Abstract
Introduction
Wherever access to direct-acting antiviral agents is restricted, dual peginterferon/ribavirin (PegIFN/RBV) therapy remains an option for treatment of hepatitis C virus (HCV) genotype 4 (GT4) infection, which predominates in the Middle East and Sub-Saharan Africa. Our goal was to develop a baseline scoring system to identify GT4-infected patients with a low or high probability of achieving a sustained virologic response (SVR) with PegIFN alfa-2a/RBV using data from two large cohort studies.
Methods
Associations between baseline characteristics and SVR were explored by generalized additive models and multiple logistic regression analysis to develop a predictive model, which was then checked by bootstrapping. The score comprised four factors with points assigned thus: age ≤40, 3 points; >40 but ≤55, 2 points; alanine aminotransferase ≤1 or >3× the upper limit of normal, 1 point; no cirrhosis, 1 point; HCV RNA <50,000 IU/mL, 2 points; 50,000 to <400,000 IU/mL, 1 point. The values for a given patient are summed to produce a score from 0 to 7 where higher scores indicate higher chances of SVR.
Results
Among the 459 patients, 28 (6%), 50 (11%), 92 (20%), 121 (26%), 103 (22%), and 65 (14%) patients had scores of 0–1, 2, 3, 4, 5, and 6–7, respectively, with respective SVR rates of 11%, 28%, 50%, 57%, 63%, and 83%. Relapse rates decreased with increasing prediction score (80%, 39%, 15%, 19%, 5%, and 7%, respectively). SVR rates were consistently higher in Caucasian than Black patients and in patients with a rapid virologic response HCV RNA <50 IU/mL at week 4); however, the trend toward higher SVR rates with increasing score remained apparent in each subgroup.
Conclusion
In conclusion, a simple scoring system can be used to identify GT4-infected patients with a high probability of achieving an SVR with PegIFN alfa-2a/RBV.
Funding
F. Hoffmann-La Roche Ltd.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis C virus (HCV) is a global health problem, with an estimated 184 million people infected worldwide [1]. Of these, it is estimated that 170 million are chronically infected and at risk of serious complications including decompensated cirrhosis and hepatocellular carcinoma [1]. Worldwide, more than 700,000 deaths are attributed to HCV-related cirrhosis or liver cancer every year [2]. HCV genotype 4 (GT4) infection is the predominant cause of chronic hepatitis C (CHC) in the Middle East, and Sub-Saharan Africa where it represents a majority of HCV infections [3]. In Egypt, the country with the highest HCV prevalence worldwide (15%), HCV GT4 is present in 90% of all cases [4, 5]. Recently, HCV GT4 has spread to Southern Europe through immigration [3]. Patients with HCV GT4 infection are an understudied group and have generally been underrepresented in large international clinical trials [6].
According to guidelines issued by the European Association for the Study of the Liver (EASL), several interferon-free and interferon-based treatment options are available for patients with HCV GT4 infection [6]. Interferon-free options include sofosbuvir/ledipasvir with or without ribavirin (RBV); ombitasvir/paritaprevir/ritonavir and RBV; sofosbuvir plus simeprevir with or without RBV; or sofosbuvir plus daclatasvir with or without RBV [6–8]. Interferon-based regimens include either sofosbuvir or simeprevir administered in combination with peginterferon (PegIFN)/(RBV) [6, 9–11]. The EASL guidelines recognize that direct-acting antiviral agents are not broadly accessible to patients in some settings, in which case the recommended therapy is dual PegIFN/RBV combination therapy [6]. Guidelines issued by the American Association for the Study of Liver Diseases (AASLD) are consistent with the EASL guidelines, although AASLD no longer recommends the use of dual PegIFN/RBV in the US [12]. Direct-acting antivirals are not readily available to all patients, meaning that PegIFN/RBV may be their only treatment option.
Few HCV GT4-infected patients were enrolled in registration trials for PegIFN alfa/RBV [13–15]. A comprehensive review of trials in GT4 patients, most of which were conducted in the Middle East, found that sustained virologic response (SVR) rates have ranged from 38% to 87% [16]. The SVR rate of 87% was obtained in HCV GT4-infected patients with a rapid virologic response (RVR), defined as undetectable HCV RNA at week 4 of treatment [17]. Consistent with this finding, an SVR rate of 86% was obtained in Egyptian patients with HCV GT4 infection who achieved an RVR [18]. In a study performed in France, an RVR was obtained in 15 out of 59 patients with HCV GT4 infection and was a strong predictor of SVR [19]. In the French study, 82%, 47%, and 29% of patients with host IL28B rs12979860 CC, CT, and TT genotypes, respectively, achieved an SVR [19].
