Abstract
Cerebellar dysfunction is evident in several developmental disorders, including autism, attention deficit-hyperactivity disorder (ADHD), and developmental dyslexia, and damage to the cerebellum early in development can have long-term effects on movement, cognition, and affective regulation. Early cerebellar damage is often associated with poorer outcomes than cerebellar damage in adulthood, suggesting that the cerebellum is particularly important during development. Differences in cerebellar development and/or early cerebellar damage could impact a wide range of behaviors via the closed-loop circuits connecting the cerebellum with multiple cerebral cortical regions. Based on these anatomical circuits, behavioral outcomes should depend on which cerebro-cerebellar circuits are affected. Here, we briefly review cerebellar structural and functional differences in autism, ADHD, and developmental dyslexia, and discuss clinical outcomes following pediatric cerebellar damage. These data confirm the prediction that abnormalities in different cerebellar subregions produce behavioral symptoms related to the functional disruption of specific cerebro-cerebellar circuits. These circuits might also be crucial to structural brain development, as peri-natal cerebellar lesions have been associated with impaired growth of the contralateral cerebral cortex. The specific contribution of the cerebellum to typical development may therefore involve the optimization of both the structure and function of cerebro-cerebellar circuits underlying skill acquisition in multiple domains; when this process is disrupted, particularly in early development, there could be long-term alterations of these neural circuits, with significant impacts on behavior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The cerebellum has been referred to as “a neuronal learning machine” [1], but only recently has there been an increasing appreciation of its role in development and developmental disorders. Development is a period of rapid skill acquisition, and the cerebellum is thought to support implicit/procedural learning via the creation and error-driven modification of internal models of behavior. The cerebellum shows a similar developmental trajectory as the cerebral cortex, with regions that support more basic sensorimotor functions (such as the cerebellar anterior lobe [lobules I–V]), maturing earlier than those associated with higher-level cognitive functions (e.g., posterolateral lobule VII). The closed-loop circuits between the cerebellum and the cerebral cortex serve as the anatomical substrate by which the cerebellum can modulate activation patterns in distal regions (Fig. 1). Based on these interactions, it has been proposed that cerebellar dysfunction or disruption early in development could have major impacts on the structure and function of the cortical regions to which it projects [2].
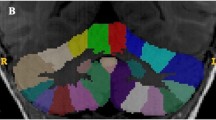
Cerebellum and developmental disorders. (Top, left) Schematic showing the closed-loop cerebro-cerebellar circuit with the frontal cortex: the cerebellar cortex projects via the deep nuclei, synapses in the thalamus, and onward to the cerebral cortex; the cerebral cortex projects via the pons to the cerebellum. Figure adapted from [2], with permission. (Top, right) Cerebellar grey matter in ASD [6]. The cluster in red shows the region in right Crus I where ASD children showed significantly reduced grey matter compared with a group of age-matched typically developing children. Other clusters show regions where grey matter volume correlated with scores on the Autism Diagnostic Observation Schedule (ADOS) and Autism Diagnostic Interview (ADI). Correlations between cerebellar grey matter and scores converged on right lobules VI and VII for ADOS Social Interaction (violet), ADOS Social Interaction + Communication (cyan), and ADOS Stereotyped Behaviors & Restricted Interests (green); ADI Social Interaction (blue) and ADI Restricted, Repetitive, & Stereotyped Behaviors (yellow) scores were associated with grey matter volume in the anterior cerebellum. (Bottom) Different cerebellar regions show grey matter reductions in ASD (red), ADHD (blue), and developmental dyslexia (green). Figure adapted from [3]
Here, we review the evidence that cerebellar dysfunction plays a critical role in neurodevelopmental disorders and discuss the potential contribution of the cerebellum to typical and atypical development. We focus on three developmental disorders in which cerebellar abnormalities have been well-documented (autism spectrum disorder [ASD], attention deficit-hyperactivity disorder [ADHD], and developmental dyslexia [3]) as well as the outcomes of cerebellar damage in pediatric populations.
ASD is characterized by deficits in communication and social interaction, accompanied by repetitive behaviors and restricted interests. The cerebellum is one of the most consistent sites of abnormality reported in ASD, with genetic, animal model, post-mortem, and neuroimaging studies reporting cerebellar differences (for reviews, [2, 4]). Hypoplasia of the posterior vermis was one of the first documented brain abnormalities in ASD, and decreased cerebellar cortical volume is an important classifier for ASD brains [4]. Across studies, grey matter reductions are consistently reported in right Crus I, left lobule VIII, and medial IX [3], which may have functional impacts on specific cerebro-cerebellar circuits; for example, reduced functional connectivity has been shown between right Crus I and left-hemisphere language regions in language-impaired children with ASD [5]. Structural differences in the cerebellar peduncles (see [4]) indicate disruption in both input and output pathways of cerebro-cerebellar circuits in ASD. Further, these cerebellar structural and functional abnormalities correlate with core autism behaviors (e.g., [6]; Fig. 1).
