Abstract
Introduction
Greater adherence to medications has been broadly demonstrated to be associated with improved clinical outcomes. However, there is limited real-world evidence on adherence to glucagon-like peptide-1 receptor agonist (GLP-1RA) therapy in patients with type 2 diabetes mellitus (T2DM).
Methods
This retrospective cohort study used United States administrative claims data to compare adherence to GLP-1RAs in T2DM patients initiating exenatide once weekly (QW), exenatide twice daily (BID), or once-daily liraglutide (initiated therapy = index therapy). Patients were included if they had T2DM, were GLP-1RA-naïve, initiated a GLP-1RA from 02/01/2012–01/31/2013 (date of initiation = index), were ≥18 years at index, and had continuous enrollment for 12 months before (baseline) to 6 months after index (follow-up). Study outcome was index GLP-1RA adherence (proportion of days covered [PDC] during follow-up, dichotomized at ≥80% vs. <80%, and at ≥90% vs. <90%). Multivariable logistic regressions compared adherence between the GLP-1RAs, adjusting for potential confounders. Sensitivity analyses were performed separating liraglutide by dose (1.2 mg/1.8 mg).
Results
Study sample included 4,041 exenatide QW, 4,586 exenatide BID, and 14,211 liraglutide (6,641 1.2 mg, 7,570 1.8 mg) patients. Median unadjusted PDC values were 0.783 for exenatide QW, 0.500 exenatide BID, 0.722 liraglutide, 0.761 liraglutide 1.2 mg, and 0.683 liraglutide 1.8 mg. Compared with patients treated with either exenatide BID or liraglutide, patients treated with exenatide QW had a statistically significantly greater multivariable-adjusted odds of achieving adherence of ≥80% (odds ratio vs. exenatide QW (OR) = 0.41 for exenatide BID; 0.80, liraglutide; 0.87, liraglutide 1.2 mg; 0.75, liraglutide 1.8 mg) and ≥90% (OR = 0.31 for exenatide BID; 0.60 liraglutide; 0.66 liraglutide 1.2 mg; 0.56 liraglutide 1.8 mg) (all P < 0.001).
Conclusion
Patients initiating exenatide QW had significantly higher adjusted odds of adherence compared with patients initiating other GLP-1RAs. Given differences in adherence across the GLP-1RAs, research correlating these factors with clinical and economic outcomes is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is a complex and chronic disorder that afflicts over 29 million individuals in the United States [1]. T2DM causes significant morbidity and mortality, and results in tens of billions of dollars in US healthcare expenditure annually [2]. T2DM is commonly managed through multi-modal strategies, including diet and exercise, with a key focus on glycemic control. The American Diabetes Association (ADA) recommends lowering glycated hemoglobin (HbA1C) to <7% in most non-pregnant adults with diabetes, with a primary goal of reduction in microvascular disease [3]. Among the available treatment strategies for T2DM, antidiabetes medications are commonly used in the medical care of T2DM, with an estimated 84% of patients with diabetes receiving one or more forms of antidiabetes medication [1].
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) represent a class of injectable antidiabetes medications that are indicated as adjunct therapy to diet and exercise to improve glycemic control in adults with T2DM, and have been recommended for use as monotherapy or in conjunction with other therapies in dual, triple, or more complex regimens [4–8]. According to ADA guidelines, metformin is the preferred initial pharmacologic agent for T2DM, while GLP-1RAs or other antidiabetes agent (oral or insulin) should be considered if noninsulin monotherapy at maximum tolerated dose does not achieve or maintain the patient’s HbA1C target over a period of 3 months [3]. The American Association of Clinical Endocrinologists 2013 Comprehensive Diabetes Management Algorithm suggests that GLP-1RAs can be used as initial monotherapy for patients with entry HbA1C <7.5% or in combination with metformin for patients with entry HbA1C ≥7.5% [8]. As of July 2014, in the United States, there were five approved GLP-1RAs with well-established clinical efficacy and differing dosing regimen complexity: exenatide twice daily (BID), exenatide once weekly (QW), liraglutide once daily, and, most recently, albiglutide QW and dulaglutide QW.
Poor adherence to antidiabetes medication can represent a barrier to optimal glycemic control. A variety of studies have correlated decreasing antidiabetes medication adherence with reduced glycemic control and increased health care costs and resource utilization [9–11]. One key element of the pharmacologic treatment of T2DM that has been identified as a barrier to optimal adherence is regimen complexity. Studies examining the association between antidiabetes medication regimen complexity and antidiabetes medication adherence have shown that regimens with less frequent dosing are associated with increased adherence [12–17]. This relationship, however, has not been evaluated among injectable GLP-1RAs, which differ widely with respect to dosing regimen complexity.
