Abstract
Introduction
Cutaneous melanoma is one of the most aggressive forms of skin neoplasms and represents a major cause of neoplastic or cancer death in Europe. Without adequate therapy, the 5-year survival rate is 15% when the disease metastasizes to distant organs. The objective of our study was to evaluate the status quo of the current treatment standards in stage IV melanoma and rationale for therapy decisions in Germany and Austria between January 2016 and September 2018.
Methods
In this retrospective, anonymized registry, data of male and female patients with unresectable advanced/metastatic BRAF-positive cutaneous melanoma treated in the first, second, and third line with registered substances were analyzed using descriptive statistics.
Results
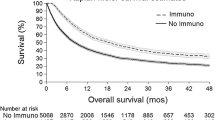
Ninety-nine patients (50.5% male) received a total of 172 treatment lines. The first (99 patients), second (56 patients), and third (17 patients) treatment lines were documented. Within the 80.8% of patients with stage IV melanoma, targeted therapy (TT) was more frequently administered as a first-line treatment than immunotherapy (IO) with checkpoint inhibitors (59.6% TT vs. 40.4% IO). Across all lines, patients received TT in 54.7% and IO in 43.0% of the cases. As targeted agents, dabrafenib plus trametinib was predominantly prescribed (72.3%), whereas the monotherapy with anti-programmed cell death protein 1 and anti-cytotoxic T lymphocyte-associated protein 4 antibodies or their combination was prescribed similarly often (50.0% vs. 47.3%). Most commonly, the treatment type was switched from TT to IO or vice versa upon disease progression. The most frequent rationales for prescribing either TT or IO were remission pressure (72.9%) or physician’s preference (45.0%), respectively. Disease progression was a more frequent cause of treatment discontinuation than undesired events.
Conclusion
Patients in Germany and Austria with unresectable advanced or metastatic BRAF-mutant melanoma predominantly receive guideline-recommended treatments. TT was more frequently administered than IO while the rationale for prescribing a specific treatment type differed between the two.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cutaneous melanoma is one of the most aggressive forms of skin cancer and represents a major cause of cancer death in Europe. |
Without adequate therapy, the 5-year survival rate is 15% when the disease metastasizes to distant organs. |
The objective of this analysis was to evaluate the status quo of the current treatment standards in stage IV melanoma and rationale for therapy decisions in Germany and Austria between January 2016 and September 2018. |
In this study, targeted therapy was more frequently administered than immunotherapy while the rationale for prescribing a specific treatment type differed between the two. |
Patients in Germany and Austria with unresectable advanced or metastatic BRAF-mutant melanoma predominantly receive guideline-recommended treatments. |
Introduction
At an incidence of approximately 100,000 new cases and approximately 22,000 deaths for both men and women in 2012, cutaneous melanoma represents the ninth leading neoplastic disease and the 14th leading cause of death due to a neoplastic or cancer disease in Europe [1]. However, these figures may represent an underestimate for new cases [2]. The 5-year survival rates range from 97% when diagnosed early at stage IA to only 15% at stage IV without adequate therapy [3]. At diagnosis, approximately 10–20% of the patients present with advanced or metastatic melanoma [4, 5] and around 45% of melanoma harbor an activating mutation of the BRAF gene [6]. The treatment of advanced or metastatic melanoma has rapidly evolved during recent years with the introduction of multiple new drugs of two predominant treatment types—immunotherapy (IO) and targeted therapy (TT). Immunity, responsible for adequate biological defenses to fight infection and cancer [7], is controlled by a complex regulatory network to maintain the sensitive balance between defense and tolerance [8] to efficiently eliminate invading pathogens [9] and at the same time to avoid the development of chronic inflammation, such as autoimmune reactions [7, 9]. This balance of the immune system is regulated by co-stimulatory and co-inhibitory molecules, known as immune checkpoints [7, 8]. One of the most important inhibitory immune checkpoints is programmed cell death protein 1 (PD-1) [8]. The PD-1 pathway downregulates effector T cells in their immune response that results in immune suppression [10]. The activation of the PD-1 signal pathway is one of the main factors of cancer immune escape in humans [8]. Cytotoxic T lymphocyte-associated protein 4 (CTLA4) is also an inhibitory receptor expressed constitutively on