The use of patient baseline factors in prognosis is widespread in medicine, and scoring systems are commonly used to predict outcome and drive treatment decisions, for example, the CHADS system in stroke prevention [20]. In the setting of CHC, a wide range of baseline host and viral factors and on-treatment predictors have been shown to be associated with SVR [21]. The ability to predict which patients are most likely to achieve an SVR with PegIFN alfa-2a/RBV on the basis of patient characteristics alone would be extremely useful in guiding treatment decisions. Moreover, the combination of a baseline prediction tool and on-treatment predictors such as RVR would allow clinicians to optimize treatment outcomes by preferentially initiating treatment in patients with favorable baseline profiles and continuing treatment only in those most likely to respond, while avoiding exposure to potential adverse events in those unlikely to achieve an SVR.
The objective of this analysis was to develop a simple and easy-to-use scoring system specifically for clinical encounters with HCV GT4-infected patients that uses readily available baseline characteristics to estimate an individual patient’s chance of responding to treatment with PegIFN alfa-2a/RBV.
Methods
This was a pooled analysis of data from patients with CHC and quantifiable serum HCV RNA levels before initiation of treatment (≥50 IU/mL) who received dual PegIFN/RBV therapy in two large, international cohort studies, PROPHESYS (ClinicalTrials.gov Identifiers: NCT01070550, NCT01066793, and NCT01066819) [22] and GUARD-C (ClinicalTrials.gov Identifier: NCT01344889) [23]. PROPHESYS and GUARD-C were conducted in 19 and 25 different countries, respectively, in Europe, Asia, North Africa and the Middle East, and South America. The present analysis included adult Caucasian or Black patients with CHC and HCV GT4 infection who were assigned to an initial treatment duration of 48 weeks with PegIFN alfa-2a (PEGASYS®, Roche, Basel, Switzerland) 180 µg once weekly plus RBV (COPEGUS®, Roche) at either a fixed dose of 800 mg/day, or a weight-based dose of 1000/1200 mg/day according to the local label. Patients with compensated cirrhosis were enrolled and treated in both PROPHESYS and GUARD-C and thus were included in this analysis. For the purposes of the present analysis, the term cirrhosis refers collectively to frank cirrhosis and bridging fibrosis (transition to cirrhosis).
Patients with contraindications to PegIFN alfa-2a/RBV, previous interferon-based treatment, with end-stage renal disease and/or recipients of major organ transplants were excluded from the present analysis, as were patients co-infected with hepatitis B virus or human immunodeficiency virus, and any patients who had received both PegIFN alfa-2a and PegIFN alfa-2b.
The original studies were conducted in accordance with the Declaration of Helsinki and the protocols were approved by the institutional review board/local independent ethics committee at each center [22, 23]. All patients provided informed written consent.
Outcomes
The primary outcome of interest was SVR, defined as HCV RNA <50 IU/mL (by polymerase chain reaction) after 24 weeks of untreated follow-up (≥140 days after last dose of treatment). Patients were excluded from the statistical analysis if they had an end of treatment (EOT) response (HCV RNA <50 IU/mL at EOT) and no record of relapse, but were missing an HCV RNA measurement ≥140 days after EOT for reasons not related to efficacy or safety. RVR was defined as undetectable HCV RNA by week 4 of treatment. Relapse was defined as detectable HCV RNA (≥50 IU/mL) during untreated follow-up in a patient with a confirmed EOT response. Only patients with an EOT response were included in calculations of relapse.
Development of Baseline Predictor Score
Baseline factors considered in the analyses included: age, gender, race (Black vs. Caucasian), body mass index (BMI), alanine aminotransferase (ALT) ratio (ALT divided by the ULN for the local laboratory), hepatic fibrosis status (cirrhosis vs. no cirrhosis), platelet count, HCV RNA level, and assigned RBV dose. Generalized additive models (GAMs) were used to explore the relationship between each of the continuous variables and SVR to identify appropriate cutoffs to be used in a logistic regression analysis. The values of each factor were grouped by deciles and the empirical probabilities for SVR at the midpoints of the deciles were included in GAM plots. Associations between the categorized baseline factors and SVR were then explored by univariate logistic regression (ULR) analyses. All baseline factors with a Wald Chi-square P value of 0.25 were selected for multiple logistic regression (MLR) analyses using a backward elimination process to identify independent predictors of SVR. A Wald Chi-square P value <0.05 was required for inclusion of a baseline variable in the final model. Internal validation procedures [24] were applied to assess the stability of the selected model using bootstrap resampling methods. A variable was considered to be a reliable predictor if it was selected in at least 50% of 1000 bootstrapped samples with replacement. In addition, the discrimination of the model was quantified by calculating the area under the receiver operating characteristics curve (ROC-AUC) and the optimism-corrected ROC-AUCs were determined using the bootstrap samples. Finally, the Hosmer–Lemeshow test was applied to assess the goodness of fit test of the final model. Points were then assigned for each baseline characteristic in the MLR model based on the magnitude of the parameter estimates in the final logistic regression model in agreement with the methods proposed by Sullivan et al. [25]. Although race was not significantly associated with SVR in the analysis SVR rates were examined separately in Black and Caucasian patients because of the well-established differences between these groups when treated with interferon-based therapies [26–30].
