Abstract
Introduction
The health benefits of entering methadone maintenance treatment (MMT) for opioid-dependent persons may not be merely limited to therapy of opioid use disorder. We aimed to compare the healthcare utilization of MMT patients before and after MMT.
Methods
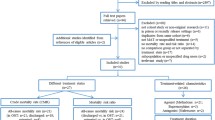
A retrospective analysis was performed using the Taiwan Illicit Drug Issue Database and the National Health Insurance Research Database (NHIRD) between 2014 and 2016. We included 1255 newly enrolled MMT patients in 2015 and randomly selected 5020 patients from NHIRD matched by age and gender as the comparison group. Changes in healthcare utilization 1 year before and 1 year after the date of the index date (MMT initiation) were compared within and between MMT and comparison groups.
Results
During the 1-year period following MMT, the hospitalization length was considerably decreased, while the number of outpatient visits, emergency department (ED) visits, and ED expenditure significantly increased in MMT patients. Multivariable linear regression with the difference-in-difference approach revealed that all the categories of healthcare utilization increased, except for a minor increase of outpatient expenditure and a slight decrease of hospitalization length for the MMT group relative to the comparison group. Increases in utilization of the departments of psychiatry and infectious diseases of the MMT patients were considerable.
Conclusion
MMT is associated with increased healthcare utilization, and departments of psychiatry and infectious diseases play substantial roles. Policy-makers should warrant access for all who need healthcare by ensuring the availability of the treatment for drug dependence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Why carry out this study? |
Individuals with substance use disorders experience enormous health inequities. |
The health benefits of methadone maintenance treatment (MMT) for opioid-dependent persons may not be limited to therapy of opioid use disorder (OUD). |
What was learned from the study? |
Healthcare utilization was increased in patients with OUD after entering MMT. |
Visits of departments of psychiatry and infectious diseases were increased in MMT patients. |
MMT might facilitate the access to healthcare for patients with OUD and thereby eliminate health inequities. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13606547.
Introduction
Individuals with substance use disorders experience tremendous health inequities across a broad range of health conditions [1]. People dependent on illicit drugs have particularly high relative risks of overdose, mental health problems, and infection by HIV and hepatitis C virus, which contribute to excess morbidity and mortality [2,3,4]. Compared with the general population, people who use illicit drugs are admitted to emergency departments (ED) or hospitals more frequently [5,6,7,8]. Medication treatment for opioid use disorder (OUD), such as methadone maintenance treatment (MMT), has been consistently correlated with reduced ED presentation or hospital admission in previous studies [5, 7, 9,10,11]. Yet, many studies fail to acknowledge that increased engagement in non-crisis medical care is essential for successful long-term recovery from OUD [12,13,14].
In Taiwan, MMT services have developed into a nationwide harm reduction program for patients with OUD since 2006 [15, 16]. Because the expenses of medical treatment for drug use disorders are not paid by Taiwan National Health Insurance (NHI), the Ministry of Health and Welfare (MOHW) subsidies the expenditure of MMT using special budgets to facilitate the access to MMT for patients with OUD [17]. Additionally, NHI began to cover the incarcerated populations in 2013, indicating that incarcerated people who use heroin have had full access to healthcare since then. Considering the medical needs of patients with OUD [18], it is crucial to understand how the frequency and costs of healthcare utilization in people with heroin use disorders are affected by MMT under complete health insurance coverage. To investigate the changes affected by MMT, we identified the MMT patients in 2015 by the Taiwan Illicit Drug Issue Database (TIDID) and compared their healthcare utilization and expenditure 1 year before and 1 year after MMT using the National Health Insurance Research Database (NHIRD). A non-MMT group with a four-fold number of participants and matched by the age and gender of the MMT patients were randomly selected from the NHIRD, and the differences between and within the MMT and non-MMT groups were examined.
Methods
Data Source
The TIDID [19], which includes the Database of Substitution Therapy from the Department of Mental and Oral Health, MOHW, is an interagency database dedicated to people who use illicit drugs in Taiwan. Taiwan’s NHIRD is constituted by claims data of the Taiwan NHI, a mandatory single-payer health insurance program covering 99% of the population in Taiwan [20, 21]. The TIDID and NHIRD are both maintained by the Health and Welfare Data Science Center (HWDC), providing domestic analysis access for research purposes. The databases can be linked to each other within the Health and Welfare Data Center (HWDC) by individual personal identification numbers to provide patient-level information on demographic characteristics for research [20].
