Abstract
Introduction
Splenectomy and splenic artery embolization are major treatment options for hypersplenism and portal hypertension in liver cirrhosis, but may lead to splanchnic vein thrombosis (SVT), which is potentially lethal. We conducted a systematic review and meta-analysis to explore the incidence of SVT in liver cirrhosis after splenectomy or splenic artery embolization and the risk factors for SVT.
Methods
All relevant studies were searched through the PubMed, EMBASE, and Cochrane Library databases. The incidence of SVT in liver cirrhosis after splenectomy or splenic artery embolization was pooled. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated.
Results
Sixty-six studies with 5632 patients with cirrhosis were included. The pooled incidence of SVT after splenectomy and splenic artery embolization was 24.6% (95% CI 20.2–29.3%) and 11.7% (95% CI 7.1–17.3%), respectively. A meta-analysis of three comparative studies demonstrated that the incidence of SVT after splenectomy was statistically similar to that after splenic artery embolization (OR 3.15, P = 0.290). Platelet count, mean platelet volume, preoperative splenic or portal vein diameter, preoperative or postoperative portal blood velocity, splenic volume and weight, and periesophagogastric devascularization were significant risk factors for SVT after splenectomy. Postoperative use of preventive antithrombotic therapy was a significant protective factor against SVT after splenectomy.
Conclusions
SVT is common in liver cirrhosis after splenectomy and splenic artery embolization. Coagulation and hemostasis factors, anatomical factors, and surgery-related factors have been widely identified for the assessment of high risk of SVT after splenectomy. Prophylactic strategy after splenectomy, such as antithrombotic therapy, might be considered in such high-risk patients.
Study Registration
This study was registered in PROSPERO with a registration number of CRD42019129673.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Why carry out this study? |
Splenectomy and splenic artery embolization are the treatment options for portal hypertension and hypersplenism in liver cirrhosis, but may lead to splanchnic vein thrombosis (SVT). The management of SVT after splenectomy or splenic artery embolization is often challenging. |
What was learned from the study? |
SVT was common in patients who underwent splenectomy and splenic artery embolization. The risk of SVT after splenectomy was similar to that after splenic artery embolization (OR 3.15, 95% CI 0.38–25.91; P = 0.290). |
Platelet count, mean platelet volume, preoperative splenic or portal vein diameter, preoperative or postoperative portal blood velocity, splenic volume and weight, and periesophagogastric devascularization are associated with development of SVT after splenectomy. |
Early imaging screening and prophylactic strategy might be beneficial in patients at high risk for SVT. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13693651.
Introduction
Liver cirrhosis, which is the end stage of chronic liver disease, often has complications associated with portal hypertension and/or hypersplenism [1]. In China and Japan, splenectomy and splenic artery embolization are the mainstay treatment options for portal hypertension and hypersplenism in patients with liver cirrhosis [2,3,4]. Splenectomy with devascularization can increase hepatopetal blood flow into the portal venous system, eliminate splenomegaly and/or hypersplenism, and control variceal bleeding [5]. Splenic artery embolization, which can preserve a portion of the spleen, is an alternative, if a patient has any contraindication for splenectomy [6]. However, both splenectomy and splenic artery embolization can lead to splanchnic vein thrombosis (SVT), which is life-threatening [7,8,9]. Until now, the epidemiology of and risk factors for SVT after the two procedures remain inconsistent among studies. Herein, we performed a systematic review and meta-analysis with two major objectives: (1) to explore the incidence of SVT in liver cirrhosis after splenectomy or splenic artery embolization and the risk factors for SVT after splenectomy; and (2) to compare the incidence of SVT in liver cirrhosis after splenectomy versus splenic artery embolization.
Methods
This is a meta-analysis based on previously published studies and does not involve any new studies of human or animal subjects performed by any of the authors. The work is conducted according to MOOSE and PRISMA. The MOOSE and PRISMA checklists are shown in the supplementary material.
Registration
This study was registered in PROSPERO with a registration number of CRD42019129673.
Search Strategy
All published literature regarding SVT after splenectomy or splenic artery embolization was retrieved through the PubMed, EMBASE, and Cochrane Library databases. Search items are listed in the supplementary material. We conducted the last search on March 24, 2019.
Study Selection
Inclusion criteria were as follows: (1) patients should undergo splenectomy or splenic artery embolization for hypersplenism secondary to liver cirrhosis and/or portal hypertension; (2) patients should be over 18 years old; (3) eligible studies should report the incidence and/or risk factors for SVT in liver cirrhosis after splenectomy or splenic artery embolization; and (4) there was no language limitation.
Exclusion criteria were as follows: (1) duplicates; (2) case reports, reviews or meta-analyses, guidelines, consensus or reports, experimental or animal studies, comments or letters, notes, and irrelevant papers; (3) patients were diagnosed with SVT before splenectomy or splenic artery embolization; (4) no detailed data regarding incidence of SVT after splenectomy or splenic artery embolization could be extracted; and (5) full text cannot be obtained.
Definitions
SVT is defined as thrombosis occurring in the portal vein system, including portal, splenic, and mesenteric veins. A cohort study is defined as one in which the follow-up outcomes of patients with cirrhosis undergoing splenectomy or splenic artery embolization are observed to explore the causal relationship of SVT with splenectomy or splenic artery embolization. A case–control study is defined as one in which a group of patients with cirrhosis and SVT is selected as the case group, and another group of patients with cirrhosis but without SVT as a control group; and then splenectomy or splenic artery embolization as an exposure is compared between case and control groups to explore the association of SVT with splenectomy or splenic artery embolization.
Data Extraction
The following data were collected: the first author, publication year, region, enrollment period, study design, type of publication, patients’ characteristics, type of splenectomy, incidence and diagnostic approaches of SVT, timing of SVT detection, preventive antithrombotic therapy after splenectomy or splenic artery embolization, splenic infarction rate, timing of calculation of splenic infarction rate after splenic artery embolization, and number of patients who underwent and did not undergo pericardial devascularization.
Study Quality
Cohort or case–control studies were evaluated by the Newcastle–Ottawa scale (NOS), in which 0–3, 4–6, and 7–9 stars represent low, moderate, and high quality, respectively. Randomized controlled trials (RCTs) were evaluated by the Cochrane risk of bias tool. Bias risk assessment levels include low risk, high risk, and uncertainty.
