Abstract
The Bounce Back program (Langley et al. in J Consult Clin Psychol 83:853, 2015) effectively reduces post-traumatic stress (PTS) symptoms and internalizing problems among Elementary students (Langley et al. in J Consult Clin Psychol 83:853, 2015; Santiago et al. in School Psychol Q 33:1–9, 2018). Some school settings may modify the program to accommodate challenges such as logistic difficulties (e.g., a busy academic schedule) and clinicians’ discomfort with parts of the protocol (i.e., the trauma narrative). Thus, research is needed to answer the question, “Can we expect to observe change if we implement a modified Bounce Back program?” Our objectives were to (1) replicate treatment outcomes, (2) examine the timing of symptom reduction to determine whether symptoms abated before and/or after the trauma narrative, and (3) test whether baseline factors predicted incremental benefits of the trauma-narrative for PTS reduction. Twenty K-5 th grade students (47.4% Hispanic/Latino, 36.8% African-American, and 63.2% White; 68% boys) attending an urban Title I Elementary school completed the Bounce Back program and reported symptoms at pre, mid therapy (immediately before the trauma narrative), and post therapy (immediately following the program). Consistent with other trials of the Bounce Back program, students in the current sample experienced significantly reduced PTS symptoms, distress, internalizing problems, and externalizing problems. Significant change in PTS and distress occurred in the first part of treatment before the trauma narrative and did not occur during the second part of treatment. The full course of treatment was needed for significant change on secondary outcomes of internalizing and externalizing problems. Distress and bereavement assessed at baseline did not predict incremental benefits of the second half of treatment. Findings yield implementation implications and directions for future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Children experience potentially traumatic circumstances like abuse, neglect, domestic violence, and community violence at alarming rates. The majority of children have witnessed, learned about, or directly experienced a potentially traumatic event (Copeland, Keeler, Angold, & Costello, 2007; McLaughlin et al., 2013). More than a third of youth have experienced multiple traumas (Copeland et al., 2007) and a quarter of youth have experienced “high magnitude” traumatic events (Costello, Erkanli, Fairbank, & Angold, 2002). These events increase risk for a wide range of psychological difficulties including post-traumatic stress (PTS) (Alisic et al., 2014; Dunn, Nishimi, Powers, & Bradley, 2017; McLaughlin et al., 2012; 2013).
Fortunately, research supports cognitive behavioral therapy (e.g., TF-CBT; Cohen, Mannarino, & Deblinger, 2012) as an efficacious and effective treatment approach for child post-traumatic stress (PTS) symptoms (de Arellano et al., 2014; Dorsey et al., 2017). Even so, many children with PTS struggle to access mental health care due to a shortage of community mental health clinicians and barriers such as transportation difficulties, limited caregiver availability to participate, and high treatment costs to families (Costello, Sampson, Kessler, & Merikangas, 2014; Kataoka, Zhang, & Wells, 2002). Poor accessibility to treatment is particularly problematic for children living in economically disadvantaged neighborhoods and for racial and ethnic minority children. Children living in economically disadvantaged neighborhoods stand at a heightened risk of traumatic exposure (e.g., Fong, 2019; Baglivio, Wolff, Epps, & Nelson, 2017) compared to youth living in more affluent contexts. Among racial and ethnic minority youth, PTSD may be under-recognized and under-treated (Schwartz, Bradley, Sexton, Sherry, & Ressler, 2005), which is particularly troublesome given research suggesting that Black/African Americans adults have the highest rates of probable lifetime PTSD (Alegría et al., 2013) and the highest risk of developing PTSD among trauma-exposed populations (Roberts, Gilman, Breslau, Breslau, & Koenen, 2011).
Implementation in the school setting improves accessibility for students who need mental health care by reducing common barriers to treatment in the community such as the need for transportation, the requirement of parental participation, and cost to the client (Lyon & Bruns, 2019). School-based interventions for PTS have demonstrated medium to large effects (Rolfsnes & Idsoe, 2011; Sanchez et al., 2018) and the value of school-based implementation is evident in the Jaycox et al. (2010) finding that students were more likely to participate in TF-CBT when offered at school (98%) versus when the same treatment was offered (at no cost to the student’s family) in a community clinic outside of school (37%).
Still, there are many challenges to successfully transferring clinical interventions for PTS from clinics to school settings. Fitting sessions into the busy school schedule is one significant implementation challenge since session time must be balanced with class instructional time needed to meet educational benchmarks. Langley, Nadeem, Kataoka, Stein, & Jaycox (2010) highlighted this difficulty, indicating that some teachers did not permit students to leave their classes to attend therapy sessions. Likewise, assemblies, special schedules, and consolidated school days made scheduling sessions particularly difficult (Langley et al., 2010). With so many competing demands on time, school-based interventions must be efficient as possible in order to provide an acceptable “fit” for the school setting.
Another factor that limits the potential impact of school-based trauma treatments is that some school-based professionals lack the training, comfort, and willingness to implement some components of effective treatments. Despite the evidence supporting their effectiveness, exposure-based treatments have been described as having a “public relations problem” that hinders their broad dissemination (Olatunji, Deacon, & Abramowitz, 2009). This problem reflects concerns that exposure intentionally evokes temporary distress. Such distress is incorrectly believed to exacerbate symptoms and cause high rates of attrition, despite empirical work suggesting the contrary (Hembree et al., 2003; Imel, Laska, Jakupcak, & Simpson, 2013). Interestingly, data from clients suggest that exposure-based therapies are not only acceptable to clients, but are, in fact, among clients’ top choices of treatment even when other approaches are offered (Becker, Darius, & Schaumberg, 2007; Feeny, Zoellner, Mavissakalian, & Roy-Byrne, 2009; Tarrier et al., 2006). Thus, it appears that clinician preferences contribute to the under-utilization of exposure treatments (van Minnen, Hendriks, & Olff, 2010) and even practitioners with specific training in exposure treatments report hesitancy to use these techniques due to concerns about how both the client and clinician will tolerate the exposure (Becker, Zayfert, & Anderson, 2004).