Cerebellar abnormalities have also been reported in ADHD, which is characterized by inattention, hyperactivity, and impulsivity. As in ASD, cerebellar findings were amongst some of the earliest reported differences in ADHD, with smaller cerebellar volumes reported in the first quantitative study of brain morphometry (for overview, see [3]). ADHD symptom severity has been shown to correlate with the degree of reduction in the posterior vermis (e.g., [7]) and overall cerebellar volume (e.g., [8]). Methylphenidate, one of the most common pharmacological treatments for ADHD, leads to changes in cerebellar activation in children with ADHD [9]. Consistent with this, posterior vermal reductions were not seen in children treated with methylphenidate [10], whereas cerebellar structural differences were the most significant finding in medication-naïve adults with ADHD [11]. A recent meta-analysis found consistent grey matter reductions in ADHD bilaterally in lobule IX ([3], Fig. 1) . Further, differences in both structural (e.g., middle cerebellar peduncles; e.g., [12]) and functional [13] cerebellar connectivity have been reported in ADHD.
Finally, developmental dyslexia is defined as a specific learning impairment in reading which cannot be accounted for by a general intellectual disability or lack of educational opportunity. Dyslexia is associated with a core behavioral deficit in phonological processing and slow, laborious reading. Poorer performance on a variety of “cerebellar” motor tasks has been reported in dyslexia, including balance, rapid pointing, peg moving, and control of eye movements [14]. These findings, coupled with the lack of fluent, automatic reading in dyslexia, led to the proposal that cerebellar dysfunction is a core neurobiological underpinning of dyslexia [15, 16]. As dyslexia is considered a specific learning impairment, cerebellar dysfunction leading to a procedural learning deficit could be a feasible explanation for dyslexic readers’ deficient literacy skill acquisition (see [16, 17]). Both structural and functional neuroimaging studies report cerebellar differences in dyslexic children and adults [14], and reduced grey matter in right lobule VI was found to be the most significant biomarker for classification of adult dyslexic brains [18]. Reduced grey matter in left lobule VI was also reported in a meta-analysis of voxel-based morphometry studies in dyslexia ([3], Fig. 1). More recent neuroimaging work suggests that the fluency component of dyslexia, characterized by rapid naming, is associated with abnormal activation in right lobule VI [19]. Finally, consistent with the idea that the cerebellum supports skill acquisition, right anterior cerebellar GM increased in response to successful remediation in dyslexia (see [14] for review).
An important theme is that different cerebellar subregions are affected in each disorder ([3]; Fig. 1), suggesting that the disruption of specific cerebro-cerebellar circuits may be relevant to the development of the behavioral features of ASD, ADHD, or dyslexia. Further, cerebellar damage can lead to symptoms—and sometimes diagnosis—of these disorders.
Data from clinical populations also suggest that early cerebellar damage is associated with a range of motor, cognitive, and affective outcomes in a location-dependent manner. Cerebellar damage has been directly associated with diagnoses of ASD (see [4]) and dyslexia (see [14]), and attention deficits in children following cerebellar damage often fall under the overarching executive function impairments associated with the cerebellar cognitive affective syndrome. While vermal damage and malformations have been associated with ASD symptoms (see [4]), right cerebellar damage has been associated with poorer language outcomes and left cerebellar damage has been associated with poorer visuo-spatial performance (e.g., [20]), reflecting the contralateral connections between the cerebellum and the cerebral cortex. Crucially, unlike damage to the cerebral cortex, outcomes following cerebellar damage in childhood can be more severe than cerebellar damage in adulthood [2].
In ASD, ADHD, and dyslexia, multiple regions of the brain show neural differences; therefore, it is important to consider the specific cerebellar contribution to the etiology of these disorders. Because the cytoarchitecture of the cerebellum is fairly uniform, it is thought that the cerebellum performs the same type of processing on whatever information it receives. One overarching potential mechanism of the cerebellar contribution to developmental disorders is in the realm of procedural learning (see [17]; e.g., explicit/declarative systems are thought to be intact in dyslexia and used for compensation). The role of the cerebellum in procedural learning may involve honing and optimizing the cerebro-cerebellar circuits that support a wide range of behaviors, from social skill acquisition, to modulation of attention, to the development of the left-hemisphere “reading” network as children acquire literacy skills. The formation of internal models within the cerebellum enables this optimization of performance, presumably through the modulation of activity in regions targeted by cerebellar output. When this modulation is lost, behavior becomes error-ridden and poorly calibrated, and procedural skill acquisition is disrupted.