Thus, we undertook this retrospective cohort study to test the hypothesis that adherence to GLP-1RA therapy would differ among GLP-1RA-naïve patients treated with exenatide QW, exenatide BID, or liraglutide, each of which has different dosing frequencies. Because clinicians may be interested in whether dosing variations for liraglutide may confer alternative adherence outcomes relative to exenatide QW, a priori defined sensitivity analyses were performed separating liraglutide by dose (1.2 mg/1.8 mg).
Methods
Overview of Study Design
This was a retrospective cohort study based on United States administrative insurance claims data for a non-probability sample of individuals with employer-sponsored commercial or Medicare supplemental health insurance. GLP-1RA-naïve patients with T2DM who initiated a GLP-1RA between February 1, 2012 and January 31, 2013 were followed for 6 months thereafter to measure and compare their adherence to the GLP-1RA that they had initiated.
Data Source
The study data were administrative insurance claims data contained in the Truven Health MarketScan® Commercial Claims and Encounters (Commercial) and Medicare Supplemental and Coordination of Benefits (Medicare Supplemental) databases (Truven Health, Ann Arbor, MI, USA). These databases contain enrollment information, inpatient and outpatient medical, and outpatient pharmacy claims data for approximately 40 million individuals (annually) with employer-sponsored primary or Medicare supplemental health insurance. These databases have been used in multiple published evaluations related to medication adherence [18].
The study databases satisfy the conditions set forth in Sections 164.514 (a)-(b)1ii of the Health Insurance Portability and Accountability Act of 1996 privacy rule regarding the determination and documentation of statistically de-identified data. Because this study used only de-identified patient records and does not involve the collection, use, or transmittal of individually identifiable data, Institutional Review Board approval to conduct this study was not necessary. This article does not contain any new studies with human or animal subjects performed by any of the authors.
Study variables were measured from the database using enrollment records, International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes, Current Procedural Technology, 4th edition (CPT-4®) codes, Healthcare Common Procedure Coding System (HCPCS) codes, and National Drug Codes (NDCs), as appropriate.
Patient Selection Criteria
Patients were initially included in the study sample if they met the following inclusion criteria: filled at least one pharmacy claim for a GLP-1RA (exenatide QW, exenatide BID, or liraglutide) between February 1, 2012 (exenatide QW was approved in late January 2012) and January 31, 2013 (the date of the first of such claims was set as the index date); did not have pharmacy claims for more than one GLP-1RA on the index date; were 18 years or older on the index date; had at least 12 months of continuous pre-index medical and pharmacy benefits enrollment (designated the baseline period); had at least 6 months of continuous post-index medical and pharmacy benefits enrollment (designated the follow-up period); had at least one medical claim with a diagnosis code for T2DM (ICD-9-CM 250.x0 or 250.x2) in the baseline period or on the index date; and had no pharmacy claims for a GLP-1RA in the baseline period, a criterion applied in an attempt to restrict the sample to GLP-1RA-naïve patients.
Patients were excluded from the study sample if they had any medical claims with a diagnosis code for type 1 diabetes (ICD-9-CM 250.x1 or 250.x3) or gestational diabetes (ICD-9-CM 648.8x), or had any medical claims indicative of pregnancy or childbirth in the baseline or follow-up periods. Patients were allowed to switch between GLP-1RAs after index, an event which would result in lower adherence as described in greater detail within the next section.
Measurement of Adherence
The study outcome was adherence, measured using the ‘proportion of days covered’ (PDC) with index GLP-1RA during the 6-month follow-up period. The PDC is a commonly used measure of medication adherence, with the noted advantage of simultaneously reflecting elements of both adherence and persistence, as described in more detail below [19]. PDC was calculated by taking the number of days the patient was ‘covered’ (i.e., had days supplied for the medication ‘on hand’) on the index GLP-1RA during the 6-month follow-up period and dividing that by 180 days. For example, if a patient had three 30-day supplied prescriptions filled and exhausted during the 6-month follow-up, they would have had a total of 90 days supplied, and their PDC value would be 90/180 days, or 50%. If a patient had prescriptions of the index medication with overlapping days of supply (i.e., if a patient refilled early), it was assumed that the patient completed the first prescription and started taking the second prescription on the day after completing the first; thus, the calculation extended the end of the days of supply of the second prescription by the number of days that it overlapped with the first prescription. In the case that a patient filled a prescription with days supplied extending beyond the day 180 of follow-up, only the portion of the prescription’s days supplied that fell within the follow-up period was used in the numerator of the PDC formula. As the PDC is calculated over a fixed period of time and for only the index GLP-1RA, it is sensitive to both lapses in medication refills (adherence) and complete medication discontinuations and switches (persistence). For patients who switched their GLP-1RA after index, the days supplied for the GLP-1RA to which they switched would not be included in the numerator of the PDC calculation.