Statistical Analysis
All meta-analyses were conducted by using StatsDirect statistical software version 2.8.0 (StatsDirect Ltd, Sale, Cheshire, UK), STATA version 12.0 (Stata Corp, College Station, Texas, USA), and Review Manager software version 5.3 (Cochrane collaboration, the Nordic Cochrane Centre, Copenhagen, Denmark). First, we pooled the incidence of SVT after splenectomy or splenic artery embolization in all studies, and compared the incidence of SVT in liver cirrhosis after splenectomy versus splenic artery embolization. Second, we collected the risk factors for SVT in patients with cirrhosis who underwent splenectomy, and then odds ratios (ORs) or mean difference (MD) with 95% confidence intervals (CIs) were calculated, if any. Only a random-effect model was performed. I2 statistics and Cochran’s Q test were used to assess the heterogeneity among studies, and I2 > 50% and/or P < 0.1 was considered to have statistically significant heterogeneity. Publication bias was performed with Egger’s test. P < 0.1 was considered as a statistically significant publication bias. Subgroup and meta-regression analyses were performed to explore the sources of heterogeneity. In the subgroup analyses, country (China versus Japan versus Egypt), region (Europe versus Oceania versus Africa versus Asia), publication year (before 2010 versus after 2010), design (cohort versus case–control versus RCT), type of splenectomy (open versus laparoscopic), diagnostic approaches of SVT [ultrasound versus computed tomography (CT) or magnetic resonance imaging (MRI) versus computed tomography angiography (CTA) or digital substraction angiography (DSA)], timing of SVT detection after surgery (within 7 days and > 7 days), pericardial devascularization (yes versus no), preventive antithrombotic therapy (yes versus no), and splenic infarction rate (≥ 50% versus < 50%) were used as covariates. Meta-regression analyses were performed in terms of country (China versus Japan versus Egypt), region (Europe versus Oceania versus Africa versus Asia), publication year (before 2010 versus after 2010), study design (cohort versus case–control versus RCT), sample size (≥ 100 versus < 100), and NOS (≥ 7 versus < 7). Sensitivity analyses were conducted to assess the stability of the results by sequentially excluding one study in one turn.
Results
Study Selection and Study Characteristics
We initially identified 766 studies through the three databases and one study by reviewing the reference list. Finally, 66 studies were included (Fig. 1) [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75], including splenectomy alone [10,11,12,13,14, 16,17,18,19, 21, 22, 24, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41, 43,44,45,46, 48, 49, 51,52,53,54,55, 57,58,59,60, 62, 64, 67,68,69, 72,73,74] (n = 51), splenic artery embolization alone [15, 20, 25, 47, 50, 56, 61, 63, 65, 70, 71, 75] (n = 12), and both [23, 42, 66] (n = 3). They were published in the form of full text [10,11,12,13,14,15, 17, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36, 38,39,40,41, 44,45,46,47,48,49, 51,52,53,54, 56,57,58,59,60,61,62, 64,65,66,67,68,69,70,71,72,73,74,75] (n = 58) or abstract [16, 18, 37, 42, 43, 50, 55, 63] (n = 8) between 1979 and 2019; 39 were cohort studies [11, 13, 16, 18, 19, 21, 25,26,27, 29, 30, 32,33,34,35, 37, 39,40,41,42,43, 46,47,48, 50,51,52, 55, 56, 60, 61, 63, 64, 67, 70,71,72, 74, 75], 20 were case–control studies [12, 14, 17, 22,23,24, 28, 31, 36, 38, 44, 45, 49, 54, 57,58,59, 62, 65, 68], and 7 were RCTs [10, 15, 20, 53, 66, 69, 73]; 57 were performed in Asia [10,11,12,13,14, 17,18,19, 21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55, 57,58,59,60,61,62, 64, 65, 67,68,69, 72,73,74], 5 in Africa [15, 16, 20, 56, 66], 3 in Europe [70, 71, 75], and 1 in Oceania [63]. They included 5632 patients with cirrhosis, of whom 1275 developed SVT. The information of the 66 included studies regarding splenectomy and splenic artery embolization was shown in Tables 1 and 2, respectively.
Study Quality
Among the cohort or case–control studies, 32 and 27 studies were of high [11, 12, 17, 19, 22,23,24, 26, 28, 30,31,32,33, 35, 36, 38, 40, 42, 44, 45, 47,48,49, 51, 54, 57,58,59, 61, 64, 65, 68] and moderate quality [13, 14, 16, 18, 21, 25, 27, 29, 34, 37, 39, 41, 43, 46, 50, 52, 55, 56, 60, 62, 63, 67, 70,71,72, 74, 75], respectively (Supplementary Table 1). Among the RCTs, the attrition bias was at high risk in one study, and other biases were at low or unclear risk in all studies (Supplementary Figs. 1, 2).
Incidence of Splanchnic Vein Thrombosis in Liver Cirrhosis after Splenectomy and Splenic Artery Embolization
Overall and Subgroup Analyses
Fifty-four studies explored the incidence of SVT after splenectomy in patients with liver cirrhosis, and the pooled incidence of SVT was 24.6% (95% CI 20.2–29.3%) (Table 3). The pooled incidence of SVT after splenectomy was 24.5%, 25.7%, and 21.0% in China, Japan, and Egypt, respectively; 18.4% and 26.7% in studies published before 2010 and after 2010, respectively; 18.2%, 36.3%, and 22.4% in cohort studies, case–control studies, and RCTs, respectively; 25.5% and 30.2% after open splenectomy (OS) and laparoscopic splenectomy (LS), respectively; 28.0%, 26.5%, and 28.7% based on ultrasound, CT/MRI, and CTA, respectively; 27.4% and 20.3% in studies evaluating SVT within 7 days and > 7 days after surgery, respectively; 27.2% and 21.6% in patients with and without pericardial devascularization, respectively; and 32.2% and 23.1% in patients with and without preventive antithrombotic therapy, respectively.