These clinical concerns coupled with common program implementation issues among school staff, such as competing job responsibilities, limited time, and perceived lack of support (Langley et al., 2010), highlight only some of the multiple professional and logistical concerns that school-based mental health professionals express about treating PTS at school. Since mental health clinicians routinely modify psychosocial treatment protocols to better fit the needs of their clients, clinicians, and settings (Stirman et al., 2013), it logically follows that some school-based clinicians may consider shortening CBT by omitting the trauma narrative, which is an exposure-heavy component of therapy that requires significant clinician time (e.g., individual breakout sessions). To promote research-based practice, it is important to test whether treatment modifications such as shortening treatment by removing a trauma narrative may impact expected outcomes.
Four studies to date have assessed whether the trauma narrative is essential to reducing PTS symptoms. Two of these studies have examined the trauma narrative in the context of individual trauma-focused cognitive behavioral therapy. Nixon, Sterk, & Pearce (2012) conducted a randomized trial that compared a 9 week course of TF-CBT (with exposure) to a 9 week course of trauma-focused cognitive therapy (CT; TF-CBT without exposure) for youth who had a single incident traumatic experience. Authors concluded that exposure is not a prerequisite for positive therapeutic outcomes. Similarly, Deblinger, Mannarino, Cohen, Runyon, and Steer (2011) randomized child sexual abuse survivors into one of four TF-CBT conditions (8 sessions or 16 sessions, with or without the trauma narrative component). Researchers found that, overall, TF-CBT was effective in improving participant symptoms regardless of the inclusion of a trauma narrative or the length of treatment. While all conditions were effective in reducing PTS symptoms, different treatment conditions demonstrated superior results on other outcomes. For some outcomes (e.g., child’s fear about talking about abuse, child anxiety at post-treatment, parental abuse-specific emotional distress), the conditions that included a trauma narrative demonstrated superior results, while, for other outcomes (e.g., parental report of externalizing symptoms, parental report of effective parenting practices), conditions without a trauma narrative demonstrated superior outcomes. Taken together, these findings suggest that significant symptom reduction occurs during TF-CBT even without the inclusion of a trauma narrative, but that some outcomes respond better when a trauma narrative is included while other outcomes respond better when treatment does not include a trauma narrative (Deblinger et al., 2011).
Two additional studies have evaluated whether trauma narrative processing is essential to group-based CBT for youth with PTSD. Layne et al. (2008) compared a psychoeducation and skill building intervention to a trauma and grief group intervention (that included a narrative component) implemented in a sample of war-exposed Bosnian adolescents. Researchers found that PTS symptoms significantly decreased in both conditions, but that maladaptive grief reactions reduced only in the treatment condition that contained a narrative, which may suggest that bereaved adolescents, in particular, benefit from narrative work. Salloum and Overstreet (2012) compared outcomes between two forms of a grief and trauma intervention. One form included coping skills and trauma narrative processing, while the other form included coping skills only. Researchers found that children in both treatment groups demonstrated significant improvements, but that highly distressed youth experienced more symptom relief when narrative processing was included. Thus, it may be that PTS reductions are possible without the trauma narrative, but that bereaved and highly distressed youth experience incremental gains when the trauma narrative is included in treatment. More studies are needed to understand whether factors identified at baseline (e.g., bereavement and baseline distress) predict which youth will significantly benefit from the trauma narrative. This information can help to individualize group treatment to produce optimal outcomes for each student.
The Bounce Back program (Langley, Gonzalez, Sugar, Solis, & Jaycox, 2015) is administered at school through 10 sessions of group CBT, parent information sessions, and up to 3 individual pull out sessions in which students meet individually with a clinician to develop a trauma narrative. Bounce Back has been shown to be a helpful treatment through one randomized control trial (RCT) conducted by the treatment developers (Langley et al., 2015) and through a “real world” replication trial (Santiago et al., 2018). In the first trial, social workers and clinical psychologists implemented Bounce Back with groups of 1st–5th grade students (50% boys, 49% Latino, 27% Caucasian, 18% African American) attending a Title I elementary school in an urban school district in Los Angeles. The treatment developer led the research team and supported the clinicians through an initial training and regular supervision meetings throughout the trial. In the replication trial (Santiago et al., 2018), school-based social workers implemented Bounce Back with groups of 1st through 4th grade students (65% boys; 82% Latino) in an urban district in Illinois. The treatment developer conducted an initial training with clinicians and continued to consult through out the implementation. Both studies suggest that Bounce Back is helpful in reducing post-traumatic stress (PTS) symptoms and internalizing problems. External research teams’ studies of additional implementations with other samples that do not have implementation support from the treatment developer can aid in determining whether Bounce Back is ready for broad dissemination (Flay et al., 2005). Furthermore, research can build upon growing evidence for the Bounce Back program by exploring the process of change. Currently, little is known about the process by which positive outcomes come about and which components of treatment are most essential to therapeutic gains. Understanding the process of change during the Bounce Back program can help clinicians to determine a timeframe for when progress in treatment should be evident and can help to clarify whether schools can expect to observe change if they reduce the length of treatment.