The statistical analyses were conducted with SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Patients
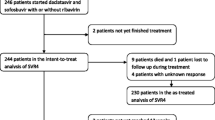
A total of 495 treatment-naive patients with HCV GT4 infection were assigned to 48 weeks of therapy with PegIFN alfa-2a 180 µg/week plus RBV 800–1200 mg/day were included in the analysis (Fig. 1). Among these 495 patients, the mean age was 45 years, 68.7% were male, 81.4% were Caucasian, 18.6% were Black, and 19.6% had cirrhosis (Table 1). HCV GT4 subtype was determined in 161 patients (32.5%), among whom subtype 4a was most common (Table 1). Patients included in the analysis came from 22 different countries (Table S1 in the supplementary material), with most patients coming from Europe (63%) the Middle East (21%), and Egypt (16%).
Graphic Analysis and Selection of Cutoffs
The GAM plots visualizing the relationship between SVR and continuous variables showed that SVR rates increased with lower age, BMI, and HCV RNA level, and with higher platelet count, but that there was no clear association between SVR and ALT ratio (Figure S1–S5 in the supplementary material). Based on this analysis, the following baseline factors and cutoffs were considered in further analyses; age ≤40, 40 to ≤55, and >55 years; BMI ≤25 and >25 kg/m2; platelet count <185 and ≥185 × 109/mL; and HCV RNA level <50,000, 50,000 to <400,000, and ≥400,000 IU/mL.
ALT ratio was dichotomized in an unusual manner (≤1.0 or >3.0 and >1.0 but ≤3.0), because the GAM analysis showed that SVR rates were highest in patients with normal ALT ratios (≤1.0) and increased in those with ALT ratios >3.0.
ULR Analysis to Identify Baseline Predictive Factors
Associations between SVR and dichotomous (gender, race, hepatic fibrosis status and planned RBV dose) and continuous baseline factors (age, ALT ratio, platelet count, and HCV RNA level using the categories specified above) were explored by ULR analysis. As a result of this analysis (Table 2), gender and planned RBV dose were rejected (P ≥ 0.25) from further model selection.
SVR rates were significantly higher in younger patients (P < 0.0001), Caucasian patients (P = 0.0212), patients with either a normal ALT ratio (<1.0) or an ALT ratio >3.0 (P = 0.0127), patients without cirrhosis (P = 0.0001), higher platelet counts (P = 0.0013), and lower HCV RNA levels (P = 0.0003) at baseline (Fig. 2). No differences in SVR rates were observed for the dichotomous variables gender (P = 0.8104) or planned RBV dose (P = 0.9265), while the difference in SVR rates for the BMI categories was borderline (P = 0.0877).
MLR Analysis of SVR
Next, an MLR analysis was performed with backward selection using a P value of 0.05 including all variables in Table 2 that had a P value <0.25 in the ULR analysis. The following independent factors were retained in the model and identified as positive predictors of SVR: younger age (P < 0.0001), ALT ratio ≤1 or >3 (P = 0.0146), absence of cirrhosis (P = 0.0073), and lower HCV RNA level (P = 0.0046) (Fig. 3). Race, BMI, and platelet count were excluded during the selection procedure. The stability of the model was supported by the bootstrap validation step. Age, HCV RNA, ALT ratio and cirrhosis stage were selected in 97%, 77%, 71% and 66% of the 1000 bootstrap samples, while platelets (40%), race (15%) and BMI class (9%) were selected in fewer than 50% of the samples. The ROC-AUC was 0.698, while the optimism-corrected ROC-AUC was 0.672.