Given that the cerebellum is thought to be maximally involved during the initial stages of learning, and less involved in the retention of learned behaviors, it is feasible that the cerebellum is more important earlier in life when cerebro-cortical networks are first being established, and less important later in life when behaviors have been appropriately set up in distributed cortical networks. Therefore, depending on the specific subregions where developmental differences arise, cerebellar dysfunction could impact behaviors associated with autism, ADHD, and dyslexia through the disruption of circuits supporting language and social cognition, attention, and literacy acquisition, respectively.
References
Raymond JL, Lisberger SG, Mauk MD. The cerebellum: a neuronal learning machine? Science. 1996;272(5265):1126–31.
Wang SS, Kloth AD, Badura A. The cerebellum, sensitive periods, and autism. Neuron. 2014;83(3):518–32.
Stoodley CJ. Distinct regions of the cerebellum show gray matter decreases in autism, ADHD, and developmental dyslexia. Front Syst Neurosci. 2014;8:92.
Becker EB, Stoodley CJ. Autism spectrum disorder and the cerebellum. Int Rev Neurobiol. 2013;113:1–34.
Verly M, Verhoeven J, Zink I, Mantini D, Peeters R, Deprez S, et al. Altered functional connectivity of the language network in ASD: role of classical language areas and cerebellum. Neuroimage Clin. 2014;4:374–82.
D’Mello AM, Crocetti D, Mostofsky SH, Stoodley CJ. Cerebellar grey matter and lobular volumes correlate with core autism symptoms. Neuroimage Clin. 2015;7:631–9.
Ivanov I, Murrough JW, Bansal R, Hao X, Peterson BS. Cerebellar morphology and the effects of stimulant medications in youths with attention deficit-hyperactivity disorder. Neuropsychopharmacology. 2014;39(3):718–26.
Castellanos F, Lee P, Sharp W, Jeffries N, Greenstein D, Clasen L, et al. Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA. 2002;288:1740–8.
Rubia K, Halari R, Cubillo A, Mohammad AM, Brammer M, Taylor E. Methylphenidate normalises activation and functional connectivity deficits in attention and motivation networks in medication-naive children with ADHD during a rewarded continuous performance task. Neuropharmacology. 2009;57(7–8):640–52.
Bledsoe J, Semrud-Clikeman M, Pliszka SR. A magnetic resonance imaging study of the cerebellar vermis in chronically treated and treatment-naive children with attention-deficit/hyperactivity disorder combined type. Biol Psychiatry. 2009;65(7):620–4.
Makris N, Liang L, Biederman J, Valera EM, Brown AB, Petty C, et al. Toward defining the neural substrates of ADHD: a controlled structural MRI study in medication-naive adults. J Atten Disord. 2013.
Bechtel N, Kobel M, Penner IK, Klarhofer M, Scheffler K, Opwis K, et al. Decreased fractional anisotropy in the middle cerebellar peduncle in children with epilepsy and/or attention deficit/hyperactivity disorder: a preliminary study. Epilepsy Behav. 2009;15(3):294–8.
Tomasi D, Volkow ND. Abnormal functional connectivity in children with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2012;71(5):443–50.
Stoodley CJ, Stein JF. Cerebellar function in developmental dyslexia. Cerebellum. 2013;12(2):267–76.
Nicolson R, Fawcett A, Dean P. Developmental dyslexia: the cerebellar deficit hypothesis. Trends Neurosci. 2001;24(9):508–11.
Nicolson RI, Fawcett AJ. Dyslexia, dysgraphia, procedural learning and the cerebellum. Cortex. 2011;47(1):117–27.
Ullman MT, Pullman MY. A compensatory role for declarative memory in neurodevelopmental disorders. Neurosci Biobehav Rev. 2015;51:205–22.
Pernet CR, Poline JB, Demonet JF, Rousselet GA. Brain classification reveals the right cerebellum as the best biomarker of dyslexia. BMC Neurosci. 2009;10:67.
Norton ES, Black JM, Stanley LM, Tanaka H, Gabrieli JD, Sawyer C, et al. Functional neuroanatomical evidence for the double-deficit hypothesis of developmental dyslexia. Neuropsychologia. 2014;61:235–46.
Scott RB, Stoodley CJ, Anslow P, Paul C, Stein JF, Sugden EM, et al. Lateralized cognitive deficits in children following cerebellar lesions. Dev Med Child Neurol. 2001;43(10):685–91.
Acknowledgments
This work was supported by the National Institutes of Health under award number R15MH106957. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health. The author would like to thank Anila D’Mello and Lauren McGrath for helpful comments and discussion.
Conflict of Interest
The author declares that she has no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stoodley, C.J. The Cerebellum and Neurodevelopmental Disorders. Cerebellum 15, 34–37 (2016). https://doi.org/10.1007/s12311-015-0715-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-015-0715-3