The Current Study
To build upon existing work, the current study had three objectives. First, we aimed to replicate and expand upon the two existing studies that suggest that the Bounce Back program is a beneficial approach to treating youth with PTS symptoms at school (Langley et al., 2015; Santiago et al., 2018). We expected that PTS, distress, internalizing problems, and externalizing problems would significantly decrease during students’ participation in Bounce Back. Secondly, we aimed to build upon research suggesting that significant reductions in PTS and related difficulties occur in early phases of treatment and occur regardless of the inclusion of a trauma narrative. To do this, we examined when change in primary symptoms (e.g., PTS, subjective distress) and secondary difficulties (e.g., internalizing problems, externalizing problems) occurred during an open trial of the Bounce Back program. Given the literature suggesting that TF-CBT is effective in reducing PTS symptoms regardless of the inclusion of a trauma narrative (Deblinger et al. 2011; Nixon et al., 2012), we expected to observe significant reduction in PTS during the first half of Bounce Back (i.e., before the trauma narratives). Aligning with the finding that TF-CBT without a narrative shows superior externalizing outcomes to TF-CBT with a narrative (Deblinger et al. 2011), we expected that the externalizing problems would significantly decrease in the first half of treatment (before the trauma narrative). Based on the finding that TF-CBT with a narrative has a greater effect on fear and anxiety (Deblinger et al. 2011), we expected to observe internalizing symptoms decrease during the second half of treatment (which included the trauma narrative). Finally, we aimed to test whether factors assessed at baseline (report of bereavement, subjective distress) would predict which youth benefit from the second part of treatment that contains the trauma narrative.
Method
Procedures
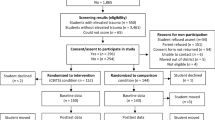
The study was conducted in strict adherence to the multi-step protocol approved by University of Delaware’s Institutional Review Board (Fig. 1).
Recruitment and Screening for Eligibility
In fall 2017, parents/guardians of all kindergarten through fifth grade students attending one urban, Title I elementary school in a small Mid Atlantic state received letters describing the purpose of conducting a trauma-focused screening and the procedures by which the screening would be conducted. After learning about the screening and study procedures, parents/guardians provided consent for students to be screened. Students with parent/guardian consent left class to meet individually with a clinician who explained the screening purpose and procedure to the student. Students who provided assent underwent a screening interview in which the clinician evaluated trauma exposure, PTS, distress related to the students’ identified “top problems,” internalizing problems, and externalizing problems using the measures described below.
Determining Eligibility, Consent for Treatment, and Treatment Initiation
Students who endorsed a heightened level of PTS symptoms and functional impairment during the screening qualified for groups. Based on the criteria set during the initial trial of the Bounce Back program (Langley et al., 2015), we set a score of 20 on the UCLA PTSD reaction index for DSM-5 (UCLA-R5, Steinberg, Brymer, Decker, & Pynoos, 2004; Steinberg et al., 2013; Elhai et al., 2013) as the minimum criterion for eligibility for group. We contacted parents of all students who meet this criterion by phone and mail to request permission for their students to participate in school-based services and, if preferred by the family, to offer referrals to other services.
Participants
Screened Sample
The screened sample (n = 147) consisted of students from kindergarten through fifth grade (kindergarten 11%, first grade 19%, second grade 19%, third grade 25%, fourth grade 14%, and fifth grade 12%). The screened sample was 61% Hispanic or Latinx, 20% Black/African-American, and 76% White/Caucasian (these race/ethnicity categories were not mutually exclusive and school records identified students in multiple categories). Boys comprised 52% percent of the screened sample.
Treatment Subsample
The subsample of students who qualified and participated in Bounce Back is the focus of this study. These students include 22 kindergarten through fifth grade students (kindergarten 9.1%, first grade 27.3%, second grade 13.6%, third grade 31.8%, fourth grader 4.5%, and fifth grade 13.6%). The treatment sample was 47.4% Hispanic or Latinx, 36.8% Black/African-American, and 63.2% White/Caucasian (these race/ethnicity categories were not mutually exclusive and school records identified students in multiple categories). Boys comprised 64% of the treatment sample. Over the course of implementation, two students withdrew from the program (one due to lack of interest and one due to moving from the school). Twenty students completed group. Table 1 displays demographic information for the whole school, screened sample, and treatment subsample.
Bounce Back Group Implementation
The Bounce Back program (Langley et al., 2015) is a trauma-focused CBT for students in kindergarten through fifth grade that is implemented across 10 group sessions, up to three individual sessions, 1–3 parent education sessions, and up to one conjoint session with a caregiver per child.
Clinical teams included a doctoral-level psychologist and a trainee in a clinical psychology doctoral program, a choice that facilitated training opportunities for future Psychologists while introducing the idea of supervised student clinicians as an economical way by which schools may increase their capacity for mental health service provision. Therapy teams led five groups that were comprised of an average of 4 students (range = 3–7 students) all of whom were within 1 grade of each other. To promote sustainability by training school-based mental health professionals, two groups had a school-based mental health professional (i.e., school guidance counselor or school psychologist) as an additional group leader. Groups met for 10 sessions between February and May 2018. Students were pulled out of their “specials” (e.g., gym, music, art, technology, library) during the regular school day to participate in a 50-min session once a week. All students attended at least 8 sessions as a criterion for participation. When a student missed a group, a clinician met with that student to provide an overview of missed content.
