgia in a patient previously diagnosed with rheumatoid arthritis and immune-related pancerebellar dysfunction in a 68-year-old man with no history of neurologic disease. In both cases, pembrolizumab was discontinued, and the patient recovered fully. There were no treatment-related deaths.
Discussion
Here, we present the outcomes of 20 patients with refractory locoregionally advanced or metastatic CSCC treated with pembrolizumab in a phase II, single-arm study [18] with long-term follow-up. The primary endpoint of NPR at 27 weeks was 37% (95% CI 0.16–0.62).
Pembrolizumab led to an ORR of 32% and a clinical benefit rate of 37% in patients with highly refractory advanced CSCC. Among responders to pembrolizumab, responses were rapid: the median time to response was 9 weeks, and 83% of responders achieved at least a partial response at the first image assessment. Responses were durable: the median duration was 27.3 months, and more than half of responders had disease control at 24 months. Moreover, the three patients with a complete response remained free of evidence of recurrence at the time of writing.
The ORR in our study, 32%, is smaller than ORRs in other phase II studies investigating anti-PD-1 in CSCC. However, our study was limited to patients with progression on standard therapies within the previous 6 months, which selected for the most refractory cases. Consistent with that assertion, at study enrollment, 50% of the patients had distant metastasis, 95% had symptoms (ECOG performance status of 1), and 95% had previously received systemic or radiation treatment for advanced disease, with 75% having chemotherapy-refractory disease (including the two patients with no response to induction chemotherapy).
In the phase II study of cemiplimab, the ORR was 46%; however, almost half of the patients (45%) were asymptomatic (ECOG 0) at study enrollment, and 66% were treatment-naïve [24]. Similarly, in the CARSkin trial, the ORR with pembrolizumab was 38.5%, but pembrolizumab was used as first-line treatment of CSCC [25]. In contrast, in the phase II Keynote-629 trial, in which pembrolizumab was investigated in patients similar to ours, with refractory recurrent/metastatic disease (87% previously treated with systemic therapy), the ORR was 34.3% [17], consistent with our results. These data suggest that PD-1 inhibitors might yield a better response rate in treatment-naïve than in previously treated patients, although the drugs can be effective in heavily pretreated patients as well.
To our knowledge, of the clinical trials of checkpoint inhibitor in patients with CSCC, the one we report here has the longest follow-up and most mature survival outcomes. The median overall survival of 8.31 months in this heavily pretreated patient population is encouraging, and it is noteworthy that three patients (15%) who achieved a complete response remained without evidence of disease more than 18 months after treatment completion.
Biomarker analysis showed a tendency of better outcomes among patients with high PD-L1 expression, although this difference was not statistically significant, possibly because of the small sample size. However, given that there are no established effective treatment options for refractory or metastatic CSCC and 30% of patients whose tumors had low PD-L1 expression benefited from pembrolizumab, this agent should be considered for all patients irrespective of PD-L1 status. Our biomarker data are in line with reports from the phase II studies with pembrolizumab or cemiplimab in CSCC showing treatment benefit regardless of PD-L1 expression or median tumor mutation burden [17, 24]
Study limitations include the small number of patients, single-center design, and non-randomized design. Nevertheless, the results are in agreement with the recently published phase II trials evaluating anti-PD-1 in patients with CSCC and further support pembrolizumab and cemiplimab as standard for patients with locoregionally advanced inoperable recurrent or metastatic CSCC. One major strength of our study is the long-term follow-up with mature outcomes data, which suggest that patients with a complete response may be cured with single-agent anti-PD-1.
Challenges remain with respect to PD-1-refractory or chronically immunosuppressed patients (e.g., solid organ transplant recipients), to whom immunotherapy can bring unacceptable harm [26]. Further studies to refine predictive biomarkers for PD-1 inhibitors and clinical trials evaluating drug combinations to overcome innate and acquired resistance to PD-1 blockage are under consideration.
Conclusions
Our study confirms clinically meaningful antitumor activity and an acceptable safety profile for pembrolizumab in patients with recurrent or metastatic refractory CSCC. Prolonged responses in patients with a complete response raise the possibility of cure for a subset of patients.