CD4+CD25+ T regulatory lymphocytes and transiently on activated CD4+ and CD8+ T lymphocytes promoting durable anergy in immune cells [11]. Immunotherapy aims at overcoming or circumventing the immune evasion mechanisms of tumor cells with inhibitory antibodies blocking immune checkpoints. Representatives among PD-1 inhibitors are pembrolizumab [Pem] and nivolumab [Niv] and among CTLA4 inhibitors substances such as ipilimumab [Ipi]. The BRAF gene, one of three isoforms of the rapidly accelerated fibrosarcoma (RAF) kinase family, encodes the serine/threonine-protein kinase B-RAF. Along with its downstream molecules, mitogen-activated protein kinase kinase (MAP2K or MEK) and extracellular signal-regulated kinase (ERK), the RAF gene family constitutes the classic mitogen-activated protein kinase (MAPK) signaling pathway [12]. This Raf/MEK/ERK kinase signal pathway is highly involved in cell proliferation, differentiation, and tumorigenesis [13]. Accordingly, mutations of B-Raf and predominantly V600E in exon 15 [14] have been detected in a variety of cancers including melanoma [15]. In the case of BRAFV600-mutant melanoma, targeted therapy can be administered to directly act on the altered protein and the activated MAPK signaling cascade with the combination of BRAF plus MEK inhibitors, namely vemurafenib + cobimetinib (Vem + Cob), dabrafenib + trametinib (Dab + Tra), and encorafenib + binimetinib (Enc + Bin) [2, 16].
Most therapeutic options currently recommended for first-line treatment of advanced or metastatic melanoma have been approved by the European Medicines Agency in 2015 and 2016 (Fig. 1).
Study Aim and Purpose
This analysis depicts the status quo of the current treatment standards in stage IV melanoma and summarizes the rationales for therapy decisions in Germany and Austria in the era when modern treatment options were available.
Methods
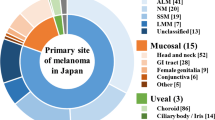
In this retrospective, cross-sectional documentation based on anonymized data at nine specialized skin cancer centers in Germany and one center in Austria, data of male or female patients, at least 18 years of age, with histologically confirmed unresectable advanced or metastatic BRAFV600E/K-positive malignant cutaneous melanoma (stage IIIB/C or IV) [17] treated between January 2016 and September 2018 in the first-, second-, and third-line setting with substances registered in the European Union at the time of treatment was collected retrospectively and analyzed using descriptive statistics. The key exclusion criteria were (1) non-cutaneous melanoma, (2) other stage III–IV malignancies, (3) prior/concomitant systemic treatment of any other malignancy, (4) participating in a clinical trial or an early access program while being treated in the first-, second-, and third-line setting.
Data from participating centers were combined, analyzed, summarized, and reported. Data sets included demographic and baseline characteristics, efficiency and safety observations, and measurements using descriptive statistics (frequency, mean, standard deviation, median, minimum, maximum, 25% quartile and 75% quartile—quantitative data) and contingency tables (absolute and relative frequencies—qualitative data) as appropriate. The treatments administered at first, second, and third line were analyzed in toto, by treatment line and by treatment type (checkpoint inhibition, targeted therapy, chemotherapy, others) together with the respective reasons. The safety parameters were analyzed by treatment line (overall and by treatment type). Further details are specified in the statistical analysis plan.
An informed consent process was not implemented in this anonymized, retrospective data analysis. The study was approved by the ethics committee (EC) of the University Hospital Regensburg, Germany (EC review number 18-935-101) and the Medical University of Graz, Austria (EC review number 30-269 ex 17/18).
Results
Patient Population
Treatment sequences of 100 patients were documented. Of these, 99 patients met all inclusion and none of the exclusion criteria and had at least one line of melanoma therapy. Fifty-six patients continued to be treated in a second-line setting and 17 patients received a third-line treatment, accounting for 172 treatment lines in total. At the start of first-line treatment, 50.5% were male and 49.5% were female. The mean age for both genders was 62.1 years at this time. Between 80.8% and 89.3% of the patients presented with stage IV melanoma at the start of each treatment line. In all treatment lines, between 35.3% and 43.4% of the patients had normal lactate dehydrogenase (LDH) and in 39.4–55.4% of the patients LDH was elevated at the start of each treatment line. For the key patients’ characteristics at the time of initiation of the first-line treatment, see Table 1.