The TIDID contains illicit drug user data on date of birth, sex, and the date of MMT entry. The NHIRD holds patient data on healthcare utilization and diseases diagnosed according to the codes in the International Classification of Diseases, Ninth or Tenth Revision, Clinical Modification (ICD-9-CM or ICD-10-CM). The data used in this study were in compliance with the regulations of the HWDC to ensure patient privacy. The Ethics Review Board of National Health Research Institutes in Taiwan approved this study (EC1060510-E-R1).
Diagnosis-related groups (DRGs), a prospective payment system, aims to reduce inefficiency and restrain costs. The NHI Administration has gradually implemented the Taiwan-version DRG payment system (Tw-DRG) since 2010. Similar to the DRG policies of other countries, the Tw-DRG system classifies hospitalized cases according to variables such as procedures performed, primary and secondary diagnoses, patient age and sex, discharge status, and the presence of complications or comorbidities [22]. The assumption is that patients belonging to a particular DRG are clinically and economically homogeneous in their resource consumption pattern. Related studies have indicated that the DRG policy significantly shortened patients’ length of stay and decreased the intensity of care during hospitalization [23].
Study Population
We identified MMT patients between 2012 and 2016 from the TIDID, and chose those admitted to MMT for the first time during 2015 (i.e., no MMT record during 2012–2014). The index date for each patient was defined by the date of taking the first MMT prescription. Under the current law in Taiwan, uncaptured heroin users (i.e., those not detected by the police) who sought MMT will initiate the treatment if no unsuitable health issues were found. On the other hand, captured heroin users either receive MMT or are imprisoned. Because imprisonment could considerably affect one’s behavior in relation to healthcare utilization, we chose the general population instead of heroin users who did not initiate MMT as the comparison group, in order to adjust the underlying, external temporal effect in operation, such as the health insurance reimbursement policy and disease epidemiology. The comparison group comprised a randomly selected cohort of patients without illicit drug use records from the NHIRD, frequency matched with age and sex. The index date for each comparison patient was assigned as the 15th of a randomly assigned month in 2015. Overall, the MMT and the comparison groups comprised 1255 and 5020 participants, respectively.
For all the study participants, the records of outpatient visits (not inclusive of MMT visits), outpatient expenditure, ED visits, ED expenditure, hospitalizations, hospitalization expenditures, and the length of hospital stays [24,25,26] during the 1-year period before and 1-year period after the index date were extracted. The primary outcome of this study was the changes in healthcare utilization between the two 1-year periods.
Demographic factors encompassed age (in groups aged 18–29, 30–39, 40–49, and 50 years and older) and sex. Comorbidities were assigned if patients were diagnosed with depression (ICD-9-CM 290.21, 296.20, 296.21, 296.22, 296.23, 296.24, 296.30, 296.31, 296.32, 296.33, 296.34, 296.8, 300.4, and 311), human immunodeficiency virus (HIV) (ICD-9-CM 042), hepatitis C virus (HCV) (ICD-9-CM 070.41, 070.44, 070.51, 070.54, 070.70, 070.71, and V0262), hepatitis B virus (HBV) (ICD-9-CM 070.20, 070.21, 070.22, 070.23, 070.30, 070.31, 070.32, 070.33, 070.42, 070.52, and V0261), or alcoholic liver disease (ALD) (ICD-9-CM 571.0, 571.1, 571.2, and 571.3) during 2012–2016.