The continuous PDC measure was then dichotomized at two thresholds to create two separate binary outcomes: (1) PDC ≥80% vs. <80% and (2) PDC ≥90% vs. <90%. The PDC ≥80% threshold was chosen because of its ubiquitous use throughout the adherence literature, because it is the threshold at which Medicare evaluates prescription drug plans on their enrollees’ adherence to antidiabetes medications for the purposes of quality measurement, and because it has been shown to be clinically relevant in that it is predictive of hospitalization and mortality among patients with diabetes taking oral antidiabetes medications [20, 21]. The PDC ≥90% threshold was chosen as a sensitivity analysis to evaluate how the GLP-1RAs compare with one another with respect to patients achieving high levels of adherence and because prior analyses have shown that oral antidiabetes PDC values >89% have been associated with the greatest discriminant accuracy for predicting all-cause hospitalization among diabetics [22].
GLP-1RA Classification and Covariates
Patients were classified according to the GLP-1RA that they initiated on the index date. For liraglutide-treated patients, a priori sensitivity analyses related to dose were also conducted in which patients were classified as being treated with either liraglutide 1.2 mg (defined as having only prescriptions indicative of 1.2-mg dose on the basis of days supplied and metric quantity during the 6-month follow-up period) or liraglutide 1.8 mg (defined as having any prescriptions indicative of 1.8-mg dose on the basis of days supplied and metric quantity during the 6-month follow-up period). Liraglutide is delivered in a self-adjustable prefilled dosing pen and it is therefore possible that patients may have self-administered more or less liraglutide than would have been indicated for the given prescription’s days supplied and metric quantity.
The study covariates included patient demographics and clinical characteristics thought to potentially confound the relationship choice of GLP-1RA and the adherence outcomes. Patient demographics were measured at the index date, and patient clinical characteristics were measured throughout the baseline period.
Statistical Analyses
Bivariate analyses were used to display summaries of variable distributions, stratified by GLP-1RA and by dose for patients treated with liraglutide. In unadjusted analyses, chi-squared tests were used to test for differences in categorical variables and t tests were used to test for differences in continuous variables. Multivariable logistic regression models were used to compare the GLP-1RAs on the probability of achieving the adherence thresholds of PDC ≥80% and PDC ≥90%, treating exenatide QW as the reference category and adjusting for all patient demographics and clinical characteristics listed in Tables 1 and 2. The variance inflation factor was used to assess multi-collinearity of the models’ independent variables. Data extraction was performed using SAS™ Version 9.2 (SAS Institute, Inc, Cary, NC, USA). Statistical analyses were performed using StataMP 12 (StataCorp, College Station, Texas, USA). P values <0.05 were considered, a priori, to be statistically significant.
Results
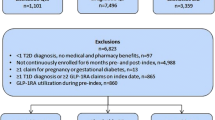
Figure 1 displays the changes in sample size associated with the application of each inclusion and exclusion criterion. From among 134,662 patients initially identified as having at least one pharmacy claim for a GLP-1RA from 02/01/2012–01/31/2013, 4,041 exenatide QW, 4,586 exenatide BID, and 14,211 liraglutide (6,641 1.2 mg, 7,570 1.8 mg) patients ultimately met all patient selection criteria.
Tables 1 and 2 display patients’ demographics and baseline clinical characteristics, respectively. Compared with patients treated with exenatide QW, patients treated with exenatide BID or liraglutide had significantly higher proportions of women (P < 0.05 for all comparisons), lower rates of baseline microvascular complications, lower rates of baseline dyslipidemia, lower mean (standard deviation [SD]) out-of-pocket monthly cost, and lower likelihood of visiting an endocrinologist at baseline. Compared with patients treated with liraglutide 1.2 mg, patients treated with liraglutide 1.8 mg were generally more similar at baseline to patients treated with exenatide QW.