During the first half of treatment (sessions 1–5), clinicians led the group in exercises focused on psychoeducation, emotion identification and processing, physiological arousal and relaxation training, and cognitive work. In session 5, clinicians provided a rationale for gradual exposure as a solution to avoidance behaviors. In the second half of group (sessions 5–10), clinicians reviewed coping skills, discussed social support and problem solving, facilitated exposure practice, focused on relapse prevention, and celebrated students’ progress through treatment. Importantly, the second half of the implementation also included pull out sessions where a clinician met individually with each student for 1–3 sessions in which they developed and processed a trauma narrative. Three parent sessions were offered in the school cafeteria on weeknight evenings, although, few parents participated in these sessions (e.g., 0–5 parents attended each session). Similarly, parents were invited to participate in a conjoint session with their child, but only 1 student’s parent participated.
Symptom Assessment
At baseline, students completed an individual interview to assess traumatic exposure, posttraumatic stress symptoms, distress related to three top problems identified by the student, internalizing problems, and externalizing problems. Symptoms were re-assessed at mid-treatment (immediately before the trauma narrative) and immediately following treatment. All items were read aloud to all students and students marked their responses.
Measures
Fidelity to the Treatment Model
Multiple aspects of the implementation design promoted fidelity to the model for clinical purposes during the implementation. All clinicians were trained and Bounce Back certified. Graduate student clinicians co-led sessions with a doctoral-level supervisor and attended weekly supervision meetings in which supervisors reviewed the treatment manual and audiotaped recordings of sessions. Clinical care quality control (rather than research objectives) was the primary reason for monitoring fidelity during the implementation.
After the implementation, for research purposes, research assistants transcribed sessions and coded twenty percent of sessions that were selected at random. Two coders who were not involved in the implementation independently rated the transcripts for session-specific adherence to the treatment manual. Specifically, the treatment manual included a checklist of specific content topics for each session. The full 10 session implementation included 57 content topics (M = 5.7 codes per session; SD = .68). Raters dichotomously rated whether each contact topic on the checklist was covered during the session (0 = content absent, 1 = content present). Coders evidenced strong inter-rater reliability with a 91% agreement on all independent ratings. The rare coding discrepancies were resolved by consensus and the consensus ratings are those that are reported in results.
Trauma Exposure
Clinicians administered the Traumatic Events Screening Inventory for Children (TESI-C; Daviss et al., 2000; Ford et al., 2002) as an individual interview at baseline to assess students’ exposure to potentially traumatic events. Students could endorse up to 24 potentially traumatic events. One of these events included bereavement and was coded dichotomously (e.g., 1 = yes bereaved, 0 = not bereaved) 46% of students who were screened endorsed experiencing significant loss. Existing literature shows that the TESI-C has strong psychometric properties (Ribbe, 1996). To qualify for treatment, students needed to endorse at least one traumatic event. On average, children in our screening sample were exposed to 3.4 traumatic events (Range 0–12, SD = 2.61). At follow up data collection points, a clinician read the traumatic events endorsed at baseline to the student before assessing PTS symptom severity.
PTS Symptoms
At baseline, before the trauma narrative, and following treatment, students completed an individual interview in which they responded to the UCLA PTSD reaction index for DSM-5 (UCLA-R5, Steinberg et al., 2004; 2013; Elhai et al., 2013). The UCLA-R5 assesses the severity of PTS symptoms by measuring the frequency in which symptoms occurred during the past month. Students rated each item on a 5-point Likert scale ranging from 0 (never) to 4 (most of the time). Internal consistency for the treatment sample was good at baseline (α = .91) midpoint (α = .94), and post-treatment (α = .92).
Internalizing Problems, Externalizing Problems, and Subjective Distress
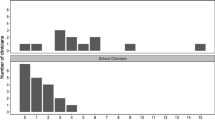
At baseline, students completed the Top Problems/Brief Problems Checklist (TP/BPC; Weisz et al., 2011). The TP/BPC includes two parts—an idiographic “top problem” report and rating and a checklist of internalizing and externalizing problems that were adapted from the Youth Self Report/Child Behavior Checklist (Achenbach & Rescorla, 2001). To complete the top problem portion, students described the top problems that they were experiencing at baseline and provided a 0–10 rating of current distress associated with that problem. A list of top problems identified by students in the current sample is included in Fig. 2. We used the distress rating provided at baseline as the subjective distress predictor variable in our aim 3 analyses. We retained the same top problem throughout the implementation and tracked distress related to this problem at mid-treatment and post-treatment.
To complete the second part of the measure, students used a 3-point scale to respond to 12 additional items assessing their internalizing and externalizing problems in the past week. Students responded to these same 12 items each week before the start of the therapy session. Subscales yielded fair internal consistency for internalizing problems (Cronbach’s α = .62, .76, .78) and externalizing problems (Cronbach’s α = 76, .66, .72) at the baseline, midpoint, and post assessments, respectively.
Research Design and Analytic Plan
A repeated measures design evaluated change during the open trial implementation, we measured symptoms at pre-treatment, mid-treatment, and post-treatment. Research assistants double entered all data and a third research assistant corrected entry discrepancies. Paired samples t tests examining pre-post change tested whether students experienced expected symptom reductions. Paired samples t tests examining change occurring from pre-to-mid and from mid-to-post determined which changes occurred in the early versus later parts of treatment. Given the multiple comparisons conducted to test these hypotheses, we presented the Bonferroni correction, a conservative strategy that accounts for multiple comparisons by setting a higher threshold for statistical significance. Finally, we examined whether bereavement and subjective distress at baseline predicted treatment response during the second half of treatment with a multiple linear regression where change in the second half of treatment was regressed onto the predictors bereavement (1 = yes bereaved, 0 = no bereaved) and baseline distress.
Results
Fidelity to the Treatment Model
Fidelity ratings of coded transcripts indicated excellent clinician adherence to the intervention manual across sessions. Clinicians covered 89.47% of all manual content.