Statistics
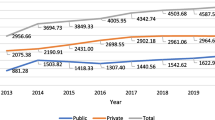
The chi-square test was used to determine the differences between the two groups in the distribution of the comorbidities. To observe patterns of healthcare utilization, we calculated the 30-day mean number of outpatient visits, outpatient expenditure, ED visits, ED expenditure, hospitalizations, hospitalization expenditures, and hospitalization length during the two 1-year periods before and 1-year periods after the index date for the MMT and comparison groups. The unit of healthcare expenditures is the medical point, where in most cases 1 point equals 1 NTD (New Taiwan Dollar). The 30-day mean number of visits was derived from the sum of total visits within 30 days among 1255 patients divided by 1255 in the MMT group and the sum of total visits among 5020 participants divided by 5020 in the comparison group. For the 1-year pre- or post-periods, we calculated the sum of total visits within the 1-year pre- or post-MMT (or pre- or post- the index date for the comparison group) divided by 1255 in the MMT group and 5020 in the comparison group. The differences in the mean changes between the two 1-year periods were checked by the Wilcoxon signed-rank test. The difference-in-difference (DID) approach was used to measure the effect of MMT by comparing the change in health care utilization and expenditure 1 year pre- and post-MMT (or pre- or post- the index date for the comparison group) between the MMT and the comparison group. A DID approach focused on the change in the outcome of interest between 1 year pre- and post-MMT, and was not influenced by the different start levels of outcome in the MMT and the comparison groups. The DID estimates are based on the following equation:
where subscript i indicates the participants, 1 and 2 designate the time points (before and after MMT, respectively). (Yi2 − Yi1) is the difference in the outcome of interest (i.e., health care utilization and expenditure) between 1 year pre- and post-MMT for individual i, Ii represents the indicator variable of treatment, while Ii = 0,1 represents the treatment status of individual i (MMT or the comparison group), Xi stands for baseline covariates: age, sex, and comorbidities including depression, HIV, HCV, HBV, and ALD for individual i, and \({\epsilon }_{i}\) is the error term. An alpha < 0.05 was considered to indicate statistical significance; all tests were two-tailed. For the DID estimate in Table 2, an alpha < 0.007 was considered to be statistical significant after Bonferroni correction for multiple comparisons. Numbers of outpatient visits and hospitalizations classified by the healthcare departments were retrieved from both the MMT and comparison groups before and after the index date, and then visualized by bar charts. All data management, statistical analyses, and the figures were performed and generated using Microsoft Excel 2016 (Microsoft, Redmond, WA, USA), SAS 9.4 (SAS Institute, Cary, NC, USA), and Prism (GraphPad Software, La Jolla, CA, USA).
Results
Cohort Characteristics
The study participants consisted of 1040 (82.9%) men and 215 (17.1%) women in the MMT group (Table 1). For the matched cohort, 4160 (82.9%) men and 860 (17.1%) women were selected from the general population. The mean age of both the MMT and comparison groups was 42 years (SD 8.1 years), and about 80% of them were aged between 30 and 49 years. Of the MMT patients, 15.3% were diagnosed to have depression, and 10.4% of the MMT patients had HCV. The proportions of other comorbidities, i.e., HIV and ALD, were also significantly higher in the MMT group than in the comparison group. There was no significant difference in HBV between the MMT and comparison groups. The mean duration in the MMT program was 228 days (SD 209 days), with 368 patients (29.3%) retained in the MMT program at the end of the 1-year follow-up period.
Changes of Healthcare Utilization
Table 2 showed healthcare utilization and expenditure changes within 1 year before and 1 year after MMT (or the index date in the comparison group). The outpatient and ED visits in the MMT group significantly increased after MMT (annual mean number of visits per person from 15 to 17 and from 0.6 to 0.7; P = 0.018 and 0.002, respectively), while those in the comparison group did not alter very much. The numbers of hospitalizations before and after the index date in both MMT and comparison groups were not significantly different. The outpatient expenditures did not change noticeably in both MMT and comparison groups after the index date. The ED expenditures increased by 447 medical points after MMT in the MMT group (P = 0.010), but did not change substantially in the comparison group. There was no obvious change for hospitalization expenditures in either group. After the index date, the hospitalization length was shorter in both the MMT (annual mean hospitalization length per person dropped from 1.15 to 0.83 days; P < 0.001) and comparison groups (from 0.35 to 0.32 days; P = 0.045).
We further compared the degree of changes in both groups. Assessed with the comparison group, the numbers of outpatient visits, ED visits, and hospitalizations increased more in the MMT group [adjusted difference with 95% CI = 2.14 (1.36, 2.92), 0.10 (0.03, 0.16), and 0.13 (0.07, 0.18), respectively]. The expenditures of ED visits, and hospitalizations increased more in the MMT group than in the comparison group [adjusted difference with 95% CI = 538 (199, 878), 9 695 (4 536, 14 853) medical points, respectively). The length of hospitalization was slightly shorter in the MMT group after the index date [adjusted difference with 95% CI = – 0.15 ( – 0.37, 0.08) days].