Table 3 displays unadjusted data on adherence, as measured by the PDC, during the 6-month follow-up period. Among the GLP-1RAs, patients treated with exenatide QW had the numerically mean PDC (exenatide QW = 0.677; exenatide BID = 0.562; liraglutide = 0.667), median PDC (exenatide QW = 0.783; exenatide BID = 0.500; liraglutide = 0.722), and proportion of patients achieving PDC ≥80% (exenatide QW = 48.6%; exenatide BID = 30.3%, P < 0.001 vs. exenatide QW; liraglutide = 44.2%, P < 0.001 vs. exenatide QW) and PDC ≥90% (exenatide QW = 40.1%; exenatide BID = 19.8%, P < 0.001 vs. exenatide QW; liraglutide = 30.3%, P < 0.001 vs. exenatide QW). When compared with patients treated with each of the individual liraglutide dose categories, patients treated with exenatide QW had a mean PDC that was numerically greater than that of patients treated with liraglutide 1.8 mg (0.659) and equal to that of patients treated with liraglutide 1.2 mg (0.677); patients treated with exenatide QW also had the numerically greatest median PDC (liraglutide 1.2 mg = 0.761; liraglutide 1.8 mg = 0.683) and proportion of patients achieving PDC ≥80% (liraglutide 1.2 mg = 46.9%, P = 0.089 vs. exenatide QW; liraglutide 1.8 mg = 41.9%, P < 0.001 vs. exenatide QW) and PDC ≥90% (liraglutide 1.2 mg = 33.1%, P < 0.001 vs. exenatide QW; liraglutide 1.8 mg = 27.9%, P < 0.001 vs. exenatide QW).
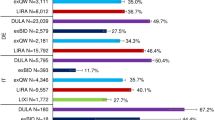
Figures 2 and 3 display the multivariable logistic regression-adjusted odds of attaining PDC ≥80% and PDC ≥90%, respectively, during the 6-month follow-up period, treating exenatide QW as the reference category. Compared with patients treated with either exenatide BID or liraglutide, including the individual liraglutide dose categories, patients treated with exenatide QW had statistically significant greater odds of achieving PDC ≥80% and PDC ≥90% (all P < 0.001). Differences were largest between patients treated with exenatide QW and patients treated with exenatide BID or liraglutide 1.8 mg. The magnitude of differences was greatest for the outcome of PDC ≥90%.
Multivariable logistic regression-adjusted odds of adherence (attaining proportion of days covered ≥80%) during 6-month follow-up period, with exenatide QW as reference category (n = 22,838). CI confidence interval, BID twice daily, QW once weekly. a P < 0.001 for exenatide QW vs. comparators. Full multivariable logistic regression results are available in Appendix Tables S1 and S2 with the models adjusted for age in years, Deyo–Charlson comorbidity index, number of unique ICD-9-CM diagnosis codes, number of unique 11-digit NDCs, total healthcare expenditures, out-of-pocket monthly cost for index GLP-1RA, patient sex, medicare enrollee (vs. commercial), region, health plan type, microvascular disease, cardiovascular disease, dyslipidemia, hypertension, hypoglycemia, obesity, renal impairment, endocrinologist visit, and prescription source (mail order, mail order/retail, retail pharmacy only)
Multivariable logistic regression-adjusted odds of adherence (attaining proportion of days covered ≥90%) during the 6-month follow-up period, with exenatide QW as reference category (n = 22,838). CI confidence interval, BID twice daily, QW once weekly. a P < 0.001 for exenatide QW vs. comparators. Full multivariable logistic regression results are available in Appendix Tables S2 and S3 with the models adjusted for age in years, Deyo–Charlson comorbidity index, number of unique ICD-9-CM diagnosis codes, number of unique 11-digit NDCs, total healthcare expenditures, out-of-pocket monthly cost for index GLP-1RA, patient sex, medicare enrollee (vs. commercial), region, health plan type, microvascular disease, cardiovascular disease, dyslipidemia, hypertension, hypoglycemia, obesity, renal impairment, endocrinologist visit, and prescription source (mail order, mail order/retail, retail pharmacy only)
Appendix Tables S1 through S4 display the detailed results of the multivariable logistic regressions. In all models, the variance inflation factor indicated no influential multi-collinearity of the models’ independent variables (data not shown). The association between covariates and the adherence outcomes were generally consistent across the models. Increasing age, having visited an endocrinologist during the baseline period, filling a prescription through mail order, having baseline dyslipidemia, and having an increasing number of NDCs during the baseline period were all associated with a statistically significant increased odds of achieving the adherence thresholds (all P < 0.05). In contrast, an increasing number of unique ICD-9-CM diagnosis codes recorded during the baseline period, increasing out-of-pocket monthly cost for the index GLP-1RA, being female, being covered by Medicare, and having baseline cardiovascular disease were all associated with a statistically significant decreased odds of achieving the adherence thresholds (all P < 0.05).