Treatment Outcomes
The first goal of this study was to replicate and expand upon the two outcome studies (Langley et al., 2015; Santiago et al., 2018) that suggest that the Bounce Back program is beneficial. We expected PTS, internalizing problems, externalizing problems, and subjective distress to significantly decrease during youth’s participation in Bounce Back. Four paired samples t tests suggested that youth’s PTS, internalizing, externalizing, and distress decreased significantly from the beginning to the end of treatment (See Table 2 for details). Large standard deviations on clinical variables convey the range of severity of presenting difficulties among participants.
Timing of Symptom Reductions
The second goal of the study was to test whether symptoms changed in the first half of treatment, the second half of treatment, or during both halves of treatment. To test these questions, we broke the 10-session group treatment in half. The first half contained group sessions 1–5 and the second half contained sessions 6–10 as well as the individual trauma narrative sessions. We tested whether significant change occurred during the first half of treatment (before the trauma narrative) and during the second half of treatment.
Paired samples t tests compared baseline to midpoint and midpoint to endpoint scores for all outcomes (see Table 2 for details). PTS scores dropped significantly in the first half of treatment (t(17) = 3.46, p < 0.01, Cohen’s d = 0.82), but did not significantly change during the second half of treatment (t(17) = 1.04, p = 3.31, Cohen’s d = 0.24). Internalizing scores did not significantly change during the first half of treatment (t(18) = 1.89, p = 0.07, Cohen’s d = 0.18)) or during the second half of treatment (t(14) = 0.32, p = 0.75, Cohen’s d = 0.08)). Externalizing scores did not significantly change during the first half of treatment (t(18) = 1.76, p = 0.10, Cohen’s d = 0.33)) or during the second half of treatment (t(15) = 0.88, p = 0.39, Cohen’s d = 0.22)). Distress scores dropped significantly during the first half of treatment (t(16) = 3.41, p < 0.01, Cohen’s d = 0.47)), but did not significantly change during the second half of treatment (t(15) = 1.46, p = 0.16, Cohen’s d = 0.49).
To further understand PTS change at the individual level, we calculated the percent of the sample that fell below the clinical threshold (Evans, Margison, & Barkham, 1998), at midpoint and post treatment. This method takes into account the expected variability from the known clinical sample, and establishes a cutoff below which clinically significant change can be presumed to have occurred. For our PTS measure (the UCLA-R) a clinical threshold was calculated using data gathered in a validation of the measure from adolescents with a confirmed diagnosis of PTSD (Kaplow et al., 2019). At the beginning of treatment, 21% of students in the sample reported scores below the clinical threshold of 28. By midpoint in treatment, 42% of students in the sample reported scores below the clinical threshold, while at post-treatment 33% of students in the sample reported scores below the clinical threshold. Thus, some students reported a loss of initial treatment gains between session 5 and the end of treatment. For distress and secondary outcomes, we examined individual change by visual examination of spaghetti plots (Figs. 3 , 4, 5, 6), which suggested considerable variability in individuals’ responses to the second part of treatment.
Baseline Predictors of Symptom Reduction
A final aim of the study was to test whether bereavement and subjective distress assessed at baseline would predict change in PTS symptoms during the second half of treatment. Considering Layne et al. (2008) and Salloum and Overstreet (2012), we expected that bereavement and baseline distress would positively predict change in the second half of treatment, suggesting that those youth with heightened clinical needs would incrementally benefit from additional sessions that include the trauma narrative. We tested this hypothesis with a multiple linear regression where change in the second half of treatment was regressed onto the predictors bereavement (1 = yes bereaved, 0 = no bereaved) and baseline distress. The regression was not significant F(2,11) = 3.16, p = .08 with an adjusted R2 = .25.
Discussion
The aims of this study were to (1) replicate and extend literature suggesting that Bounce Back is helpful for trauma-exposed youth, (2) examine when symptom reduction occurred during an open trial of Bounce Back, and (3) test whether bereavement and subjective distress assessed at baseline predicted students’ PTS symptom reduction during the second half of treatment. As hypothesized, we found significant decreases in all assessed outcome variables (PTS, internalizing, externalizing, and top problem distressed) from the beginning to the end of treatment. Although the current study was not designed to test effectiveness or efficacy, the findings from this open-trial in the real world does further support previous evidence that Bounce Back is associated with decreased PTS and internalizing symptoms (Langley et al., 2015; Santiago et al., 2018). Furthermore, data from the current study builds upon existing studies by providing preliminary evidence that students participate in the full course of the Bounce Back program also experience decreases in externalizing symptoms and top problem distress. Externalizing symptoms are common among youth who have experienced trauma and change on this outcome may be particularly relevant in the school setting where disruptive behavior can impede multiple students’ educational experiences. Furthermore, the observation of change in distress related to targets that students’ themselves identified (e.g., “top problem”) offers assurance that the Bounce Back program is associated with change both on standard symptom measures and on targets that are personally meaningful to the students who are participating. Future studies may build on our results with randomized control designs that test whether observed change in externalizing problems and top problems distress is due to participation in the Bounce Back program or some other factor. Additionally, future studies should assess externalizing symptoms via reports from teachers or caregivers rather than relying exclusively on students’ self-reports.