Multivariate logistic regression analysis. ALT alanine aminotransferase; ALT ratio ALT divided by ULN for the local laboratory; CI confidence intervals; ULN upper limit of normal. Asterisk indicates Wald Chi-square test for each regression coefficient; hash indicates Wald Chi-square test for each variable; AUC ROC = 0.698, Hosmer–Lemeshow goodness of fit test: P = 0.4556
The scoring system was then developed by assigning a value of 0 to the reference value for each predictive factor (e.g., age >55 years; HCV RNA ≥400,000 IU/mL; see Table 3). Thereafter, points were assigned in accordance with the size of the regression coefficient and using 0.5 as the unit for one point. For example, the regression coefficient for age ≤40 is 1.6392 and when divided by 0.5 the result is 3.2784 (this value was then rounded to 3). The points assigned for each of the variables were summed according to the baseline characteristics for an individual patient, resulting in possible prediction scores ranging from 0 to 7, where patients with higher prediction scores have a higher chance of achieving an SVR. The formula for estimating the probability for SVR based on the final logistic regression model is shown in the Supplementary material (Supplementary prediction formula).
SVR and Relapse According to Prediction Score
The distribution of prediction scores in the 459 patients with sufficient data to calculate a baseline score was as follows: 0–1 points (n = 28, 6.1%); 2 points: (n = 50, 10.9%); 3 (n = 92, 20.0%); 4 (n = 121, 26.4%); 5 points (n = 103, 22.4%); 6–7 points (n = 65, 14.2%).
Among these patients, the SVR rate was 54.7% (251/459) overall, and among Caucasian and Black patients the overall SVR rates were 57.8% (215/372) and 41.4% (36/87), respectively.
SVR rates increased with increasing prediction score and ranged from 10.7% in patients with a baseline prediction score of 0–1 to 83.1% in patients with a score of 6 or 7 (Fig. 4a; Table 4). Patients with scores of at least 5 (n = 168, 37% of all patients) had considerably higher SVR rates (70.8%) than the overall population (54.7%).
a SVR by baseline score; b RVR by baseline score; c SVR in Caucasian patients with and without an RVR, by baseline score; d SVR in black patients with and without an RVR, by baseline score; e SVR in cirrhotic and non-cirrhotic patients. Patients with missing scores omitted (Caucasian n = 31, black; n = 5 non-cirrhotic n = 11). SVR sustained virologic response; RVR rapid virologic response
Consistent with the increase in SVR rates with increasing baseline prediction score, relapse rates decreased with increasing baseline prediction score and were highest among those with a score of 0–1 (80%) and lowest among those with a score of 5 (4.5%) and 6–7 (6.9%) (Table 4).
The overall SVR rate was higher in Caucasian than in Black patients. However, the proportion of patients with lower scores (0–3) was considerably higher in Black (51/87, 59%) than in Caucasian patients (119/372, 32%), which might explain, in part, the lower overall SVR rate in Black patients. Similar trends in SVR rates were evident within the Caucasian and Black subgroups, with numerically higher SVR rates achieved in Caucasian patients when compared with Black patients with the same baseline scores (Fig. 4a).
HCV GT4 subtype was unknown for most patients; however, 92 patients with HCV subtype 4a infection had prediction scores. In patients with baseline predictions scores of 0–1, 2, 3, 4, and 5, SVR rates were 10%, 38.1%, 57.1%, 66.7%, and 85.7%, respectively. No patient with a known HCV GT4a subtype had a score of 6 or 7.
RVR rates increased with increasing baseline prediction score, overall and among Caucasian patients (Fig. 4b). A similar trend was apparent in Black patients (Fig. 4b). Achievement of an RVR was associated with an overall SVR rate of 82.2% (106/129) among Caucasian patients (Fig. 4c) and 84.6% (22/26) among Black patients (Fig. 4d). In contrast, overall SVR rates were lower among Caucasian patients without an RVR (46.5%, 107/230) and among Black patients without an RVR (22.0%, 13/59).
Among Caucasian patients with an RVR, SVR rates were 66.7% in those with a baseline score of 0–1 and exceeded 80% among those with baseline scores of 4 or higher (Fig. 4c). SVR rates also increased with increasing baseline prediction score among those without an RVR, although they tended to be lower than in those who achieved an RVR (Fig. 4c). Among the 54 Caucasian patients with a baseline score of 6–7, all but seven achieved an SVR, including 32 of 37 patients with an RVR and 15 of 17 patients without an RVR (Fig. 4c). Among Black patients SVR rates were generally higher in patients with than without an RVR, although the number of patients within each category tended to be low (Fig. 4d).
SVR rates increased with increasing baseline score in patients with and without cirrhosis, although only seven patients with cirrhosis had a prediction score of 5 and none had a score of 6 or 7 (Fig. 4e).