Figure 1 demonstrates the monthly changes of mean number and expenditures in healthcare utilization within 1 year before and 1 year after the MMT. Month 0 indicates the index date. The outpatient visits in the MMT group increased after MMT, while the numbers in the comparison group were similar before and after the index date. However, the outpatient expenditures did not appear to change perceptibly after MMT in the MMT group. The ED visits in the MMT group increased within 6 months after MMT and then declined to a similar level as those before MMT, while the latter did not change sizably after the index date in the comparison group. There was an evident peak for the ED expenditures in the 12th month after MMT in the MMT group, which might be due to a few extremely costly ED managements for the limited number of patients utilizing ED. The number of hospitalizations and hospitalization expenditures did not show obvious trends before and after MMT. The hospitalization length also did not show noticeable trends before and after MMT.
Healthcare Utilization by Departments
We performed a comprehensive analysis on the healthcare utilization of the MMT and comparison groups classified by the healthcare departments before and after the index date. Figure 2a illustrates the number of outpatient visits. Before MMT, the top five visited departments in the MMT group were Psychiatry, Family Medicine (designated as Primary Care General Practice in Europe), General Medicine, Dentistry, and Orthopedics, while in the comparison group, they were Family Medicine, Chinese Medicine, Otolaryngology, Dentistry, and General Medicine. After MMT, the top five utilized departments in the MMT group were Psychiatry, Family Medicine, General Medicine, Dentistry, and General Surgery, while in the comparison group, they were Family Medicine, Chinese Medicine, Otolaryngology, Dentistry, and General Medicine. The number of visits to the departments of Psychiatry and Family Medicine increased drastically after MMT (Fig. 2a, left panel), but this trend was not observed in the comparison group (Fig. 2a, right panel).
Figure 2b shows the number of hospitalizations classified by the departments. Before MMT, the top six utilized departments in the MMT group were Orthopedics, General Surgery, Gastroenterology, Infectious Diseases, Neurosurgery, and Plastic Surgery (the last two tied), while the top five visited departments in the comparison group were Orthopedics, Obstetrics & Gynecology, General Surgery, Gastroenterology, and Urology. After MMT, the top five utilized departments in the MMT group were Orthopedics, Infectious Diseases, Psychiatry, General Surgery, and Chest Medicine, while the top six used departments in the comparison group were Chest Medicine, Obstetrics & Gynecology, Psychiatry, Orthopedics, Gastroenterology, and Urology (the last two were equal). The number of hospitalizations to the departments of Infectious Diseases and Cardiovascular Medicine increased radically after MMT (Fig. 2b, left panel), but the same tendency was not seen in the comparison group (Fig. 2b, right panel).
Discussion
Through comparing the healthcare utilization 1 year before and 1 year after the index date in the MMT and comparison groups, we found that MMT is related to increased healthcare utilization (outpatient visits, ED visits, ED expenditures, hospitalizations, and hospitalization expenditures). Utilization of psychiatry and infectious diseases departments increased considerably in MMT patients.
In Taiwan, a complete course of MMT is 6–12 months. Therefore, patients may leave MMT after 6 months if judged by certified psychiatrists to be unlikely to use heroin again. The mean duration of 228 days falls reasonably between 6 months (183 days) and 12 months (365 days). We chose 1 year instead of longer periods as the cutoff point in order to eliminate the time-dependent effects of on- and off-MMT. As Fig. 1 reveals, the numbers of ED visits and hospitalization did not go up after 8 months (240 days), implying that the off-MMT-associated elevated risk of overdose and consequent ED admission/hospitalization did not play a major role in the 1-year study period.
Patients with OUD have a high degree of healthcare needs, and their frequent visits to the MMT clinics offer the opportunity for easily accessible healthcare [27, 28]. Although there have been several studies evaluating the healthcare utilization of people who use heroin in Taiwan [9, 12, 29], our study is the first nationwide investigation assessing the differences between pre- and post-MMT. Consistent with previous studies, our results demonstrated the higher prevalence of depression, HIV, and HCV of the MMT patients, compared with patients without illicit drug use records, and enhanced utilization of outpatient services after receiving MMT. The numbers of ED visits and hospitalizations increased post-MMT in our study, which was the opposite of the findings noted in a recent review that opioid substitution therapy was consistently associated with reduced ED presentation and hospital admission [5]. One possible explanation was that these increases originated from previously unmet medical needs, and prevented us from seeing the reduction of risk-taking and drug overdose events often observed in MMT patients. The patients were required to take physical examinations prior to MMT initiation, such as blood and urine tests, chest X-rays, and electrocardiography, to check their fitness for receiving MMT. Therefore, the increase of outpatient and ED visits and hospitalizations just prior to initiating MMT shown in Fig. 1 could be attributed to these procedures. The length of hospital stay significantly decreased in both the MMT and comparison groups, probably due to the impact of the DRG payment, which shortened patients’ length of stay and decreased the intensity of care during hospitalization, on the healthcare provider's conduct under NHI in Taiwan [22, 23]. Yet, the reduced length of hospital stay in MMT patients might reflect their improved physical conditions and reduced consumption of hospital resources [30].