Discussion
This retrospective cohort study examined medication adherence in patients with T2DM initiating exenatide BID, exenatide QW, or liraglutide once daily. Over a 6-month period after new initiation of GLP-1RA therapy, patients treated with exenatide QW had a statistically significantly greater probability of achieving adherence of ≥80% and ≥90%—two clinically significant adherence thresholds in diabetes—when compared with patients treated with either exenatide BID or liraglutide. Exenatide QW was consistently associated with greater adherence when compared to both the 1.2-mg and the 1.8-mg dose groups of liraglutide, and the adjusted odds of adherence for exenatide QW grew stronger when examining the more restrictive adherence threshold of ≥90%.
Two prior studies have also compared GLP-1RAs with different administration frequencies, and one also found greater adherence with less frequent dosing but the other did not. Malmenäs and colleagues (2013) compared adherence (using a calculation that is identical to the PDC) over a 12-month follow-up period between patients treated with liraglutide 1.8 mg and patients treated with exenatide BID 10 mg [23]. Although the present study did not directly compare these specific treatments, Malmenäs and colleagues’ findings were generally consistent with those of the present study, suggesting that patients treated with exenatide BID 10 mg were less likely to achieve ≥80% adherence when compared with patients treated with liraglutide 1.8 mg. Malmenäs and colleagues hypothesized that reasons for this difference may have included frequency of treatment administration, with liraglutide having the benefit of once-daily administration over exenatide BID, among other factors.
In another retrospective cohort study, Pelletier and colleagues (2012) compared adherence (using PDC) over a 6-month follow-up period between patients treated with any dose of exenatide BID and patients treated with any dose of liraglutide [24]. In contrast to the present study, Pelletier and colleagues found that patients treated with exenatide BID and patients treated with liraglutide had similar mean adherence rates (exenatide BID PDC 56%, liraglutide PDC 57%, P = 0.088). Although it is not possible to determine why the results of the present study differ from those found by Pelletier and colleagues, it is possible that the mixed findings may be partially explained by the potential differences in treatment patterns of the index medications between the study time frame for Pelletier et al. (i.e., January 1, 2010 through June 30, 2010) versus the time frame of the present study. For example, liraglutide-treated patients in the Pelletier et al. analyses would have been early adopters of liraglutide (approved in January 2010) and may have been different (e.g., more severely diseased or difficult to treat) than patients who were prescribed liraglutide in 2012. Furthermore, these patients may have been selectively prescribed a once-daily regimen because of anticipated medication non-adherence concerns. Finally, Pelletier and colleagues compared patients treated with any dose of exenatide BID and patients treated with any dose of liraglutide. This may have led to the results differing from those of Malmenäs and colleagues, which corresponded to patients treated with exenatide BID 10 mg and patients treated with liraglutide 1.8 mg.
The present study is the first to evaluate adherence to exenatide QW in clinical practice. Thus, we are unable to compare the results for exenatide QW with other studies. We hypothesized that the reduced frequency of dosing associated with exenatide QW may confer adherence benefits. Although we did not attempt to fully isolate the effect of dosing frequency, the finding that exenatide QW was associated with the greatest probability of achieving the adherence thresholds—and that among the GLP-1RAs increasing dosage frequency was associated with decreasing adherence in general—is consistent with prior research suggesting that reduced regimen complexity is associated with increased adherence [3, 8–12]. Also, prior studies have found similar associations wherein an increasing number of baseline overall medications is predictive of increased antidiabetes medication adherence or decreased antidiabetes medication discontinuation risk [16, 25]. In the context of these findings related to regimen complexity, our study findings were consistent in that an increase in the overall number of baseline medications used (as measured by count of NDCs) was associated with a slightly increased probability of achieving the adherence thresholds. Furthermore, studies of regimen complexity have found that frequency of dosing can exert a greater influence than pill burden on antidiabetes medication adherence [13]. Thus, while other factors beyond dosing frequency may play a role in the likelihood of adherence to antidiabetes medications, we believe that there is a reasonable basis to partially attribute our findings to the reduced frequency of dosing—once weekly vs. once or twice daily—associated with exenatide QW.