Discussion
The results of this analysis indicate that a simple and easy-to-implement baseline scoring system can be used to identify HCV GT4-infected patients who are highly likely to achieve an SVR with dual PegIFN alfa-2a/RBV therapy. The scoring system comprises four readily available patient demographic and disease characteristics, including age, ALT ratio, hepatic fibrosis status, and serum HCV RNA level, and can be easily incorporated into routine patient encounters. Points were assigned according to the magnitude of the regression coefficient in the multivariate analysis. The individual values for a given patient are summed to produce a score ranging from 0 to 7 where higher scores indicate higher chances of SVR.
Of note, younger age (≤40 years) was the strongest predictor of SVR in the present analysis. This is consistent with other MLR analyses that have found younger age to be significantly associated with SVR [31, 32]. The association between younger age and higher SVR rates shows that if interferon-based therapy is a consideration, it is best to treat patients now rather than waiting because the likelihood of achieving an SVR will only decrease as the patient ages. Other factors that predicted SVR included either a normal ALT ratio or an ALT ratio >3 × ULN, the absence of advanced fibrosis (transition to cirrhosis or frank cirrhosis), and a low HCV RNA level. It is important to note that patients with the highest chance of achieving an SVR, namely younger patients and those without advanced fibrosis, also tend to tolerate PegIFN/RBV treatment better than older patients and those with advanced fibrosis [23, 33]. Thus, the benefit:risk ratio for PegIFN/RBV treatment is highest in younger patients without advanced fibrosis.
Achievement of an RVR is a much stronger predictor of SVR after treatment with PegIFN alfa-2a/RBV than any baseline characteristic [31]. The consistently high SVR rates found in this analysis for patients with an RVR, regardless of baseline score, confirm previous results and show that baseline predictors can and should be used in combination with RVR (if available).
We envisage that the tool would be used to select patients with a reasonable chance of achieving an SVR and alternatively to identify patients with a low chance of achieving an SVR. For example, a clinician may choose to offer therapy to patients with a minimum baseline prediction score and to encourage patients with lower baseline scores to defer treatment until therapy with direct-acting antivirals (DAAs) becomes more accessible. The threshold for such recommendations would be at the discretion of the investigator. Among patients who do initiate therapy, on-treatment monitoring would then be used to ensure that only those highly likely to achieve an SVR (i.e., those with an RVR) would continue treatment. Patients with the highest scores (6–7) have a high chance of achieving an SVR even if they do not achieve an RVR (69%); thus, it may be worthwhile to continue treatment in such patients, regardless of the RVR status at week 4 of treatment. In such cases, the standard week 12 stopping rules should be applied. Stopping treatment at week 4 in patients with baseline predictions scores <6 who do not achieve an RVR would limit exposure to treatment, and thus the potential for adverse events in patients unlikely to achieve a cure.
HCV GT4 subtype was not determined in the majority of patients included in this analysis; hence, no firm conclusions can be drawn on the importance of GT4 subtype and the potential impact this might have on the applicability of the prediction score.
A selection tool similar to that in the present analysis has been developed for the identification of HCV GT1-infected patients likely to achieve an SVR with PegIFN alfa-2a/RBV [34]. The GT1 prediction tool was developed using data from treatment-naive Caucasian patients in the PROPHESYS cohorts [22], and requires baseline age, BMI, ALT and aspartate aminotransferase (AST) levels, platelet count, and HCV RNA level, to generate a prediction score that ranges from 0 to 10. Higher SVR rates were associated with higher baseline prediction scores such that SVR in Caucasian patients with HCV GT1 with scores of ≥5 and undetectable HCV RNA by week 4 was 86.7%. A modified version of this tool (i.e., minus AST) was recently evaluated in a cohort of 951 Caucasian non-cirrhotic patients with HCV GT1 infection, in which it was shown to be able to differentiate effectively between patients with a low and high chance of achieving an SVR [23]. A baseline prediction tool has also been developed for identifying HCV GT3 patients with low and high probability of SVR [35]. This latter analysis used the same database of patients as that used in this study and used similar methodology. The GT3 prediction tool includes age, bodyweight, cirrhosis status, ALT ratio, platelet count and baseline HCV RNA level to predict the likelihood of SVR in Caucasian patients. In contrast to the tool developed by Ferenci et al. [34] for GT1 and Asselah et al. [35] for GT3, the HCV GT4 baseline prediction tool may be used in both Black and Caucasian patients.