Our comprehensive diagrams of the differences in utilization of different medical departments before and after MMT revealed that psychiatry and infectious diseases are among the most utilized departments. This result correlates well with a cohort study of patients with heroin dependence in England, which showed that mental and behavioral disorders caused the most excess hospital admissions, and where the predominant subcategories were mental and behavioral disorders owing to alcohol, chronic obstructive pulmonary disease, head injuries, and diseases of the oral cavity [3]. A Vietnamese study demonstrated that MMT was associated with a clinical difference in health utility, and in large reductions in health care service utilization and health expenditure in HIV-positive drug users [31]. The improved utilization of the infectious disease departments of the MMT patients implied similar trends in healthcare of HIV in Taiwan. Since MMT patients usually have concomitant psychiatric disorders, such as depression [32] and insomnia [33], it was conceivable that utilization of psychiatric departments became more frequent after MMT.
There are several limitations to our study. First, outpatient services could offer prescription medication or treatments not reimbursed by NHI, and hence the expenditures would not be recorded in the NHIRD. Second, the cost of MMT and HIV treatments were covered by other government-supported grants, not NHI, so the expenditures of related healthcare could be underestimated. Third, although the insurance reimbursement policy of NHI is universal and the samples in the NHIRD covers more than 99% of the Taiwanese population, socio-economic status is still likely to affect the healthcare utilization in the study sample, with those in the lower-income group having greater odds of experiencing preventable hospitalizations and having a comorbid condition compared to the high-income group [34]. Fourth, healthcare utilization among MMT patients might vary depending on the types of insurance. Therefore, the experience of Taiwan, a region with a single-payer healthcare system [35], might not be able to apply directly to the United States, a nation with multiple healthcare payers. Fifth, comorbidity was measured on the basis of diagnoses made between 2012 and 2016, i.e., diagnoses relatively recent to the observation period, but some of the conditions considered here are long term, so there could have been under-ascertainment of some long-term comorbidities if diagnosis was prior to 2012. Last, the design of our study does not permit inferences about the direction of the association between MMT and increased healthcare utilization. All of these warrant future research to obtain more precise numbers in healthcare utilization for MMT patients.
Our results resonate with the Report of the Johns Hopkins’ Lancet Commission on Drug Policy and Health [36, 37]: policy-makers should prioritize people who use drugs in treatment for HIV and HCV, and ensure that services are adequate to safeguard access for all who need care. Humane and scientifically sound treatment for drug dependence should be available by scaling-up medication treatment for OUD.
Conclusions
MMT is associated with augmented healthcare utilization in patients with OUD. Enhanced utilization of psychiatry and infectious diseases departments after MMT admission implies that mental health problems are being resolved and communicable diseases are being treated in this socially marginalized group of patients. Policy-makers should guarantee access to healthcare by safeguarding the availability of the treatment for drug dependence.
Change history
05 May 2021
A Correction to this paper has been published: https://doi.org/10.1007/s12325-021-01712-y
References
Aldridge RW, Story A, Hwang SW, Nordentoft M, Luchenski SA, Hartwell G, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391(10117):241–50.
Volkow ND, Jones EB, Einstein EB, Wargo EM. Prevention and Treatment of Opioid Misuse and Addiction: A Review. JAMA Psychiatry. 2019;76(2):208–16.
Lewer D, Tweed EJ, Aldridge RW, Morley KI. Causes of hospital admission and mortality among 6683 people who use heroin: A cohort study comparing relative and absolute risks. Drug Alcohol Depend. 2019;204:107525.
Choi SKY, Boyle E, Cairney J, Grootendorst P, Gardner S, Collins EJ, et al. Impact of depression and recreational drug use on emergency department encounters and hospital admissions among people living with HIV in Ontario: A secondary analysis using the OHTN cohort study. PLoS ONE. 2018;13(4):e0195185-e.