Patients’ preferences for dosing and other features of antidiabetes regimens may also impact treatment satisfaction and medication adherence. Previous patient preference studies have demonstrated that less frequent daily dosing is preferred by patients with T2DM and may likely improve adherence to treatment with oral antidiabetes agents and that patients are willing to forego treatment benefits to avoid daily insulin injections [26, 27]. In a recent discrete-choice experiment comparing administration features of GLP-1RAs, when asked to choose between hypothetical treatments, a greater proportion of injection-naïve patients with T2DM preferred weekly injections over daily injections [28]. Injection frequency was reported as the most important attribute of GLP-1RA treatments, and preferences for other treatment features depended on injection frequency [28].
Another plausible explanation for the present study’s findings may be related to medication tolerability. In a head-to-head, 26-week, randomized study (DURATION-6) comparing the efficacy and tolerability of exenatide once weekly vs. liraglutide 1.8 mg once daily in patients with T2DM, patients treated with exenatide QW had a statistically significantly lower incidence of gastrointestinal tolerability problems when compared with patients treated with liraglutide 1.8 mg (9% and 21% experienced nausea, 6% and 13% experienced diarrhea, and 4% and 11% experienced vomiting, respectively) [29]. If such tolerability differences were a factor within the present study, this could be another potential explanation for the higher adherence rates observed in patients treated with exenatide QW versus patients treated with liraglutide. Furthermore, in the liraglutide cohort, the lower odds of achieving the adherence thresholds in patients treated with liraglutide 1.8 mg vs. liraglutide 1.2 mg are supported by clinical evidence that has shown that patients treated with liraglutide 1.8 mg tend to experience a greater incidence of tolerability issues than patients treated with liraglutide 1.2 mg [30–35].
We also evaluated the association between adherence and other demographic and clinical factors. Across the models, increasing age and filling a prescription through mail order were associated with greater adherence, and increasing comorbidity, increasing out-of-pocket monthly cost for the index GLP-1RA, and female sex were associated with lower adherence. We also found that having had a baseline visit with an endocrinologist was associated with significantly increased adjusted odds of adherence. These observed associations are consistent with prior research, which further supports the validity of our overall study findings [24, 36–39].
Although exenatide QW had the greater probability of achieving adherence of ≥80% and ≥90%, the overall unadjusted proportions of patients achieving these thresholds were low for all GLP-1RAs, ranging from 30.3% to 48.6% for the ≥80% threshold and from 19.8% to 40.1% for the ≥90% threshold. These findings of overall low adherence suggest a need for effective means to improve patient adherence to GLP-1RA therapy. Future studies using data that include information beyond that which may be included in administrative claims may help to identify patient, clinician, and payer-specific factors that may influence adherence. Identification of these factors will be critical to the design and implementation of interventions to improve patient adherence to GLP-1RA therapy, which will likely improve patient outcomes.
Our study has several important limitations. First, administrative claims data are not collected for research purposes, and the coding on administrative claims is recorded by physicians to support reimbursement. Diagnoses on claims may be coded incorrectly or missing, which may introduce measurement error with respect to ICD-9-CM-based variables. Second, although this study used the largest non-probability sample available in proprietary databases, findings from the study may not be generalizable to the entire United States population, including the uninsured or those who have insurance coverage through Medicaid or the military. Third, we classified patients treated with liraglutide into 1.2 or 1.8 mg on the basis of days supplied and metric quantity recorded on the pharmacy claims. Because liraglutide is delivered in a self-adjustable prefilled dosing pen, it is possible that patients may have self-administered more or less liraglutide than would be indicated for the given prescription’s days supplied and metric quantity. We do not know of any information regarding the likelihood of misclassification based on this approach. The consequences of misclassification would not affect our main results related to liraglutide overall, but would potentially limit the generalizability of our findings related to the individual 1.2 and 1.8 mg doses. Fourth, we did not examine whether adherence outcomes varied by dose for exenatide BID. It is possible that adherence outcomes could have differed by dose of exenatide BID and further research is needed to understand whether this is indeed the case. Fifth, because of the limited duration of history for which data are available on exenatide QW, our study examined a relatively short follow-up period of 6 months. Also, the patterns of exenatide QW use reflected only the first year of market availability, and these patterns may change over time. Thus, future analyses are needed to better understand the comparative long-term adherence to each GLP-1RA. Sixth, this study did not include all available GLP-1RAs, as albiglutide and dulaglutide were approved after the study period ended. Seventh, observational analyses such as the present study may be subject to residual confounding despite multivariable adjustment. Finally, patients may have been selectively prescribed a once-weekly regimen because of anticipated medication non-adherence, which may adversely impact findings among exenatide QW patients.