Physicians may be reluctant to treat patients with dual PegIFN alfa-2a/RBV therapy because of the high rates of adverse events associated with these drugs. In a large extended access program, the rate of withdrawal for adverse events was 10% [33]. The large prospective GUARD-C study evaluated factors associated with safety-related dose reductions and discontinuations (sr-RD) in patients treated with PegIFN alfa/RBV [23]. Among 3181 patients assigned to treatment with PegIFN alfa/RBV, the overall incidence of safety-related sr-RD of PegIFN alfa and RBV was 16.9% and 21.8%, respectively. Cox proportional hazards analysis showed that female sex, older age, lower BMI, infection with HCV GT 1 or 4 (rather than 2 or 3), the presence of cardiovascular and/or pulmonary disease, and low hematological indices (hemoglobin, neutrophils, platelets) at baseline were all significantly associated with sr-RD in these 3181 patients. The incidence of sr-RD increased in proportion to the number of these risk factors that were present at baseline. The SVR rate was highest in patients with none of these nine risk factors for sr-RD and lowest in patients with ≥6 of these nine risk factors for sr-RD [23]. This information could be used in conjunction with the baseline scoring system to further inform treatment decisions, to select the best patients for treatment with dual therapy and alternatively to identify patients who are not well suited to this regimen.
Highly effective all-oral interferon-free regimens are now available for the treatment of CHC including HCV GT4 [5]; however, these are not universally available, for various reasons. Worldwide, a majority of patients have not been screened for HCV infection and have not been treated, and access to DAAs is limited [2]. In the US, a majority of patients identified by screening do not receive therapy, and the main barrier to treatment is lack of health insurance [36]. For patients who do have insurance, access to treatment with new oral antivirals may be restricted by reimbursement criteria [37], such as a requirement for advanced fibrosis or cirrhosis. As a result, patients with CHC do not have access to treatment despite recommendations in treatment guidelines. For this reason, dual PegIFN alfa/RBV therapy remains a treatment option in settings where access to newer agents is restricted [6].
Limitations of this analysis include those usually associated with selected cohorts and retrospective analyses. The numbers of Black patients and of cirrhotic patients were low which may limit the generalizability of the scoring system. In addition, HCV GT4 subtype was not available for the majority of patients included in these studies, which precludes any comment on the importance of HCV GT4 subtype in prediction of SVR. Host IL28B genotype is the most important baseline predictor of SVR to PegIFN alfa-2a/RBV [19, 29, 38], but this information was not collected in either of the cohorts of patients included in the analysis, and therefore it was not possible to include it in the development of this scoring system.
The analysis shows that SVR rates increase with increasing baseline score in Black patients, but the association between prediction score and SVR rate was weaker in Black patients than in Caucasian patients. SVR rates in the few Black patients included in the analysis were found to be lower than in Caucasian patients with the same score, which is consistent with previous studies that have reported lower SVR rates in Black than non-Black patients treated with interferon-based therapies [26–30].
Patients with cirrhosis are in urgent need of treatment and should therefore be prioritized for treatment regardless of their baseline prediction score. These patients are most likely to have access to new direct-acting antiviral agents; however, should these new agents not be available, the tool can be used to inform decisions regarding dual therapy for these patients.
The strength of this clinical scoring system lies in its ease of use and inclusion of readily available baseline characteristics prospectively to identify HCV GT4-infected patients most likely to respond to treatment with PegIFN alfa-2a/RBV, avoiding unnecessary treatment, and thus adverse events, in those patients unlikely to experience treatment success. Further studies are required to validate the prediction method in larger datasets. Moreover, incorporating host IL28B genotype may lead to additional refinement of the predictive scoring system.
Conclusion
A simple scoring system can be used to identify GT4-infected patients with a high probability of achieving an SVR with dual PegIFN alfa-2a/RBV therapy. The scoring system can be used in Black or Caucasian patients, comprises four readily available patient demographic and disease characteristics, including age, ALT ratio, hepatic fibrosis status, and serum HCV RNA level, and can be easily incorporated into routine patient encounters.
References
Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57:1333–42.
Ward JW, Mermin JH. Simple, effective, but out of reach? Public health implications of HCV drugs. N Engl J Med. 2015;373:2678–80.
Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61:S45–57.
Asselah T, Bourlière M. Hepatitis C virus: current and evolving treatments for genotype 4. Gastroenterol Clin N Am. 2015;44:859–70.
Asselah T. Optimism for patients with genotype 4 HCV infection: clinical trials with direct-acting antivirals finally available. J Hepatol. 2015;62:996–9.
European Association for Study of Liver. EASL recommendations on treatment of hepatitis C 2015. J Hepatol. 2015;63:199–236.