Treatment
TT was more frequently administered as a first-line treatment than modern IO (59.6% TT vs. 40.4% IO). Across all lines, patients received TT in 54.7% and IO in 43.0% of the cases, whereas chemotherapy was only administered in a few cases (1.7%). The overall absolute frequencies of the active components used are depicted in Fig. 2 (presented excluding chemotherapy data). BRAF inhibitors were administered as a monotherapy only in 3 out of 94 cases; whereas in all other patients, combinations of BRAF and MEK inhibitors were administered. Within the group treated with TT, Dab + Tra was the therapy of choice when compared to Vem + Cob (72.3% vs. 24.5%). Patients treated with IO received a combination treatment with Ipi plus either Niv or Pem (47.3%) or IO monotherapy regimens (50.0%) and in a few cases T-VEC (2.7%). The treatment sequences for each patient are shown in Fig. 3. Most commonly, the treatment type was switched either from TT to IO or vice versa. In a total of 13 cases, patients received TT twice; however, in the seven out of these 13 patients having received consecutive TT, the active substances were mostly switched, whereas the six patients rechallenged with TT after second-line IO mainly received the same combination treatment again (data not shown).
Treatment sequences (first-line to second-line to third-line treatment) for all patients. Each patient is represented by a single colored line (or by a single colored dot in case only the first line was administered). Accordingly, the treatment sequences of each patient can be followed starting with the first-line treatment (on the left) and moving forward to the right to the subsequent treatment line(s), i.e., to the second line in the middle and to the third line on the right, if applicable. The more patients received the same treatment types consecutively the more lines are depicted, hence highlighting the absolute number of patients being treated with the same treatment sequence in a row
According to the physician’s assessment, the most frequent reason for choosing a certain treatment was high remission pressure (50.6%; i.e., rapid tumor progression, tumor load and location, and elevated LDH) followed by the physician’s preferences for the prescribed treatment (34.3%). The main reasons differed between the two treatment types (TT and IO) with remission pressure being named most often for TT (72.9%) and physician’s preference for IO (45.0%). Details for the first-line treatments are outlined in Table 2.
The main reasons for prescribing a specific drug are outlined in Table 3. The treatment choice between Dab + Tra vs. Vem + Cob was mainly driven by the toxicity profile, tolerability, and physician’s preference. The combination of Ipi + Niv was mainly selected because it was the only registered option, whereas the monotherapies were selected on the basis of physician’s preference, tolerability, or administration interval (3-week-/2-week regimen).
Treatment Discontinuation
Most treatments were discontinued by the time of data documentation. Across all treatment lines, the predominant reason for discontinuation was the development of disease progression followed mainly by toxicities (Table 4). In particular, the combination regimen Ipi + Niv treatment was discontinued in around one-third of the cases as a result of toxicities (Table 5). The specific toxicities leading to treatment discontinuation by drug(s) are listed in Table 6. For TT, the events were mostly specific for the active substances while exclusively inflammatory events were described for IO.
Discussion
In this study we examined the real-world treatment of unresectable advanced or metastatic BRAFV600E/K-positive malignant cutaneous melanoma in patients treated in nine specialized skin cancer centers in Germany and one center in Austria. The aim of our data analysis was to better understand the treatment landscape and the decision-making process in Germany and Austria. The results of this study include information on patient profiles, treatment patterns, and outcomes of patients treated in the real-world setting.
Almost exclusively, modern treatments were administered as chemotherapy was chosen only in rare cases. In most patients treated with modern oncological regimens, a higher number of patients were treated with TT compared to IO, reflecting the positive BRAF-mutational status as selection criterion. However, the administration of BRAF inhibitors in monotherapy occurred in single cases only. For patients treated with TTs, the combination of Dab + Tra was predominantly prescribed, followed by the combination of Vem + Cob. The combination Enc + Bin has not been registered in the observed time period. In contrast, combination therapy and monotherapy were administered in a more balanced fashion in the IO group.
Our data suggests that the main driver for administering TTs was the need of a rapid, reliable, and sustained remission (remission pressure) compared to the IO group. Results from several phase III trials have demonstrated that molecules targeting BRAF and MEK kinases achieved (BRAF monotherapy, as well as combined BRAF and MEK inhibition) higher overall response rates and shorter response times than modern immunotherapy along with a favorable safety profile [18]. In the IO group, the treatment choices were influenced by the treating physician’s preferences. Favorable overall survival data of the combination regimen Ipi + Niv compared to TT may have had an impact on decision-making [19, 20]. Taken together, our data underline that in specialized skin cancer centers in Germany and Austria, modern treatment options are the standard of care.