Conclusion
This retrospective cohort study compared medication adherence in patients with T2DM initiating GLP-1RAs with different dosage frequency. Patients with T2DM initiating the long-acting once-weekly formulation of exenatide had significantly higher adjusted odds of adherence compared with patients initiating short-acting GLP-1RAs. Our findings may have potential important clinical and economic implications, as poor adherence to antidiabetes medications in general has been associated with increases in HbA1C, hospitalization rates, and healthcare utilization and costs. Thus, understanding medication adherence to GLP-1RAs is critical to optimizing patient outcomes and glycemic control in routine care. Future studies are needed to examine the relationship between outcomes and adherence to GLP-1RAs.
References
Centers for Disease Control and Prevention. National diabetes statistics report. 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed June 26, 2014.
American Diabetes Association. Statistics about diabetes. http://www.diabetes.org/diabetes-basics/statistics/ (2013). Accessed March 28, 2014.
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(Suppl 1):S11–66.
Bydureon [package insert]. San Diego: Amylin Pharmaceuticals, Inc.; 2012.
Byetta [package insert]. San Diego: Amylin Pharmaceuticals, Inc.; 2011.
Victoza [package insert]. Plainsboro: Novo Nordisk; 2013.
Tanzeum [package insert]. Wilmington: GlaxoSmithKline LLC; 2014.
Tamez-Pérez HE, Proskauer-Peña SL, Hernŕndez-Coria MI, Garber AJ. AACE comprehensive diabetes management algorithm 2013. Endocr Pract. 2013;19:736–7.
Asche C, LaFleur J, Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes. Clin Ther. 2011;33:74–109.
Wild H. The economic rationale for adherence in the treatment of type 2 diabetes mellitus. Am J Manag Care. 2012;18(3 Suppl):S43–8.
Salas M, Hughes D, Zuluaga A, Vardeva K, Lebmeier M. Costs of medication nonadherence in patients with diabetes mellitus: a systematic review and critical analysis of the literature. Value Health. 2009;12:915–22.
Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med. 2005;118(Suppl 5A):27S–34S.
Zhang L, Zakharyan A, Stockl KM, Harada AS, Curtis BS, Solow BK. Mail-order pharmacy use and medication adherence among Medicare Part D beneficiaries with diabetes. J Med Econ. 2011;14(5):562–7 Am J Manag Care. 2012;18(3 Suppl):S49–S54.
Dezii CM1, Kawabata H, Tran M. Effects of once-daily and twice-daily dosing on adherence with prescribed glipizide oral therapy for type 2 diabetes. South Med J. 2002;95:68–71.
Ingersoll KS, Cohen J. The impact of medication regimen factors on adherence to chronic treatment: a review of literature. J Behav Med. 2008;31:213–24.
Melikian C, White TJ, Vanderplas A, Dezii CM, Chang E. Adherence to oral antidiabetic therapy in a managed care organization: a comparison of monotherapy, combination therapy, and fixed-dose combination therapy. Clin Ther. 2002;24:460–7.
Pollack M, Chastek B, Williams SA, Moran J. Impact of treatment complexity on adherence and glycemic control: an analysis of oral antidiabetic agents. J Clin Outcomes Manag. 2010;17:257–65.
Truven Health Analytics. MarketScan bibliography. http://marketscan.truvenhealth.com/marketscanuniversity/publications/2012%20Truven%20Health%20MarketScan%20Bibliography.pdf (2012). Accessed June 20, 2014.
Peterson AM, Nau DP, Cramer JA, Benner J, Gwadry-Sridhar F, Nichol M. A checklist for medication compliance and persistence studies using retrospective databases. Value Health. 2007;10:3–12.
Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–41.
Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27:2149–53.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25:2303–10.
Malmenäs M, Bouchard JR, Langer J. Retrospective real-world adherence in patients with type 2 diabetes initiating once-daily liraglutide 1.8 mg or twice-daily exenatide 10 μg. Clin Ther. 2013;35:795–807.
Pelletier EM, Pawaskar M, Smith PJ, Best JH, Chapman RH. Economic outcomes of exenatide vs liraglutide in type 2 diabetes patients in the United States: results from a retrospective claims database analysis. J Med Econ. 2012;15:1039–50.
Trinacty CM, Adams AS, Soumerai SB, et al. Racial differences in long-term adherence to oral antidiabetic drug therapy: a longitudinal cohort study. BMC Health Serv Res. 2009;9:24.