Change During the First Half of Treatment
The current study’s open trial, repeated measures design was well suited to examine our second question about when change took place during the Bounce Back program. PTS symptoms, the main target of treatment, decreased significantly in the first part of treatment (sessions 1–5) and so did distress related to students’ top problems. These results join with outpatient psychotherapy research showing that most symptom reduction occurs in the early phases of treatment (Rubel, Lutz, & Schulte, 2015) and that PTS reductions, in particular, can occur after only a few sessions of CBT. For example, nearly half of the youth participating in individual CBT for PTSD responded to treatment after just four sessions, early response predicted superior treatment gains, and this early response was maintained across a 3 month follow up (Wamser-Nanney, Scheeringa, & Weems, 2016). Findings also support the idea that statistically significant reductions in PTS can occur without the trauma narrative (Deblinger et al., 2011; Layne et al., 2008; Salloum & Overstreet, 2012).
Taken together, these findings suggest that many youth experience PTS symptom reduction even before completing trauma narratives when participating in the Bounce Back program and similar CBTs. Accordingly, psychoeducational and skill building components of CBT should be regarded not just as pre-requisites for the trauma narrative, but as important therapeutic activities by which change in PTS can and does occur. This interpretation is consistent with the literature that suggests that trauma treatments for adults work through multiple mechanisms including (1) emotional processing of traumatic memories that is facilitated through exposure and/or (2) a shift in meaning of the traumatic events through cognitive processing. Importantly, Resick et al. (2008) found that trauma treatment with adults was equally effective when it included or omitted the writing/reading of a trauma account and existing research has supported cognitive change as a mechanism of change in PTSD treatment (McLean, Yeh, Rosenfield, & Foa 2015) for adults. Future research can build upon the current literature by testing whether cognitive change mediates PTS symptom reduction in youth participating in programs like Bounce Back. Such studies should also test whether processes that are inherent to good group therapy (e.g., improved feelings of connectedness, social bonding, decreased isolation) or whether aspects of group composition may also contribute to these positive outcomes.
Change During the Second Half of Treatment
Given that change in primary symptoms occurred during the first half of treatment for many of the youth in our sample, curiosity about the benefit of the second half of treatment is a logical next question. In our sample, we observed no significant change in primary and secondary symptoms from midpoint to the end of Bounce Back. This is particularly surprising given that the second half of treatment included not only the same number of group sessions as the first half but also included individual pull out sessions where trauma narratives were developed and processed. The small sample in the current study was underpowered to detect small effects that may have occurred during the second part of the program. Alternately, it could be that the second part of the program was not incrementally helpful to youth who had already experienced significant change in the first half. In fact, some students reported reductions of their initial treatment gains during the second half of treatment. This reduction of initial treatment gains (e.g., symptoms worsening from midpoint to post treatment) could suggest that a 10 session group treatment is not the best fit for all students. It may be that students who reported rapid gains met their treatment goals and no longer needed treatment. For these students, staying in group therapy may have had iatrogenic effects. Alternately, the loss of initial treatment gains may indicate that some students needed more sessions to fully process the trauma narrative. To address this interpretation, we offered students a list of school-based resources (e.g., contact information for the guidance counselor and a school-based social worker) as well as referrals to community providers at the end of the study. In future implementations, clinicians could use the midpoint assessment to determine whether expected treatment gains had been made and, if not, whether students could benefit from a higher level of care (e.g., individual treatment). Such an approach would help to tailor treatment to each student’s individual needs. A stepped care model for treating PTS has been shown to be as effective as individual TF-CBT and less expensive (Salloum et al., 2016).
Despite no significant change occurring during the second half of treatment, we did observe that statistically significant change on secondary outcomes (e.g., internalizing and externalizing problems) was not evident until the full course of treatment was completed.
It may be that youth need additional opportunities to practice CBT skills in the group order to show significant improvements in internalizing and externalizing problems. It also may be that these secondary symptoms responded sequentially to treatment because PTS symptoms and current distress needed to dissipate before youth could focus their attention on reducing internalizing and externalizing problems. Overall, the finding suggests that, while PTS symptoms decrease early on during treatment, a full course of Bounce Back is needed in order for youth to report statistically significant change in secondary outcomes like internalizing and externalizing problems.
Predictors of Change During the Second Half of Treatment
Understanding which students benefit from the second part of treatment that includes the trauma narrative will help in individualizing treatment so that it can be optimally helpful to all students who participate. Previous studies suggest that highly distressed youth (Salloum & Overstreet, 2012) and youth who are bereaved (Layne et al., 2008) may be a subset of trauma-exposed youth who experience incremental benefits from sessions that focus on trauma-narrative processing. Our data do not support these findings. We found that bereavement and distress assessed at baseline did not predict change during the second half of treatment. This result should be interpreted with caution as our small sample size was underpowered to detect small to moderate links.
Dose effects may also affect the response to treatment, particularly during the trauma 1–3 narrative sessions. Our study could not directly examine this dose effect due to several limitations. The sample size does not provide sufficient power to detect small to moderate effects of dose within a more complex statistical model which would be required to simultaneously analyze timing of change along with dose of individual sessions. Furthermore, because our study was based on data from a community implementation, rather than a rigorous research trial, number of individual sessions was not recorded consistently. While this is an acknowledged limitation, it is not uncommon for evidence-based models, including trauma treatment, to vary in number of sessions to allow flexibility in meeting client needs.
Individual-Level Change
In addition to understanding change in the group as a whole, it is important to understand change at the individual level. Existing research suggests that the process of change is not always linear (Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, 2007) and that individuals may follow different trajectories of change in therapy. Visual examination of individual trajectories showed that, across outcomes, during the first half of treatment, most students improved or stayed the same. However, there appeared to be considerable variability in the benefit of the second part of treatment for individual students (Figs. 3, 4, 5, 6). Rather than mostly improving, in the second half of treatment, some students some students reported continued gains, some reported maintenance of initial treatment gains, and some students reported a loss of initial treatment gains (i.e., lower PTS scores at mid treatment than at post treatment).”