Fifteen studies explored the incidence of SVT after splenic artery embolization in patients with liver cirrhosis, and the pooled incidence of SVT was 11.7% (95% CI 7.1–17.3%) (Table 4). The pooled incidence of SVT after splenic artery embolization was 22.6%, 16.7%, 10.7%, and 9.7% in Europe, Oceania, Africa, and Asia, respectively; 18.4% and 8.0% in studies published before 2010 and after 2010, respectively; 10.1%, 21.4%, and 12.1% in cohort studies, case–control studies, and RCTs, respectively; 7.2%, 18.5%, and 10.0% based on ultrasound, CT/MRI, and DSA, respectively; 32.1% and 7.4% in studies evaluating SVT within 7 days and > 7 days after surgery, respectively; 13.0% and 9.3% in patients with a splenic infarction rate of ≥ 50% and < 50%, respectively.
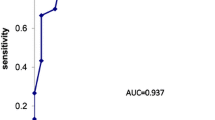
Three studies compared the incidence of SVT after splenectomy versus splenic artery embolization in patients with liver cirrhosis. Meta-analysis indicated that the incidence of SVT was not significantly different between the two groups (OR 3.15, 95% CI 0.38–25.91; P = 0.29) (Fig. 2).
Meta-Regression Analyses
Meta-regression analyses indicated that study design (P = 0.007), rather than publication year (P = 0.131), sample size (P = 0.368), region (P = 0.875), and NOS score (P = 0.207), could explain the potential source of heterogeneity (Supplementary Table 2).
Meta-regression analyses indicated that publication year (P = 0.232), sample size (P = 0.824), study design (P = 0.895), region (P = 0.783), and NOS score (P = 0.461) were not the source of heterogeneity (Supplementary Table 3).
Sensitivity Analyses
Sensitivity analyses were performed in all included studies, but the source of heterogeneity was not found.
Risk Factors for Splanchnic Vein Thrombosis in Liver Cirrhosis After Splenectomy
Systematic Review
Twenty-four studies reported the risk factors for SVT after splenectomy in liver cirrhosis. Fifteen studies explored the risk factors for SVT by univariate analysis (Supplementary Table 4); the most common risk factors were preoperative platelet count (seven studies) and preoperative portal vein diameter (seven studies), followed by preoperative splenic vein diameter (six studies), postoperative platelet count (four studies), and postoperative d-dimer level (four studies). Twenty-four studies explored the risk factors for SVT by multivariate analysis (Supplementary Table 5); the most common risk factor was preoperative portal vein diameter (seven studies), followed by preoperative splenic vein diameter (six studies), postoperative D-dimer level (six studies), and splenic volume and weight (four studies).
Meta-Analyses
Age
Eleven studies provided detailed data regarding the association of age with SVT. Meta-analysis indicated that age was not significantly associated with SVT (MD 0.81, 95% CI − 1.73 to 3.36; P = 0.53).
Preoperative Platelet Count
Nine studies provided detailed data regarding the association of preoperative platelet count with SVT. Meta-analysis indicated that lower preoperative platelet count was a significant risk factor for SVT (MD − 5.96, 95% CI − 10.64 to − 1.28; P = 0.01).
Postoperative Platelet Count
Three studies provided detailed data regarding the association of postoperative platelet count with SVT. Meta-analysis indicated that higher postoperative platelet count was a significant risk factor for SVT (MD 79.52, 95% CI 60.82–98.23; P < 0.00001).
Mean Platelet Volume
Two studies provided detailed data regarding the association of mean platelet volume with SVT. Meta-analysis indicated that larger mean platelet volume was a significant risk factor for SVT (MD 1.62, 95% CI 1.05–2.19; P < 0.00001).
P-selectin
Two studies provided detailed data regarding the association of P-selectin with SVT. Meta-analysis indicated that P-selectin was not significantly associated with SVT (MD 27.20, 95% CI − 2.92 to 57.33; P = 0.08).
Postoperative d-dimer Level
Five studies provided detailed data regarding the association of postoperative d-dimer level with SVT. Meta-analysis indicated that higher postoperative d-dimer level was a significant risk factor for SVT (MD 8.90, 95% CI 2.91–14.88; P = 0.004).
Preoperative Splenic Vein Diameter
Five studies provided detailed data regarding the association of preoperative splenic vein diameter with SVT. Meta-analysis indicated that wider preoperative splenic vein diameter was a significant risk factor for SVT (MD 2.01, 95% CI 0.83–3.19; P = 0.0008).
Preoperative Portal Vein Diameter
Four studies provided detailed data regarding the association of preoperative portal vein diameter with SVT. Meta-analysis indicated that wider preoperative portal vein diameter was a significant risk factor for SVT (MD 1.87, 95% CI 1.47–2.28; P < 0.00001).
Preoperative Portal Blood Flow Velocity
Four studies provided detailed data regarding the association of preoperative portal blood flow velocity with SVT. Meta-analysis indicated that decreased of preoperative portal blood flow velocity was a significant risk factor for SVT (MD − 8.80, 95% CI − 14.72 to − 2.88; P = 0.004).
Postoperative Portal Blood Flow Velocity
Two studies provided detailed data regarding the association of postoperative portal blood velocity with SVT. Meta-analysis indicated that decreased postoperative portal blood velocity was a significant risk factor for SVT (MD − 10.35, 95% CI − 15.39 to − 5.30; P < 0.0001).
Splenic Volume
Three studies provided detailed data regarding the association of splenic volume with SVT. Meta-analysis indicated that larger splenic volume was a significant risk factor for SVT (MD 216.40, 95% CI 80.35–352.45; P = 0.002).
Splenic Weight
Five studies provided detailed data regarding the association of splenic weight with SVT. Meta-analysis indicated that larger splenic weight was a significant risk factor for SVT (MD 202.22, 95% CI 31.83–372.61; P = 0.02).
Pericardial Devascularization
Four studies provided detailed data regarding the association of pericardial devascularization with SVT. Meta-analysis indicated that pericardial devascularization was a significant risk factor for SVT (OR 2.81, 95% CI 1.74–4.53; P < 0.0001).