References
Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the US population, 2012. JAMA Dermatol. 2015;151(10):1081–6.
Karia PS, Han J, Schmults CD. Cutaneous squamous cell carcinoma: estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012. J Am Acad Dermatol. 2013;68(6):957–66.
Clayman GL, Lee JJ, Holsinger CF, et al. Mortality risk from squamous cell skin cancer. J Clin Oncol. 2005;23(4):759–65.
Jarkowski A 3rd, Hare R, Loud P, et al. Systemic therapy in advanced cutaneous squamous cell carcinoma (CSCC): the Roswell park experience and a review of the literature. Am J Clin Oncol. 2016;39(6):545–8.
Shin DM, Glisson BS, Khuri FR, et al. Phase II and biologic study of interferon alfa, retinoic acid, and cisplatin in advanced squamous skin cancer. J Clin Oncol. 2002;20(2):364–70.
Sadek H, Azli N, Wendling JL, et al. Treatment of advanced squamous cell carcinoma of the skin with cisplatin, 5-fluorouracil, and bleomycin. Cancer. 1990;66(8):1692–6.
William WN Jr, Feng L, Ferrarotto R, et al. Gefitinib for patients with incurable cutaneous squamous cell carcinoma: a single-arm phase II clinical trial. J Am Acad Dermatol. 2017;77(6):1110 e2-1113 e2.
Gold KA, Kies MS, William WN Jr, Johnson FM, Lee JJ, Glisson BS. Erlotinib in the treatment of recurrent or metastatic cutaneous squamous cell carcinoma: a single-arm phase 2 clinical trial. Cancer. 2018;124(10):2169–73.
Foote MC, McGrath M, Guminski A, et al. Phase II study of single-agent panitumumab in patients with incurable cutaneous squamous cell carcinoma. Ann Oncol. 2014;25(10):2047–52.
Maubec E, Petrow P, Scheer-Senyarich I, et al. Phase II study of cetuximab as first-line single-drug therapy in patients with unresectable squamous cell carcinoma of the skin. J Clin Oncol. 2011;29(25):3419–26.
Chalmers ZR, Connelly CF, Fabrizio D, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017;9(1):34.
Pickering CR, Zhou JH, Lee JJ, et al. Mutational landscape of aggressive cutaneous squamous cell carcinoma. Clin Cancer Res. 2014;20(24):6582–92.
Euvrard S, Kanitakis J, Claudy A. Skin cancers after organ transplantation. N Engl J Med. 2003;348(17):1681–91.
Yarchoan M, Hopkins A, Jaffee EM. Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med. 2017;377(25):2500–1.
Yarchoan M, Albacker LA, Hopkins AC, et al. PD-L1 expression and tumor mutational burden are independent biomarkers in most cancers. JCI Insight. 2019. https://doi.org/10.1172/jci.insight.126908.
Migden MR, Rischin D, Schmults CD, et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N Engl J Med. 2018;379(4):341–51.
Grob JJ, Gonzalez R, Basset-Seguin N, et al. Pembrolizumab monotherapy for recurrent or metastatic cutaneous squamous cell carcinoma: a single-arm phase II trial (KEYNOTE-629). J Clin Oncol. 2020;38(25):2916–25.
Naing A, Meric-Bernstam F, Stephen B, et al. Phase 2 study of pembrolizumab in patients with advanced rare cancers. J Immunother Cancer. 2020;8(1):e000347corr1.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Nishino M, Tirumani SH, Ramaiya NH, Hodi FS. Cancer immunotherapy and immune-related response assessment: the role of radiologists in the new arena of cancer treatment. Eur J Radiol. 2015;84(7):1259–68.
US Department of Health and Human Services. Common terminology criteria for adverse events v4.03 (CTCAE). 2010.
Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees (Wadsworth statistics/probability). Boca Raton: Chapman and Hall/CRC; 1984.
Rischin D, Khushalani NI, Schmults CD, et al. Phase II study of cemiplimab in patients (pts) with advanced cutaneous squamous cell carcinoma (CSCC): longer follow-up. J Clin Oncol. 2020;38(15_suppl):10018–10018.