Lewer D, Freer J, King E, Larney S, Degenhardt L, Tweed EJ, et al. Frequency of health-care utilization by adults who use illicit drugs: a systematic review and meta-analysis. Addiction. 2020;115(6):1011–23.
Chen IM, Huang CL-C, Yeh B-J, Chien Y-L. Health service utilization of heroin abusers: a retrospective cohort study. Addict Behav. 2015;45:281–6.
Kendall CE, Boucher LM, Mark AE, Martin A, Marshall Z, Boyd R, et al. A cohort study examining emergency department visits and hospital admissions among people who use drugs in Ottawa, Canada. Harm Reduct J. 2017;14(1):16.
Onyeka IN, Beynon CM, Ronkainen K, Tiihonen J, Föhr J, Kuikanmäki O, et al. Hospitalization in a cohort seeking treatment for illicit drug use in Finland. J Subst Abuse Treat. 2015;53:64–70.
Chen Y-C, Chen C-K, Lin S-K, Chiang S-C, Su L-W, Wang L-J. Health care service utilization and associated factors among heroin users in northern Taiwan. Addict Behav. 2013;38(11):2635–8.
Gourevitch MN, Chatterji P, Deb N, Schoenbaum EE, Turner BJ. On-site medical care in methadone maintenance: associations with health care use and expenditures. J Subst Abuse Treat. 2007;32(2):143–51.
Schwarz R, Zelenev A, Bruce RD, Altice FL. Retention on buprenorphine treatment reduces emergency department utilization, but not hospitalization, among treatment-seeking patients with opioid dependence. J Subst Abuse Treat. 2012;43(4):451–7.
Chen C-Y, Wang IA, Fang S-Y, Huang N, Tsay J-H, Chang S-H. Inadequate prenatal care utilization among women with and without methadone-treated opioid use disorders in Taiwan. Int J Drug Policy. 2019;67:1–8.
Lan CW, Lin C, Thanh DC, Li L. Drug-related stigma and access to care among people who inject drugs in Vietnam. Drug Alcohol Rev. 2018;37(3):333–9.
McCarty D, Perrin NA, Green CA, Polen MR, Leo MC, Lynch F. Methadone maintenance and the cost and utilization of health care among individuals dependent on opioids in a commercial health plan. Drug Alcohol Depend. 2010;111(3):235–40.
Lyu S-Y, Su L-W, Chen Y-MA. Effects of education on harm-reduction programmes. Lancet. 2012;379(9814):e28–30.
Lin T, Chen CH, Chou P. Effects of combination approach on harm reduction programs: the Taiwan experience. Harm Reduct J. 2016;13(1):23.
Ministry of Health and Welfare 2020 Annual Drug Addiction Treatment Expenses Subsidy Program [Available from: https://dep.mohw.gov.tw/domhaoh/cp-4097-50627-107.html.
Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. StatPearls. Treasure Island (FL): StatPearls; 2020.
Instructions for the Application and Use of the "Taiwan Illicit Drug Issue Database" of the Ministry of Health and Welfare [Available from: https://antidrug.moj.gov.tw/cp-91-6186-2.html.
Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, et al. Taiwan’s National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;11:349–58.
Lin LY, Warren-Gash C, Smeeth L, Chen PC. Data resource profile: the National Health Insurance Research Database (NHIRD). Epidemiol Health. 2018;40:e2018062.
Chien LC, Chou YJ, Huang YC, Shen YJ, Huang N. Reducing low value services in surgical inpatients in Taiwan: Does diagnosis-related group payment work? Health Policy. 2020;124(1):89–96.
Cheng S-H, Chen C-C, Tsai S-L. The impacts of DRG-based payments on health care provider behaviors under a universal coverage system: a population-based study. Health Policy. 2012;107(2–3):202–8.
Chiu SL, Chu CL, Muo CH, Chen CL, Lan SJ. Trends in glaucoma medication expenditures under universal health coverage: a national population-based longitudinal survey in Taiwan. J Ophthalmol. 2015;2015:243401.
Tsou Y-A, Lin C-C, Lai C-H, Wang C-Y, Lin C-D, Chen P-C, et al. Does Adenotonsillectomy really reduced clinic visits for pediatric upper respiratory tract infections? A national database study in Taiwan. Int J Pediatr Otorhinolaryngol. 2013;77(5):677–81.