Preventive Antithrombotic Therapy
Four studies provided detailed data regarding the association of preventive antithrombotic therapy with SVT. Among them, some patients received prophylactic antiplatelet therapy in two studies, including aspirin or dipyridamole; some patients received prophylactic antithrombotic therapy in one study, including low molecular weight heparin, warfarin, and aspirin; and some patients received prophylactic anticoagulation in one study, but anticoagulant drugs were unspecified. Meta-analysis indicated that postoperative use of preventive antithrombotic therapy was a significant protective factor against SVT (OR 0.40, 95% CI 0.17–0.91; P = 0.03).
Discussion
Our proportion meta-analysis demonstrated that the pooled incidence of SVT seemed to be absolutely higher in patients who underwent splenectomy than those who underwent splenic artery embolization (24.6% versus 11.7%). However, our meta-analysis of three comparative studies evaluating splenectomy versus splenic artery embolization in liver cirrhosis demonstrated that the risk of SVT after splenectomy was not significantly different from that after splenic artery embolization. This seemingly contradictory phenomenon can be explained by the fact that the characteristics of patients included in the three studies were well comparable between the two groups. In details, in the RCT by Amin et al. [66], white blood cells count, hemoglobin, serum creatinine, alanine aminotransferase, aspartate aminotransferase, serum albumin, serum bilirubin, prothrombin concentration, and international normalized ratio were statistically similar between the two groups; in the case–control study by Jiao et al. [23], age, gender, serum HBV DNA level, antiviral therapy, spleen weight, grade of esophageal varices, Child–Pugh class, indocyanine green retention value at 15 min, comorbidity rate, and ASA grade were statistically similar between the two groups; in the study by Wu et al. [42], age, gender, and Child–Pugh class were statistically similar between the two groups. More importantly, we have also identified the risk factors for SVT after splenectomy, including coagulation and hemostasis factors, anatomical factors, and surgery-related factors, which may be useful to enable the risk stratification and improve patient management.
Our subgroup analysis demonstrated that the incidence of SVT after splenectomy was the highest based on CTA, followed by ultrasound and CT/MRI. CTA is a gold standard for the detection of thrombosis, but it is so invasive and expensive that it is not considered as the first-line choice of detection [76]. Ultrasound is a non-invasive and inexpensive approach for diagnosis of thrombosis with good compliance. The sensitivity and specificity of ultrasound in the diagnosis of SVT were 89–93% and 92–99%, respectively [77]. Ultrasound can be valuable for screening early asymptomatic SVT to improve the detection rate of thrombosis as compared to CT/MRI scans. However, the results of ultrasound are often limited by the operator’s experience and the patient’s disease conditions (i.e., obesity, ascites, and bowel gas) [77, 78]. In addition, it is still a clinical challenge to distinguish SVT and disappearance of portal vein blood flow by color Doppler ultrasound. In the case where a patient is suspected of having SVT by color Doppler ultrasound, further verification with CT/MRI scan should be considered [77, 79].
Our subgroup analysis found that the incidence of SVT was higher in the cases where SVT was evaluated within 7 days after surgery than those where SVT was evaluated > 7 days after surgery. It seems to be counterintuitive that more SVT events are observed during a longer follow-up duration. However, it can be assumed that early asymptomatic SVT might be spontaneously resolved in some cases [80], which might lead to a relatively lower incidence of SVT detected during a longer follow-up period.
Several factors associated with coagulation and hemostasis have been identified as risk factors for SVT after splenectomy. First, lower preoperative platelet count and higher postoperative platelet count were risk factors for SVT after splenectomy in liver cirrhosis. This finding seemed to be a paradox. Indeed, a low preoperative platelet count indicated more severe portal hypertension, splenomegaly, and hypersplenism in liver cirrhosis. Because the spleen size is a well-known indicator for SVT after splenectomy [81], it is easy to understand that a low preoperative platelet count should also be considered as a risk factor for SVT. By comparison, a higher postoperative platelet count indicated a hypercoagulable state after splenectomy [11, 28, 44]. As known, platelet aggregation should be the first step of the blood coagulation process. A rapid increase of platelet count and augmented aggregation competence of platelets after splenectomy predispose to the development of SVT [82]. Second, mean platelet volume is positively related to platelet activity. When larger platelets are activated, more prethrombotic substances are released, such as P-selectin, platelet factor 4, and platelet-derived growth factor, thus promoting the formation of SVT. Third, P-selectin, a prethrombotic substance, can promote the adhesion of platelets to endothelial cells and inflammation of vascular wall [83], which may be related to the risk of thrombosis. Fourth, thrombus precursor protein is a soluble fibrin monomer, which is involved in the second step of the coagulation process. Soluble fibrin is converted into insoluble fibrin, which plays an important role in the formation of venous thromboembolism [84, 85]. Fifth, d-dimer is one of the fibrin degradation products, which is a sign of early thrombosis. Higher postoperative d-dimer level is associated with SVT after splenectomy, which is consistent with our previous meta-analysis that postoperative d-dimer level was significantly higher in the SVT group than the non-SVT group [86].
Several factors associated with anatomical structure have been identified as risk factors for SVT. First, wider preoperative portal and splenic vein diameter were significant risk factors for SVT after splenectomy. There are several possibilities for explaining this finding. (1) Wider portal and splenic vein diameter usually indicates higher portal pressure, which may cause vascular endothelial damage [24, 44], thereby triggering the coagulation system. (2) Wider portal and splenic vein diameter leads to a reduction of portal vein flow velocity [14, 28, 49, 87]. (3) A larger splenic vein can aggravate blood turbulence and stasis in the splenic vein stump after splenectomy, resulting in increased coagulation capacity [45, 59, 88]. Second, a patient with a massive spleen seems to have a wider splenic vein diameter which positively correlates with the rate of change of portal or splenic vein flow [88]. Once a massive spleen is removed, there is a more drastic change in portal or splenic blood flow, which enhances the development of SVT.