Hezode C, Asselah T, Reddy KR, Hassanein T, Berenguer M, Fleischer-Stepniewska K, et al. Ombitasvir plus paritaprevir plus ritonavir with or without ribavirin in treatment-naive and treatment-experienced patients with genotype 4 chronic hepatitis C virus infection (PEARL-I): a randomised, open-label trial. Lancet. 2015;385:2502–9.
Abergel A, Metivier S, Samuel D, Jiang D, Kersey K, Pang PS, et al. Ledipasvir plus sofosbuvir for 12 weeks in patients with hepatitis C genotype 4 infection. Hepatology. 2016 (in press).
Lawitz E, Mangia A, Wyles D, Rodriguez-Torres M, Hassanein T, Gordon SC, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368:1878–87.
Moreno C, Hezode C, Marcellin P, Bourgeois S, Francque S, Samuel D, et al. Efficacy and safety of simeprevir with PegIFN/ribavirin in naive or experienced patients infected with chronic HCV genotype 4. J Hepatol. 2015;62:1047–55.
Hezode C, Hirschfield GM, Ghesquiere W, Sievert W, Rodriguez-Torres M, Shafran SD, et al. Daclatasvir plus peginterferon alfa and ribavirin for treatment-naive chronic hepatitis C genotype 1 or 4 infection: a randomised study. Gut. 2015;64:948–56.
American Association for the Study of Liver Diseases (AASLD), Infectious Diseases Society of America (IDSA). HCV guidance: recommendations for testing, managing, and treating hepatitis C. Updated 2016. http://www.hcvguidelines.org/. Accessed June 17, 2016.
Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Gonçales FL Jr, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975–82.
Manns MP, McHutchison JG, Gordon SC, Rustgi VK, Shiffman M, Reindollar R, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958–65.
Hadziyannis SJ, Sette H Jr, Morgan TR, Balan V, Diago M, Marcellin P, et al. Peginterferon-alpha2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med. 2004;140:346–55.
Esmat G, El Kassas M, Hassany M, Gamil M, El Raziky M. Optimizing treatment for HCV genotype 4: PEG-IFN alfa 2a vs. PEG-IFN alfa 2b; the debate continues. Liver Int. 2014;34(Suppl 1):24–8.
Ferenci P, Laferl H, Scherzer TM, Gschwantler M, Maieron A, Brunner H, et al. Peginterferon alfa-2a and ribavirin for 24 weeks in hepatitis C type 1 and 4 patients with rapid virological response. Gastroenterology. 2008;135:451–8.
Kamal SM, El Kamary SS, Shardell MD, Hashem M, Ahmed IN, Muhammadi M, et al. Pegylated interferon alpha-2b plus ribavirin in patients with genotype 4 chronic hepatitis C: the role of rapid and early virologic response. Hepatology. 2007;46:1732–40.
Asselah T, De Muynck S, Broet P, Masliah-Planchon J, Blanluet M, Bieche I, et al. IL28B polymorphism is associated with treatment response in patients with genotype 4 chronic hepatitis C. J Hepatol. 2012;56:527–32.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071–104.
Estrabaud E, Vidaud M, Marcellin P, Asselah T. Genomics and HCV infection: progression of fibrosis and treatment response. J Hepatol. 2012;57:1110–25.
Marcellin P, Cheinquer H, Curescu M, Dusheiko GM, Ferenci P, Horban A, et al. High sustained virologic response rates in rapid virologic response patients in the large real-world PROPHESYS cohort confirm results from randomized clinical trials. Hepatology. 2012;56:2039–50.
Foster GR, Coppola C, Derbala M, Ferenci P, Orlandini A, Reddy KR, et al. Impact of safety-related dose reductions or discontinuations on sustained virologic response in HCV-infected patients: results from the GUARD-C cohort. PLoS One. 2016;11:e0151703.
Clinical Steyerberg E, Models Prediction. A practical approach to development, validation, and updating. New York: Springer; 2009.
Sullivan LM, Massaro JM, D’Agostino RBS. Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med. 2004;23:1631–60.
Jeffers LJ, Cassidy W, Howell CD, Hu S, Reddy KR. Peginterferon alfa-2a (40 kd) and ribavirin for black American patients with chronic HCV genotype 1. Hepatology. 2004;39:1702–8.
Muir AJ, Bornstein JD, Killenberg PG. Peginterferon alfa-2b and ribavirin for the treatment of chronic hepatitis C in blacks and non-hispanic whites. N Engl J Med. 2004;350:2265–71.
Conjeevaram HS, Fried MW, Jeffers LJ, Terrault NA, Wiley-Lucas TE, Afdhal N, et al. Peginterferon and ribavirin treatment in African American and Caucasian American patients with hepatitis C genotype 1. Gastroenterology. 2006;131:470–7.
Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, Urban TJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature. 2009;461:399–401.
Poordad F, McCone J Jr, Bacon BR, Bruno S, Manns MP, Sulkowski MS, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195–206.
Fried MW, Hadziyannis SJ, Shiffman ML, Messinger D, Zeuzem S. Rapid virological response is the most important predictor of sustained virological response across genotypes in patients with chronic hepatitis C virus infection. J Hepatol. 2011;55:69–75.
Shiffman ML, Suter F, Bacon BR, Nelson D, Harley H, Sola R, et al. Peginterferon alfa-2a and ribavirin for 16 or 24 weeks in HCV genotype 2 or 3. N Engl J Med. 2007;357:124–34.
Lee SS, Roberts SK, Berak H, Dusheiko GM, Harley HA, Gane EJ, et al. Safety of peginterferon alfa-2a plus ribavirin in a large multinational cohort of chronic hepatitis C patients. Liver Int. 2012;32:1270–7.
Ferenci P, Aires R, Ancuta I, Arohnson A, Cheinquer H, Delic D, et al. A tool for selecting patients with a high probability of sustained virological response to peginterferon alfa-2a (40kD)/ribavirin. Liver Int. 2014;34:1550–9.
Asselah T, Thompson AJ, Flisiak R, Romero-Gomez M, Messinger D, Bakalos G, et al. A predictive model for selecting patients with HCV genotype 3 chronic Infection with a high probability of sustained virological response to peginterferon alfa-2a/ribavirin. PLoS One. 2016;11(3):e0150569.
Ditah I, Al Bawardy B, Gonzalez HC, Saberi B, Ditah C, Kamath PS, et al. Lack of health insurance limits the benefits of hepatitis C virus screening: insights from the National Health and Nutrition Examination Hepatitis C follow-up study. Am J Gastroenterol. 2015;110:1126–33.
Barua S, Greenwald R, Grebely J, Dore GJ, Swan T, Taylor LE. Restrictions for Medicaid reimbursement of sofosbuvir for the treatment of hepatitis C virus infection in the United States. Ann Intern Med. 2015;163:215–23.
Stattermayer AF, Stauber R, Hofer H, Rutter K, Beinhardt S, Scherzer TM, et al. Impact of IL28B genotype on the early and sustained virologic response in treatment-naive patients with chronic hepatitis C. Clin Gastroenterol Hepatol. 2011;9:344–50.
Acknowledgments
Sponsorship of these studies and article processing charges were funded by F. Hoffmann-La Roche Ltd, Basel, Switzerland. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. Editorial assistance in the preparation of this manuscript was provided by Dr. Manda Gent and Blair Jarvis of Health Interactions. Support for this assistance was funded by F. Hoffmann-La Roche Ltd, Basel, Switzerland. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Tarik Asselah is a speaker/consultant for Roche, AbbVie, Achillion, Boehringer-Ingelheim, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck. Gamal Esmat is a speaker, investigator and/or advisory board member for AbbVie, Bristol-Myers Squibb, Janssen, Merck, F Hoffmann-La Roche. Faisal M. Sanai is a consultant for/advises, is on the speakers’ bureau of, and has received grant support from F. Hoffmann-La Roche, and Bristol-Myers Squibb. He has been a consultant for, and advised Merck, Gilead Sciences, Janssen Pharmaceuticals and AbbVie. He is on the speakers’ bureau of Merck, Gilead Sciences, and AbbVie. Ioannis Goulis is a speaker, investigator and/or advisory board member for AbbVie, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck, F Hoffmann-La Roche. Diethelm Messinger is an employee of PROMETRIS GmbH. PROMETRIS GmbH has a contract with F. Hoffmann-La Roche Ltd to provide statistical support. Georgios Bakalos is an employee of F. Hoffmann-La Roche Ltd. Imam Waked is a speaker, investigator and/or advisory board member for AbbVie, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck, Pharco, F Hoffmann-La Roche.
Compliance with Ethics Guidelines
All procedures followed in the original studies were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/6AE4F060111952BB.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Asselah, T., Esmat, G., Sanai, F.M. et al. Simple Predictive Model for Identifying Patients with Chronic Hepatitis C and Hepatitis C Virus Genotype 4 Infection with a High Probability of Sustained Virologic Response with Peginterferon Alfa-2a/Ribavirin: Pooled Analysis of Data from Two Large, International Cohort Studies. Adv Ther 33, 1797–1813 (2016). https://doi.org/10.1007/s12325-016-0396-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-016-0396-4