Conclusions
To disseminate evidence-based treatments on a large scale and to advance science, the flow of information between research and practice should be bi-directional (Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014). Information from the current study provides important evidence from a real-world open implementation trial and attempts to answer a question that is relevant to clinicians implementing the program, “Can we expect to observe change if we implement a modified Bounce Back program?” Thus, current findings should be considered by program developers in terms of possible adaptations that could maximize uptake by systems, improve efficiency of our treatments, and increase students’ access to services. If current results are replicated with larger samples and more elaborate research designs, they may suggest that Bounce Back can be adapted to meet the preferences of the clinicians working in the organizations where they are being implemented. Specifically, schools that elect to implement only the first part of treatment may still expect to see significant PTS reductions among participating students. Clinicians should be cautioned, however, that modifying treatment in this way may reduce the likelihood of significant change in externalizing and internalizing difficulties, which required the full course of treatment in our sample.
Limitations and Future Directions
Results should be interpreted with caution given the limitations of this study. First, this open trial design precludes making inferences about whether Bounce Back (and its specific components) caused symptom reduction and, without a comparison group, we cannot rule out the interpretation that symptoms reduce naturally over time and results reflect “regression to the mean.” Still, the interpretation that change would have occurred without treatment is unlikely given the existing research that suggests that after the acute post trauma period, PTS symptoms persist (Hiller et al., 2016) or worsen overtime for trauma-exposed youth who do not receive treatment (Goenjian et al., 1997; 2020). We implemented Bounce Back in this Title I elementary school as an effort to extend clinical services to students who likely experienced barriers to accessing therapy in other settings, but we did not measure whether each student was engaging in other forms of therapy. Future dismantling studies should measure receipt of other clinical services and use randomization and comparison conditions to further assess which components of the Bounce Back program produce change, whether the program is equally effective at reducing PTS if program modifications are made, and whether secondary outcomes (internalizing and externalizing problems) significantly change if the program is modified.
Secondly, when interpreting the finding that PTS reductions occur before the trauma narrative, it is important to consider that the trauma narrative is only one of the exposure-based exercises introduced in the Bounce Back program. Our screening procedures ask children to recount details of a traumatic memory and the screening itself could be considered an exposure exercise. Furthermore, later in Bounce Back children engage in gradual exposure exercises as they take small steps towards achieving larger behavioral goals that may or may not be related to their traumatic experiences. Thus, results may indicate that PTS reduction is possible before a trauma narrative, but should not be interpreted to mean that the Bounce Back program would be effective at reducing PTS symptoms without exposure.
Finally, we should caution that our sample is underpowered to detect small effects and, so, the null results should be interpreted with caution. On one hand, the finding that significant reductions in internalizing and externalizing problems were not observed in either the first or second half of treatment alone could mean that these secondary symptoms take more time to respond to treatment that is designed to treat PTS. This idea would be consistent with the idea that PTS symptoms need to abate before youth can focus on other, related concerns. Alternately, it could be that these secondary symptoms do change during the entire course of treatment, but to a lesser extent than PTS symptoms and that these small effects could not be detected in our small sample. Furthermore, although we did not detect significant change in PTS symptoms during the second half of treatment, decisions about when to end treatment and whether the second half of treatment is necessary should be made on a case-by-case basis considering specifics of the presentation (e.g., level of secondary problems), client preferences, and goals of therapy. Our small sample size also precluded testing a wide range of other variables that could be related to treatment outcome. For example, in post hoc exploratory analyses, we examined age as a predictor of outcome and found no associations. Previous studies of the Bounce Back program (Langley et al., 2015; Santiago et al., 2018) do not test the potential impact of age on outcomes and cognitive developmental norms suggest that older children may benefit more from cognitive components of the program than younger children. Future studies should examine these questions in larger samples.
While the current study focused on length of treatment and clinicians’ discomfort as potential implementation barriers, there are other barriers that impede implementation of evidence-based treatments and these barriers should be further understood and addressed. For example, in our sample, several students qualified for treatment, but we were unable to reach their parents for permission to treat. It may be that parents preferred to seek treatment outside of the school setting or preferred not to seek treatment. We observed that, among students who qualified for treatment, PTS scores were slightly (although not significantly) higher among students whose parents could not be reached a second time for consent to treat than among the students whose parents consented to both screening and treatment. It is important for research review boards to carefully consider the consequences of requiring a second phase of consenting since this appears to presents a barrier to treatment, especially for the students with the highest levels of needs. Streamlining consent to screen and treat processes would help to ensure that youth who need treatment are able to access treatment. Additionally, implementation costs are a factor that limits the uptake of evidence-based therapies in school settings. We selected the Bounce Back program, in part, because training materials (e.g., training videos, a certification process, the treatment manual) are freely available online (www.bouncebackprogram.org). Still, our approach to symptom monitoring (a primary component of evidence-based practice) was costly. Measure administration costs must be seriously considered when determining whether evidence-based practices (which should include repeated symptom assessment) are scalable or feasible at all in under-resourced community settings and schools. To bridge the science-to-service gap, it is the responsibility of researchers to ensure that the products of their publicly-funded work are regarded as public property and freely available to community clinicians who need to use them. Future studies should build upon our results and address our limitations in order to facilitate data-based decision making about if and how to modify evidence-based programs for implementation in schools and other community settings.
References
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Center for Children, Youth and Families.