Several factors associated with surgery have been identified as risk factors for SVT. First, our subgroup analysis reported that the pooled incidence of SVT after LS seemed to be higher than that after OS. This may be because carbon dioxide (CO2) pneumoperitoneum significantly increases intra-abdominal pressure during laparoscopic procedures, thereby decreasing portal vein blood flow [89]. Moreover, CO2 pneumoperitoneum may lead to hypercoagulability [90]. In addition, the instrument for ligation of splenic vessels (LigaSure vessel-sealing device or harmonic shears) during LS may be a potential factor that contributes to the development of SVT by causing venous intimal damage using heat energy or oscillation [24], whereas the ligation of the splenic vessels during OS is mainly achieved by the application of traditional clamp and a ligature or suture with silk. Second, pericardial devascularization increases the risk of SVT after splenectomy, which may be due to a decreased blood flow in the portal system and more severe endothelial damage after devascularization [44, 69]. Third, pancreatic fistula develops as a potential complication of splenectomy due to damage of the pancreas tail, which may lead to pancreatic leakage and subphrenic inflammation, and in turn causes the portal vein inflammation and increases the risk of thrombosis [91].
Preventive antithrombotic therapy has been identified as a protective factor against SVT, which was consistent with our meta-analysis [92]. Anticoagulants can improve blood hypercoagulability, thereby reducing the occurrence of thrombosis [32, 93]. Theoretically, patients with liver cirrhosis have abnormal coagulation function and risk of bleeding, and early anticoagulation treatment after surgery may encounter the dilemma of bleeding. However, previous studies have shown that early use of anticoagulants after splenectomy in cirrhosis is a safe and effective regimen to prevent from SVT [93]. On the other hand, because increased platelet count and enhanced aggregation are important factors in the occurrence of SVT after splenectomy, it may be necessary to consider antiplatelet therapy after surgery. Aspirin has an antiplatelet aggregation effect and its efficacy in the prevention and treatment of thrombotic diseases has been recognized [94]. Zhou et al. reported that antiplatelet drugs after splenectomy in liver cirrhosis should be safe [11].
Our study had several limitations. First, the heterogeneity among studies was significant. Second, follow-up period was different among studies. Third, nine studies were published in the form of an abstract, in which some detailed information cannot be obtained. Fourth, the majority of included studies were retrospective, which might cause recall bias. Fifth, despite an absolute difference in the incidence of SVT among subgroups, a statistical comparison cannot be performed.
Conclusions
SVT is common in liver cirrhosis after splenectomy and splenic artery embolization. Early imaging screening should be valuable to improve the detection rate of asymptomatic SVT. Coagulation and hemostasis factors, anatomical factors, and surgery-related factors associated with development of SVT after splenectomy should be fully considered. Additionally, an early prophylactic strategy might be beneficial in patients at high risk for SVT. However, large-scale RCTs are necessary in future to explore the efficacy and safety of antithrombotic therapy for prevention of SVT after splenectomy.
References
Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371(9615):838–51.
Zhan XL, Ji Y, Wang YD. Laparoscopic splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension. World J Gastroenterol. 2014;20(19):5794–800.
Qi X, Li H, Liu X, et al. Novel insights into the development of portal vein thrombosis in cirrhosis patients. Expert Rev Gastroenterol Hepatol. 2015;9(11):1421–32.
Wang YB, Zhang JY, Zhang F, Zhao Y, Gong JP. Partial splenic artery embolization to treat hypersplenism secondary to hepatic cirrhosis: a meta-analysis. Am Surgeon. 2017;83(3):274–83.
Wright AS, Rikkers LF. Current management of portal hypertension. J Gastrointest Surg. 2005;9(7):992–1005.
Hadduck TA, McWilliams JP. Partial splenic artery embolization in cirrhotic patients. World J Radiol. 2014;6(5):160–8.
Petermann A, Chabrot P, Cassagnes L, et al. Hypersplenism due to portal hypertension: retrospective evaluation of 17 patients treated by splenic embolization. Diagn Interv Imaging. 2012;93(1):30–6.
Zhang B, Kim M, Griffiths C, et al. Incidence of splanchnic vein thrombosis after abdominal surgery: a systematic review and meta-analysis. J Surg Res. 2020;245:500–9.
Guan YS, Hu Y. Clinical application of partial splenic embolization. Sci World J. 2014;2014:961345.
Bai DS, Xia BL, Zhang C, et al. Warfarin versus aspirin prevents portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection: a randomized clinical trial. Int J Surg. 2019;64:16–23.
Zhou JB, Luo BY, Liu CW, Zhu F. Effects of early antiplatelet therapy after splenectomy with gastro-oesophageal devascularization. ANZ J Surg. 2018;88(10):E725–9.
Wei Y, Chen X, Shen H, et al. P-selectin level at first and third day after portal hypertensive splenectomy for early prediction of portal vein thrombosis in patients with cirrhosis. Clin Appl Thromb Hemost. 2018;24(9_suppl):76s–83s.
Matsui T, Usui M, Wada H, et al. Platelet activation assessed by glycoprotein vi/platelet ratio is associated with portal vein thrombosis after hepatectomy and splenectomy in patients with liver cirrhosis. Clin Appl Thromb Hemost. 2018;24(2):254–62.
Huang L, Yu Q, Wang J. Association between changes in splanchnic hemodynamics and risk factors of portal venous system thrombosis after splenectomy with periesophagogastric devascularization. Med Sci Monitor. 2018;24:4355–62.
Dawoud M, Hamisa M, Behiery A, Abed O. Gel foam or microsphere particles for partial splenic artery embolization in managing patients with hypersplenism. Egypt J Radiol Nuclear Med. 2018;49(3):804–14.
Alla H. Post-splenectomy portal venous thrombosis in cirrhotic patients: an observational clinical trial. Surg Endosc. 2018;32(1):S275.
Qian YY, Li K. The early prevention and treatment of PVST after laparoscopic splenectomy: a prospective cohort study of 130 patients. Int J Surg. 2017;44:147–51.
Oshima M, Uemura J, Ando Y, Suto H, Okano KYS. Laparoscopic splenectomy for thrombocytopenia could ameliorate liver function in a selected population classified into Child Pugh grade B with liver cirrhosis. J Hepatobiliary Pancreat Sci. 2017;24:A196.
Bao H, He Q, Dai N, Ye R, Zhang Q. Retrospective study to compare selective decongestive devascularization and gastrosplenic shunt versus splenectomy with pericardial devascularization for the treatment of patients with esophagogastric varices due to cirrhotic portal hypertension. Med Sci Monitor. 2017;23:2788–95.
Assal F, El Kassas M, Esmail E, et al. Microwave ablation in the spleen versus partial splenic artery embolisation: a new technique for hypersplenism in cirrhosis. Arab J Gastroenterol. 2017;18(1):25–9.