Ko YL, Wang JW, Hsu HM, Kao CH, Lin CY. What happened to health service utilization, health care expenditures, and quality of care in patients with acute pancreatitis after implementation of global budgeting in Taiwan? Medicine (Baltimore). 2018;97(41):e12620.
Troberg K, Håkansson A, Dahlman D. Self-Rated Physical Health and Unmet Healthcare Needs among Swedish Patients in Opioid Substitution Treatment. J Addict. 2019;2019:7942145.
O’Toole J, Hambly R, Cox A-M, O’Shea B, Darker C. Methadone-maintained patients in primary care have higher rates of chronic disease and multimorbidity, and use health services more intensively than matched controls. Eur J Gen Pract. 2014;20(4):275–80.
Fang S-Y, Huang N, Lin T, Ho I-K, Chen C-Y. Health insurance coverage and healthcare utilization among infants of mothers in the national methadone maintenance treatment program in Taiwan. Drug Alcohol Depend. 2015;153:86–93.
Papi M, Pontecorvi L, Setola R. A new model for the length of stay of hospital patients. Health Care Manag Sci. 2016;19(1):58–65.
Tran BX, Nguyen LT. Impact of methadone maintenance on health utility, health care utilization and expenditure in drug users with HIV/AIDS. Int J Drug Policy. 2013;24(6):e105–10.
Yin W, Pang L, Cao X, McGoogan JM, Liu M, Zhang C, et al. Factors associated with depression and anxiety among patients attending community-based methadone maintenance treatment in China. Addiction. 2015;110(Suppl 1):51–60.
Hallinan R, Elsayed M, Espinoza D, Veillard A-S, Morley KC, Lintzeris N, et al. Insomnia and excessive daytime sleepiness in women and men receiving methadone and buprenorphine maintenance treatment. Subst Use Misuse. 2019;54(10):1589–98.
Cho HE, Wang L, Chen JS, Liu M, Kuo CF, Chung KC. Investigating the causal effect of socioeconomic status on quality of care under a universal health insurance system - a marginal structural model approach. BMC Health Serv Res. 2019;19(1):987.
Cheng TM. Reflections on the 20th anniversary of Taiwan’s single-payer National Health Insurance System. Health Aff (Millwood). 2015;34(3):502–10.
Lancet. Reforming international drug policy. Lancet. 2016;387(10026):1347.
Csete J, Kamarulzaman A, Kazatchkine M, Altice F, Balicki M, Buxton J, et al. Public health and international drug policy. Lancet. 2016;387(10026):1427–80.
Acknowledgements
We thank Department of Mental and Oral Health (DMOH), Ministry of Health and Welfare, Taipei, Taiwan for the use of their Database of Substitution Therapy. Parts of this material are based on data and information compiled and provided by DMOH. However, the analyses, conclusions, opinions and statements expressed herein are those of the authors and not necessarily those of DMOH.
Funding
This study was supported in part by Ministry of Science and Technology (MOST 104-3011-F-039-001), Ministry of Health and Welfare (M05B4352), National Health Research Institutes (NP-108-GP-05), Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212-114004), China Medical University Hospital, and China Medical University under the Higher Education Sprout Project of the Ministry of Education, Taiwan. The journal’s Rapid Service Fee was funded by the China Medical University Hospital.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Chieh-Liang Huang, I-Ju Tsai, Wen-Chi Lin, Ing-Kang Ho, Ruey-Yun Wang and Cynthia Wei-Sheng Lee declare that they have no conflict of interest.
Compliance with Ethics Guidelines
The Ethics Review Board of National Health Research Institutes in Taiwan approved this study (EC1060510-E-R1).
Data Availability
Due to constraints on the data sharing permissions of the data in Health and Welfare Data Science Center (HWDC) in Taiwan, we are not allowed to share the data for public use.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original online version of this article was revised due to update in affilation of first author.
Rights and permissions
About this article
Cite this article
Huang, CL., Tsai, IJ., Lin, WC. et al. Augmentation in Healthcare Utilization of Patients with Opioid Use Disorder After Methadone Maintenance Treatment: A Retrospective Nationwide Study. Adv Ther 38, 2908–2919 (2021). https://doi.org/10.1007/s12325-021-01633-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01633-w