Hauber AB, Han S, Yang JC, et al. Effect of pill burden on dosing preferences, willingness to pay, and likely adherence among patients with type 2 diabetes. Patient Prefer Adherence. 2013;7:937–49.
Hauber AB, Johnson FR, Sauriol L, Lescrauwaet B. Risking health to avoid injections: preferences of Canadians with type 2 diabetes. Diabetes Care. 2005;28:2243–5.
Hauber AB, Nguyen H, Posner J, et al. Patient preferences for frequency of glucagon-like peptide-1 receptor agonists (GLP-1RA) injections in the treatment of type 2 diabetes. Presented at the 19th ISPOR annual international meeting. Montreal, QC, Canada. May 31–June 4, 2014.
Buse JB, Nauck M, Forst T, et al. Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): a randomised, open-label study. Lancet. 2013;381:117–24.
Marre M, Shaw J, Brandle M, et al. Liraglutide, a once-daily human GLP-1 analogue, added to a sulphonylurea over 26 weeks produces greater improvements in glycaemic and weight control compared with adding rosiglitazone or placebo in subjects with type 2 diabetes (LEAD-1 SU). Diabet Med. 2009;26:268–78.
Nauck M, Frid A, Hermansen K, et al. Efficacy and safety comparison of liraglutide, glimepiride, and placebo, all in combination with metformin, in type 2 diabetes: the LEAD (liraglutide effect and action in diabetes)-2 study. Diabetes Care. 2009;32:84–90.
Garber A, Henry R, Ratner R, Garcia, et al. Liraglutide versus glimepiride monotherapy for type 2 diabetes (LEAD-3 Mono): a randomised, 52-week, phase III, double-blind, parallel-treatment trial. Lancet. 2009;373:473–81.
Zinman B, Gerich J, Buse JB, et al. Efficacy and safety of the human glucagon-like peptide-1 analog liraglutide in combination with metformin and thiazolidinedione in patients with type 2 diabetes (LEAD-4 Met + TZD). Diabetes Care. 2009;32:1224–30.
Russell-Jones D, Vaag A, Schmitz O, et al. Liraglutide vs insulin glargine and placebo in combination with metformin and sulfonylurea therapy in type 2 diabetes mellitus (LEAD-5 met + SU): a randomised controlled trial. Diabetologia. 2009;52:2046–55.
Buse JB, Rosenstock J, Sesti G, et al. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet. 2009;374:39–47.
Gibson TB, Song X, Alemayehu B, et al. Cost sharing, adherence, and health outcomes in patients with diabetes. Am J Manag Care. 2010;16:589–600.
Lee WC, Balu S, Cobden D, Joshi AV, Pashos CL. Prevalence and economic consequences of medication adherence in diabetes: a systematic literature review. Manag Care Interface. 2006;19:31–41.
Hertz RP, Unger AN, Lustik MB. Adherence with pharmacotherapy for type 2 diabetes: a retrospective cohort study of adults with employer-sponsored health insurance. Clin Ther. 2005;27:1064–73.
Curkendall SM, Thomas N, Bell KF, Juneau PL, Weiss AJ. Predictors of medication adherence in patients with type 2 diabetes mellitus. Curr Med Res Opin. 2013;29:1275–86.
Acknowledgments
This study was sponsored by AstraZeneca, Fort Washington, PA, and Bristol-Myers Squibb, Plainsboro, NJ. AstraZeneca funded the article processing fees. All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. Boris Ivanov, employee of Truven Health Analytics, provided statistical programming support for this study.
Conflict of interest
Stephen Johnston is an employee of Truven Health Analytics. Katherine Cappell is an employee of Truven Health Analytics. James Nelson is an employee of Truven Health Analytics. Bong-Chul Chu is an employee of Truven Health Analytics. Truven Health Analytics was paid by the study sponsors to conduct this study. Hiep Nguyen is an employee of AstraZeneca and was an employee of Bristol-Myers Squibb at the time this study was conducted. Iftekhar Kalsekar is an employee of AstraZeneca and was an employee of Bristol-Myers Squibb at the time this study was conducted. Eugene Felber is an employee of Bristol-Myers Squibb.
Compliance with ethics guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Johnston, S.S., Nguyen, H., Felber, E. et al. Retrospective Study of Adherence to Glucagon-like Peptide-1 Receptor Agonist Therapy in Patients with Type 2 Diabetes Mellitus in the United States. Adv Ther 31, 1119–1133 (2014). https://doi.org/10.1007/s12325-014-0166-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-014-0166-0