Wang M, Wei A, Zhang Z, Peng B. Laparoscopic splenectomy for the elderly liver cirrhotic patients with hypersplenism: a retrospective comparable study. Medicine. 2016;95(10):e3012.
Qi X, Han G, Ye C, et al. Splenectomy causes 10-fold increased risk of portal venous system thrombosis in liver cirrhosis patients. Med Sci Monitor. 2016;22:2528–50.
Jiao S, Chen H, Wang Y, Zhu J, Tan J, Gao J. Splenectomy versus partial splenic embolization for massive splenomegaly secondary to hepatitis B-related liver cirrhosis: a case-control study. Gastroenterol Res Pract. 2016;2016:3471626.
Jiang GQ, Bai DS, Chen P, Qian JJ, Jin SJ, Wang XH. Risk factors for portal vein system thrombosis after laparoscopic splenectomy in cirrhotic patients with hypersplenism. J Laparoendosc Adv Surg Tech Part A. 2016;26(6):419–23.
Chen X, Li J, Xu J, et al. Percutaneous transhepatic variceal embolization combined with partial splenic embolization for treatment of esophagogastric variceal bleeding in patients with liver cirrhosis. Chin J Gastroenterol. 2016;21(4):197–201.
Yang S, He C, Fan X, Ding W, Wu X, Li J. Early prophylactic anticoagulation via transjugular intrahepatic route for portal vein thrombosis after splenectomy in cirrhotic portal hypertension. J Vasc Interv Radiol. 2015;26(7):1009–17.
Yamamoto N, Okano K, Oshima M, et al. Laparoscopic splenectomy for patients with liver cirrhosis: improvement of liver function in patients with Child-Pugh class B. Surgery. 2015;158(6):1538–44.
Wu S, Wu Z, Zhang X, Wang R, Bai J. The incidence and risk factors of portal vein system thrombosis after splenectomy and pericardial devascularization. Turk J Gastroenterol. 2015;26(5):423–8.
Kawanaka H, Akahoshi T, Kinjo N, et al. Laparoscopic splenectomy with technical standardization and selection criteria for standard or hand-assisted approach in 390 patients with liver cirrhosis and portal hypertension. J Am Coll Surg. 2015;221(2):354–66.
Hongwei C, Zhang L, Maoping L, Yong Z, Chengyou D, Dewei L. Era of liver transplantation: combined anatomic splenectomy and anticoagulant therapy in prevention of portal vein thrombosis after splenectomy. Hepatogastroenterology. 2015;62(138):405–9.
He S, He F. Predictive model of portal venous system thrombosis in cirrhotic portal hypertensive patients after splenectomy. Int J Clin Exp Med. 2015;8(3):4236–42.
Cheng Z, Yu F, Tian J, et al. A comparative study of two anti-coagulation plans on the prevention of PVST after laparoscopic splenectomy and esophagogastric devascularization. J Thromb Thrombolysis. 2015;40(3):294–301.
Shi R, Zhang YM, Zhu ZJ, et al. Synchronous splenectomy and hepatectomy in patients with hepatocellular carcinoma, hypersplenism and liver cirrhosis. Hepatogastroenterology. 2014;61(133):1363–7.
Ogata T, Okuda K, Sato T, et al. Long-term outcome of splenectomy in advanced cirrhotic patients with hepatocellular carcinoma and thrombocytopenia. Kurume Med J. 2013;60(2):37–45.
Jiang GQ, Chen P, Qian JJ, et al. Perioperative advantages of modified laparoscopic vs open splenectomy and azygoportal disconnection. World J Gastroenterol. 2014;20(27):9146–53.
Iida H, Aihara T, Ikuta S, Yamanaka N. Predictive factors of portal vein thrombus following splenectomy in patients with severe cirrhosis. Hepatogastroenterology. 2014;61(134):1552–5.
Huang N, Ji F, Zhou R, et al. Splenectomy improve long-term prognosis in cirrhotic patients with portal hypertension and hypersplenism, and facilitate adherence to subsequent treatment programs for hepatitis C. Hepatol Int. 2014;8(1):S370.
Han J, Yi Y, Ding H, et al. Preoperative risk factors of portal venous thrombosis after splenectomy and gastric pericardial devascularization for portal hypertension. Zhonghua Gan Zang Bing Za Zhi = Chin J Hepatol. 2014;22(10):739–43.
Cheng Z, Li JW, Chen J, Fan YD, Guo P, Zheng SG. Therapeutic effects of laparoscopic splenectomy and esophagogastric devascularization on liver cirrhosis and portal hypertension in 204 cases. J Laparoendosc Adv Surg Tech Part A. 2014;24(9):612–6.
Zhou J, Wu Z, Wu J, et al. Transjugular intrahepatic portosystemic shunt (TIPS) versus laparoscopic splenectomy (LS) plus preoperative endoscopic varices ligation (EVL) in the treatment of recurrent variceal bleeding. Surg Endosc. 2013;27(8):2712–20.
Zhao S, Lv T, Gong G, Wang C, Huang B, Zhou W. Outcome of laparoscopic splenectomy with sandwich treatment including pericardial devascularization and limited portacaval shunt for portal hypertension due to liver cirrhosis. J Laparoendosc Adv Surg Tech Part A. 2013;23(1):43–7.
Wu Z, Zhou JBP. Laparoscopic splenectomy versus partial splenic embolization for the management of hypersplenism in cirrhotic patients. Surg Endosc. 2013;27:S452.
Wang WD, Lin J, Chen XW, Wu ZQ, Liu QB, He W. Laparoscopic periesophagogastric devascularization and splenectomy in the management of portal hypertension. HPB. 2013;15(SUPPL. 2):114–5.
Li MX, Zhang XF, Liu ZW, Lv Y. Risk factors and clinical characteristics of portal vein thrombosis after splenectomy in patients with liver cirrhosis. Hepatobiliary Pancreat Dis Int. 2013;12(5):512–9.
Kakinoki K, Okano K, Suto H, et al. Hand-assisted laparoscopic splenectomy for thrombocytopenia in patients with cirrhosis. Surg Today. 2013;43(8):883–8.