For modern immunotherapy, immune-related adverse reactions represent the leading cause for treatment discontinuation. In the absence of other causes, considering the mode of action of IO therapies, the correlation between such immune-related toxicities and the treatment with IO must be assumed. TTs, however, predominantly showed substance-specific toxicities, such as pyrexia or rash. The availability of numerous combinations makes switching to an alternative TT combination (with intermediate or subsequent IO treatment) a common therapeutic strategy in cases where specific toxicities required treatment discontinuation. Our data showing more frequent cases of rechallenge treatment sequences with TT underline that this approach is feasible and not uncommon. The registration of encorafenib and binimetinib is associated with a distinct toxicity profile and thus leads to yet another option for future patients with melanoma, especially after disease progression or treatment discontinuation due to adverse events. Additionally, combinations and the sequential use of TTs and IOs are currently being investigated.
Methodological Limitations
The underlying study included efficiency endpoints whose interpretation is troubled by a series of limitations. Only patients who had completed at least one treatment line, which had been started after January 2016 were eligible for inclusion, therefore heavily biasing the treatment duration, time-to-progression, and response rates. In addition, the documentation period ended in March 2018. Another bias is introduced by the nature of this study with its uncontrolled, open design, non-standardized treatment allocations and conditions, as well as its non-standardized, observational character in terms of efficacy follow-up and the limited number of events, in particular in the group of patients treated in the third-line setting. To conclude, efficiency cannot be assessed adequately. These data are hence not shown here.
Conclusion
Patients in Germany and Austria with unresectable advanced or metastatic BRAF-mutant melanoma predominantly receive guideline-recommended treatments. In this study, TT was more frequently administered than IO while the reasons for prescribing a specific treatment type differed between the two.
References
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374–403.
Coit DG, Thompson JA, Albertini MR, et al. NCCN clinical practice guidelines in oncology (NCCN Guidelines): cutaneous melanoma. Version 1.2020. https://www.nccn.org/professionals/physician_gls/pdf/cutaneous_melanoma.pdf. Accessed 2 Apr 2020.
Long GV, Menzies AM, Nagrial AM, et al. Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol. 2011;29(10):1239–46.
Bericht zum Krebsgeschehen in Deutschland. 2016. https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebsgeschehen/Krebsgeschehen_node.html. Accessed 2 Apr 2020.
National Cancer Institute. SEER Cancer Statistics Review 1975-2014. 2020. https://surveillance.cancer.gov/delay/. Accessed 2 Apr 2020.
Garbe C, Amaral T, Peris K, et al. European consensus-based interdisciplinary guideline for melanoma. Part 1: diagnostics—update 2019. Eur J Cancer. 2020;126:141–58.
Huang C, Zhu HX, Yao Y, et al. Immune checkpoint molecules. Possible future therapeutic implications in autoimmune diseases. J Autoimmun. 2019;104:102333.
Chamoto K, Al-Habsi M, Honjo T. Role of PD-1 in Immunity and diseases. Curr Top Microbiol Immunol. 2017;410:75–977.
Subleski JJ, Wiltrout RH, Weiss JM. Application of tissue-specific NK and NKT cell activity for tumor immunotherapy. J Autoimmun. 2009;33(3–4):275–81.
Zhu X, Lang J. Soluble PD-1 and PD-L1: predictive and prognostic significance in cancer. Oncotarget. 2017;8(57):97671–822.
Kailashiya V, Sharma HB, Kailashiya J. Role of CTLA4 A49G polymorphism in systemic lupus erythematosus and its geographical distribution. J Clin Pathol. 2019;72(10):659–62.
Pratilas CA, Solit DB. Targeting the mitogen-activated protein kinase pathway: physiological feedback and drug response. Clin Cancer Res. 2010;16(13):3329–34.
Roskoski R Jr. RAF protein-serine/threonine kinases: structure and regulation. Biochem Biophys Res Commun. 2010;399(3):313–7.
Kumar R, Angelini S, Czene K, et al. BRAF mutations in metastatic melanoma: a possible association with clinical outcome. Clin Cancer Res. 2003;9(9):3362–8.
Huang T, Karsy M, Zhuge J, Zhong M, Liu D. B-Raf and the inhibitors: from bench to bedside. J Hematol Oncol. 2013;6:30.