Maubec E, Boubaya M, Petrow P, et al. Pembrolizumab as first line therapy in patients with unresectable squamous cell carcinoma of the skin: interim results of the phase 2 CARSKIN trial. J Clin Oncol. 2018;36(15_suppl):9534–9534.
Abdel-Wahab N, Safa H, Abudayyeh A, et al. Checkpoint inhibitor therapy for cancer in solid organ transplantation recipients: an institutional experience and a systematic review of the literature. J Immunother Cancer. 2019;7(1):106.
Acknowledgements
We thank Stephanie Deming, scientific editor, Research Medical Library, for editing this article
Funding
Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., provided the study drug and funded the study. Support was also provided by the National Institutes of Health/National Cancer Institute under award number P30CA016672 (used the Biostatistics Resource Group) and The University of Texas MD Anderson Cancer Center through the Molecular Evaluation and/or Biopsy Related Support Program (used for performing biopsy in selected patient cohorts). The Journal’s Rapid Service Fee was funded by the authors.
Disclosures
Dr. Ferrarotto reports personal fees from Regeneron-Sanofi, Ayala Pharmaceuticals, Prelude Pharmaceuticals, Bicara Therapeutics, Klus Pharma, Medscape, and Carevive and institutional fees from AstraZeneca, Merck, Genentech, Pfizer, EMD-Serono, Ayala Pharmaceuticals, Prelude Pharmaceuticals, and Rakuten Medical not related to the topic of the submitted work. Dr. Piha-Paul reports receiving the following research/grant funding from: AbbVie, Inc.; ABM Therapeutics, Inc.; Acepodia, Inc; Alkermes; Aminex Therapeutics; Amphivena Therapeutics, Inc.; BioMarin Pharmaceutical, Inc; Boehringer Ingelheim; Bristol Myers Squib; Cerulean Pharma, Inc.; Chugai Pharmaceutical Co., Ltd; Curis, Inc.; Daiichi Sankyo; Eli Lilly; ENB Therapeutics; Five Prime Therapeutics; Gene Quantum; Genmab A/S; GlaxoSmithKline; Helix BioPharma Corp.; Incyte Corp.; Jacobio Pharmaceuticals Co., Ltd.; Medimmune, LLC.; Medivation, Inc.; Merck Sharp and Dohme Corp.; Novartis Pharmaceuticals; Pieris Pharmaceuticals, Inc.; Pfizer; Principia Biopharma, Inc.; Puma Biotechnology, Inc.; Rapt Therapeutics, Inc.; Seattle Genetics; Silverback Therapeutics; Taiho Oncology; Tesaro, Inc.; and TransThera Bio.
Authors’ Contributions
Renata Ferrarotto contributed to enrollment of patients, data analysis, data interpretation, and writing the manuscript; Luana Sousa contributed to literature search, data analysis, data interpretation, and writing the manuscript; Yun Qing and J. Jack Lee contributed to analysis and interpretation of data; Diana Kaya reviewed the radiographic data and performed the quantitative imaging analysis; Bettzy Stephen contributed to literature search, data collection, data analysis, and data interpretation; Shubham Pant, Apostolia M. Tsimberidou, Filip Janku, Jordi Rodon Ahnert, Sapina A. Piha-Paul, and Dipti Jain contributed to acquisition and interpretation of data; Charles Lu, Michael Wong, George Blumenschein, and Bonnie Glisson contributed to enrollment of patients and acquisition and interpretation of data; Diana Bell contributed to pathological analysis and interpretation; Funda Meric-Bernstam contributed to study design, data interpretation, and writing; Aung Naing contributed to study design, conduct of the study, enrollment of patients, data and biospecimen collection, data analysis, data interpretation, and writing of the manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Compliance with Ethics Guidelines
The protocol was approved by the FDA and the Institutional Review Board at The University of Texas MD Anderson Cancer Center. The study was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice guidelines. All the study participants provided written informed consent before enrollment.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request and approval from study sponsor according to available guidelines at time of request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ferrarotto, R., Sousa, L.G., Qing, Y. et al. Pembrolizumab in Patients with Refractory Cutaneous Squamous Cell Carcinoma: A Phase II Trial. Adv Ther 38, 4581–4591 (2021). https://doi.org/10.1007/s12325-021-01807-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01807-6