Ji F, Zhang S, Huang N, Deng H, Li Z. Splenectomy prior to antiviral therapy in patients with hepatitis C virus related decompensated cirrhosis. Braz J Infect Dis. 2013;17(5):601–5.
Cai M, Zhu K, Huang W, et al. Portal vein thrombosis after partial splenic embolization in liver cirrhosis: efficacy of anticoagulation and long-term follow-up. J Vasc Interv Radiol. 2013;24(12):1808–16.
Zhou J, Wu Z, Pankaj P, Peng B. Long-term postoperative outcomes of hypersplenism: laparoscopic versus open splenectomy secondary to liver cirrhosis. Surg Endosc. 2012;26(12):3391–400.
Zhang Y, Wen TF, Yan LN, et al. Preoperative predictors of portal vein thrombosis after splenectomy with periesophagogastric devascularization. World J Gastroenterol. 2012;18(15):1834–9.
Murugesan B, Jain D, Mukund ASS. Partial splenic embolization in hepatitis C virus related cirrhosis: prior to pegylated interferon based therapy. Hepatol Int. 2012;6(1):182–3.
Lai W, Lu SC, Li GY, et al. Anticoagulation therapy prevents portal-splenic vein thrombosis after splenectomy with gastroesophageal devascularization. World J Gastroenterol. 2012;18(26):3443–50.
Akahoshi T, Tomikawa M, Kawanaka H, et al. Laparoscopic splenectomy with interferon therapy in 100 hepatitis-C-virus-cirrhotic patients with hypersplenism and thrombocytopenia. J Gastroenterol Hepatol. 2012;27(2):286–90.
Yao HS, Wang WJ, Wang Q, et al. Randomized clinical trial of vessel sealing system (LigaSure) in esophagogastric devascularization and splenectomy in patients with portal hypertension. Am J Surg. 2011;202(1):82–90.
Ushitora Y, Tashiro H, Takahashi S, et al. Splenectomy in chronic hepatic disorders: portal vein thrombosis and improvement of liver function. Dig Surg. 2011;28(1):9–14.
Pan WD, Xu RY. Precaution of the portal system thrombosis in patients with portal hypertension of cirrhosis resulting from hepatitis after splenectomy. J Gastroenterol Hepatol. 2011;26(SUPPL. 5):140.
Elmonem SA, Tantawy HI, Ragheb AS, Matar NEH. The outcome of partial splenic embolization for hypersplenism in the cirrhotic patients. Egypt J Radiol Nuclear Med. 2011;42(1):35–42.
Wang L, Liu GJ, Chen YX, Dong HP, Zhang YQ, Wang LX. Combined use of D-dimer and P-selectin for the diagnosis of splenic or portal vein thrombosis following splenectomy. Thromb Res. 2010;125(5):e206–9.
Meng J, Lu SC, Wang ML, Goa F. Portal vein thrombosis after splenectomy for hypersplenism in patients with liver cirrhosis: an analysis of 22 cases. World Chin J Digestol. 2010;18(33):3584.
Kinjo N, Kawanaka H, Akahoshi T, et al. Risk factors for portal venous thrombosis after splenectomy in patients with cirrhosis and portal hypertension. Br J Surg. 2010;97(6):910–6.
Imura S, Shimada M, Utsunomiya T, et al. Impact of splenectomy in patients with liver cirrhosis: results from 18 patients in a single center experience. Hepatol Res. 2010;40(9):894–900.
Zhu K, Meng X, Qian J, et al. Partial splenic embolization for hypersplenism in cirrhosis: a long-term outcome in 62 patients. Dig Liver Dis. 2009;41(6):411–6.
Yoshida M, Watanabe Y, Horiuchi A, Yamamoto Y, Sugishita H, Kawachi K. Portal and splenic venous thrombosis after splenectomy in patients with hypersplenism. Hepatogastroenterology. 2009;56(90):538–41.
Sawhney R, Howell JA, Schelleman AG, Goodwin M, Gow PJ. Partial splenic embolisation for management of hypersplenism in patients with hepatitis C cirrhosis prior to antiviral therapy. J Gastroenterol Hepatol. 2009;2009:A294.
Morihara D, Kobayashi M, Ikeda K, et al. Effectiveness of combination therapy of splenectomy and long-term interferon in patients with hepatitis C virus-related cirrhosis and thrombocytopenia. Hepatol Res. 2009;39(5):439–47.
Matsumoto T, Yamagami T, Terayama K, et al. Risk factors and clinical course of portal and/or splenic vein thrombosis after partial splenic embolization. Acta Radiol. 2009;50(6):617–23.
Amin MA, el-Gendy MM, Dawoud IE, Shoma A, Negm AM, Amer TA. Partial splenic embolization versus splenectomy for the management of hypersplenism in cirrhotic patients. World J Surg. 2009;33(8):1702–10.
Watanabe Y, Horiuchi A, Yoshida M, et al. Significance of laparoscopic splenectomy in patients with hypersplenism. World J Surg. 2007;31(3):549–55.
Deng MH, Liu B, Fang HP, et al. Predictive value of D-dimer for portal vein thrombosis after portal hypertension surgery in hepatitis B virus-related cirrhosis. World J Gastroenterol. 2007;13(48):6588–92.
Lin N, Liu B, Xu RY, Fang HP, Deng MH. Splenectomy with endoscopic variceal ligation is superior to splenectomy with pericardial devascularization in treatment of portal hypertension. World J Gastroenterol. 2006;12(45):7375–9.
N’Kontchou G, Seror O, Bourcier V, et al. Partial splenic embolization in patients with cirrhosis: efficacy, tolerance and long-term outcome in 32 patients. Eur J Gastroenterol Hepatol. 2005;17(2):179–84.
Foruny JR, Blázquez J, Moreno A, et al. Safe use of pegylated interferon/ribavirin in hepatitis C virus cirrhotic patients with hypersplenism after partial splenic embolization. Eur J Gastroenterol Hepatol. 2005;17(11):1157–64.
Wang MC, Li S, Zhu JY, Leng XS, Du RY. The reason and treatment of portal vein thrombosis in patients with portal hypertension postoperation. Zhonghua Wai Ke Za Zhi [Chin J Surg]. 2004;42(5):269–71.