Michielin O, van Akkooi ACJ, Ascierto PA, Dummer R, Keilholz U. Cutaneous melanoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30:1884–901.
Gershenwald JE, Scolyer RA, Hess KR, et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. 2020. https://acsjournals.onlinelibrary.wiley.com/doi/epdf/10.3322/caac.21409. Accessed 17 Apr 2020.
Silva IP, Long GV. Systemic therapy in advanced melanoma: integrating targeted therapy and immunotherapy into clinical practice. Curr Opin Oncol. 2017;29(6):484–92.
Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2019;381(16):1535–46.
Robert C, Grob JJ, Stroyakovskiy D, et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N Engl J Med. 2019;381(7):626–36.
Acknowledgements
Funding
Sponsorship for this project was funded by Pierre Fabre Pharma GmbH (Freiburg, Germany). Pierre Fabre Pharma GmbH also provided financial support for data analysis and medical writing as well as for Advances in therapy’s Rapid Service Fee.
Medical Writing, Editorial, and Other Assistance
The authors would like to acknowledge editorial support provided by Andreas Zähringer, Freiburg. We would also like to express our gratitude to Monika Schwager (Winicker Norimed GmbH, Nuremberg, Germany) for providing the statistical support in this project. Support for this assistance was funded by Pierre Fabre GmbH.
Authorship
The authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
This project and the analysis were designed and conducted by B. Edlich and S. Haferkamp. All named authors participated in the development of this manuscript and in the decision to submit this manuscript for publication.
Disclosures
Sebastian Haferkamp is on the advisory board or has received honoraria and travel support from Amgen, Bristol Myers Squibb, Merck Sharp and Dohme, Novartis, Pierre Fabre, Roche, and Sanofi outside the submitted work. Mareike Alter has received an honorarium for speakers and consulting roles from Novartis, Roche, AbbVie, BMS, MSD, Merck, Pfizer, Sanofi, Sun-Pharma, and Takeda. Dirk Debus has received lecture, advisory and moderation fees as well as travel and/or participation fees for training/congresses from the following companies: Amgen, BMS, MSD, Novartis, Pierre Fabre, Roche, Sanofi. Bastian Schilling reported grants and personal fees from BMS, grants and personal fees from MSD Sharp & Dohme, personal fees from Incyte, personal fees from Novartis, personal fees from Roche, grants and personal fees from Pierre Fabre Pharmaceuticals, personal fees from Pfizer, personal fees from AMGEN, outside the submitted work. Patrick Terheyden reported speaker’s honoraria from BMS, Novartis, MSD, Pierre Fabre, CureVac, Kyowa Kirin, and Roche, consultant’s honoraria from BMS, Novartis, Pierre Fabre, Merck Serono, Kyowa Kirin, Sanofi, and Roche and travel support from MBS and Pierre Fabre outside the submitted work. Jochen Utikal is on the advisory board or has received honoraria and travel support from Amgen, Bristol Myers Squibb, GSK, LeoPharma, Merck Sharp and Dohme, Novartis, Pierre Fabre, Roche, and Sanofi outside the submitted work. Michael M. Sachse has received speaker honoraria from Roche Pharma, MSD Sharp & Dohme, Novartis Pharma, and Sanofi-Aventis. Thomas Haalck has received a speaker’s honorarium from Pierre Fabre outside the submitted work. Ingrid Wolf has received a speaker’s honorarium form BMS, MSD, Novartis, and Pierre Fabre outside the submitted work. These authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. Andreas Pinter has nothing to disclose.
Compliance with Ethics Guidelines
An informed consent process was not implemented in this anonymized, retrospective data analysis. The study was approved by the ethics committee of the University Hospital Regensburg, Germany (EC review number 18-935-101) and the Medical University of Graz, Austria (EC review number 30-269 ex 17/18).
Data Availability
The datasets generated during and or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request. The anonymized data from the clinical trial is archived according to the ICH-GCP requirements at Pierre Fabre Pharma GmbH, Freiburg, Germany and will not be made public.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12571082.
Rights and permissions
About this article
Cite this article
Haferkamp, S., Alter, M., Debus, D. et al. Patients with BRAF-Mutant Advanced/Metastatic Melanoma: Original Research on the Treatment Reality in Germany and Austria in the Era of Choice. Adv Ther 37, 3619–3629 (2020). https://doi.org/10.1007/s12325-020-01430-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01430-x