Liu B, Lin N, Xu RY. Splenectomy combined with endoscopic variceal ligation in treating portal hypertension. Zhong Nan Da Xue Xue Bao Yi Xue Ban = J Central South Univ Med Sci. 2004;29(1):87–9.
Eguchi A, Hashizume M, Kitano S, Tanoue K, Wada H, Sugimachi K. High rate of portal thrombosis after splenectomy in patients with esophageal varices and idiopathic portal hypertension. Arch Surg. 1991;126(6):752–5.
Owman T, Lunderquist A, Alwmark A, Borjesson B. Embolization of the spleen for treatment of splenomegaly and hypersplenism in patients with portal hypertension. Invest Radiol. 1979;14(6):457–64.
Manzano-Robleda Mdel C, Barranco-Fragoso B, Uribe M, Méndez-Sánchez N. Portal vein thrombosis: what is new? Ann Hepatol. 2015;14(1):20–7.
Intagliata NM, Caldwell SH, Tripodi A. Diagnosis, development, and treatment of portal vein thrombosis in patients with and without cirrhosis. Gastroenterology. 2019;156(6):1582-99.e1.
Stine JG, Northup PG. Management of non-tumoral portal vein thrombosis in patients with cirrhosis. Dig Dis Sci. 2019;64(3):619–26.
Margini C, Berzigotti A. Portal vein thrombosis: the role of imaging in the clinical setting. Dig Liver Dis. 2017;49(2):113–20.
Qi X, Guo X, Yoshida EM, et al. Transient portal vein thrombosis in liver cirrhosis. BMC Med. 2018;16(1):83.
Weledji EP. Benefits and risks of splenectomy. Int J Surg. 2014;12(2):113–9.
Chu SG, Becker RC, Berger PB, et al. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost. 2010;8(1):148–56.
Blann AD, Nadar SK, Lip GY. The adhesion molecule P-selectin and cardiovascular disease. Eur Heart J. 2003;24(24):2166–79.
Song KS, Kim HK, Song JW. Measurement of thrombus precursor protein in septic patients with disseminated intravascular coagulation and liver disease. Haematologica. 2002;87(10):1062–7.
Carville DG, Dimitrijevic N, Walsh M, et al. Thrombus precursor protein (TpP): marker of thrombosis early in the pathogenesis of myocardial infarction. Clin Chem. 1996;42(9):1537–41.
Dai J, Qi X, Li H, Guo X. Role of D-dimer in the development of portal vein thrombosis in liver cirrhosis: a meta-analysis. Saudi J Gastroenterol. 2015;21(3):165–74.
Qi X, Han G, Fan D. Management of portal vein thrombosis in liver cirrhosis. Nature Rev Gastroenterol Hepatol. 2014;11(7):435–46.
Danno K, Ikeda M, Sekimoto M, et al. Diameter of splenic vein is a risk factor for portal or splenic vein thrombosis after laparoscopic splenectomy. Surgery. 2009;145(5):457–64 (discussion 65–6).
Klopfenstein CE, Morel DR, Clergue F, Pastor CM. Effects of abdominal CO2 insufflation and changes of position on hepatic blood flow in anesthetized pigs. Am J Physiol. 1998;275(3):H900–5.
Lindberg F, Rasmussen I, Siegbahn A, Bergqvist D. Coagulation activation after laparoscopic cholecystectomy in spite of thromboembolism prophylaxis. Surg Endosc. 2000;14(9):858–61.
Tsutsumi N, Tomikawa M, Akahoshi T, et al. Pancreatic fistula after laparoscopic splenectomy in patients with hypersplenism due to liver cirrhosis: effect of fibrin glue and polyglycolic acid felt on prophylaxis of postoperative complications. Am J Surg. 2016;212(5):882–8.
Qi X, Bai M, Guo X, Fan D. Pharmacologic prophylaxis of portal venous system thrombosis after splenectomy: a meta-analysis. Gastroenterol Res Pract. 2014;2014:292689.
Jiang GQ, Xia BL, Chen P, et al. Anticoagulation therapy with warfarin versus low-dose aspirin prevents portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection. J Laparoendosc Adv Surg Tech Part A. 2016;26(7):517–23.
Paikin JS, Wright DS, Eikelboom JW. Effectiveness and safety of combined antiplatelet and anticoagulant therapy: a critical review of the evidence from randomized controlled trials. Blood Rev. 2011;25(3):123–9.
Acknowledgements
Funding
The study was partially supported by the Science and Technology Project Foundation of Shenyang (19-112-4-005). No Rapid Service Fee was received by the journal for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Authorship Contributions
All authors made substantial contributions to the intellectual content of this paper. YW: methodology; formal analysis; investigation; writing–original draft; writing–review and editing. HL: validation; writing–original draft; writing–review and editing. TZ: formal analysis; writing–review and editing. ZB: data curation; writing–review and editing. XX: formal analysis; validation; writing–review and editing. GBLS: writing–review and editing. LW: data curation. XQ, conceptualization; methodology; validation; investigation; writing–original draft; writing–review and editing; supervision; project administration.
Prior Publication
This work was partially presented as a poster presentation at the Asian-Pacific Association for the Study of Liver (APASL) 2020 Conference held in Bali, Indonesia from March 4, 2020 to March 8, 2020. Please see the following link https://springerlink.bibliotecabuap.elogim.com/content/pdf/10.1007/s12072-020-10030-4.pdf.
Disclosures
Yanyan Wu, Hongyu Li, Tiansong Zhang, Zhaohui Bai, Xiangbo Xu, Giovanni Battista Levi Sandri, Le Wang, and Xingshun Qi have nothing to disclose.
Compliance with Ethics Guidelines
This is a meta-analysis based on previously published studies and does not involve any new studies of human or animal subjects performed by any of the authors. The work is conducted according to MOOSE and PRISMA. The MOOSE and PRISMA checklists are shown in the supplementary material.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, Y., Li, H., Zhang, T. et al. Splanchnic Vein Thrombosis in Liver Cirrhosis After Splenectomy or Splenic Artery Embolization: A Systematic Review and Meta-Analysis. Adv Ther 38, 1904–1930 (2021). https://doi.org/10.1007/s12325-021-01652-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01652-7