Alegría, M., Fortuna, L. R., Lin, J. Y., Norris, L. F., Gao, S., Takeuchi, D. T., et al. (2013). Prevalence, risk, and correlates of posttraumatic stress disorder across ethnic and racial minority groups in the US. Medical Care, 51, 1114.
Alisic, E., Zalta, A. K., Van Wesel, F., Larsen, S. E., Hafstad, G. S., Hassanpour, K., et al. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. The British Journal of Psychiatry, 204, 335–340.
Baglivio, M. T., Wolff, K. T., Epps, N., & Nelson, R. (2017). Predicting adverse childhood experiences: The importance of neighborhood context in youth trauma among delinquent youth. Crime & Delinquency, 63, 166–188.
Becker, C., Darius, E., & Schaumberg, K. (2007). An analogue study of patient preferences for exposure versus alternative treatments of posttraumatic stress disorder. Behaviour Research and Therapy, 45, 2861–2873.
Becker, C. B., Zayfert, C., & Anderson, E. (2004). A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy, 42, 277–292.
Cohen, J. A., Mannarino, A. P., & Deblinger, E. (Eds.). (2012). Trauma-focused CBT for children and adolescents: Treatment applications. New York: Guilford Press.
Copeland, W. E., Keeler, G., Angold, A., & Costello, E. J. (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64, 577–584.
Costello, E. J., Erkanli, A., Fairbank, J. A., & Angold, A. (2002). The prevalence of potentially traumatic events in childhood and adolescence. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 15, 99–112.
Costello, E. J., Sampson, N. A., Kessler, R. C., & Merikangas, K. (2014). Services for adolescents with psychiatric disorders: 12-month data from the National Comorbidity Survey-Adolescent. Psychiatric Services, 65, 359–366.
Daviss, W. B., Mooney, D., Racusin, R., Ford, J. D., Fleischer, A., & McHUGO, G. J. (2000). Predicting posttraumatic stress after hospitalization for pediatric injury. Journal of the American Academy of Child & Adolescent Psychiatry, 39, 576–583.
de Arellano, M. A., Lyman, D. R., Jobe-Shields, L., George, P., Dougherty, R. H., Daniels, A. S., et al. (2014). Trauma-focused cognitive-behavioral therapy for children and adolescents: Assessing the evidence. Psychiatric Services (Washington, D.C.), 65(5), 591–602. https://doi.org/10.1176/appi.ps.201300255.
Deblinger, E., Mannarino, A. P., Cohen, J. A., Runyon, M. K., & Steer, R. A. (2011). Trauma-focused cognitive behavioral therapy for children: Impact of the trauma narrative and treatment length. Depression and Anxiety, 28, 67–75. https://doi.org/10.1002/da.20744.
Dunn, E. C., Nishimi, K., Powers, A., & Bradley, B. (2017). Is developmental timing of trauma exposure associated with depressive and post-traumatic stress disorder symptoms in adulthood? Journal of Psychiatric Research, 84, 119–127.
Elhai, J. D., Layne, C. M., Steinberg, A. S., Vrymer, M. J., Briggs, E. C., Ostrowski, S. A., et al. (2013). Psychometric properties of the UCLA PTSD Reaction Index. Part 2: Investigating factor structure findings in a national clinic-referred youth sample. Journal of Traumatic Stress, 26, 10–18.
Evans, C., Margison, F., & Barkham, M. (1998). The contribution of reliable and clinically significant change methods to evidence-based mental health. Evidence Based Mental Health, 1, 70–72.
Feeny, N. C., Zoellner, L. A., Mavissakalian, M. R., & Roy-Byrne, P. P. (2009). What would you choose? Sertraline or prolonged exposure in community and PTSD treatment seeking women. Depression and Anxiety, 26, 724–731. https://doi.org/10.1002/da.20588.
Flay, B. R., Biglan, A., Boruch, R. F., Castro, F. G., Gottfredson, D., Kellam, S., ... & Ji, P. (2005). Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prevention Science, 6(3), 151–175.
Fong, K. (2019). Neighborhood inequality in the prevalence of reported and substantiated child maltreatment. Child Abuse and Neglect, 90, 13–21.
Ford, I., Racusin, J. D., Acker, R., Bosquet, R., Ellis, C., & Schiffman, R. (2002). Traumatic Events Screening Inventory (TESI-PRR/TESI-SRR).
Goenjian, A. K., Karayan, I., Pynoos, R. S., Minassian, D., Najarian, L. M., Steinberg, A. M., et al. (1997). Outcome of psychotherapy among early adolescents after trauma. American Journal of Psychiatry, 154, 536–542.
Goenjian, A. K., Steinberg, A. M., Walling, D., Bishop, S., Karayan, I., & Pynoos, R. (2020). 25-year follow-up of treated and not-treated adolescents after the Spitak earthquake: Course and predictors of PTSD and depression. Psychological Medicine, 1–13.
Hayes, A. M., Laurenceau, J. P., Feldman, G., Strauss, J. L., & Cardaciotto, L. (2007). Change is not always linear: The study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review, 27, 715–723.
Hembree, E. A., Foa, E. B., Dorfan, N. M., Street, G. P., Kowalski, J., & Tu, X. (2003). Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress, 16, 555–562.
Hiller, R. M., Meiser-Stedman, R., Fearon, P., Lobo, S., McKinnon, A., Fraser, A., et al. (2016). Research review: Changes in the prevalence and symptom severity of child post-traumatic stress disorder in the year following trauma—A meta-analytic study. Journal of Child Psychology and Psychiatry, 57, 884–898.
Imel, Z. E., Laska, K., Jakupcak, M., & Simpson, T. L. (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81, 394–404.
Jaycox, L. H., Cohen, J. A., Mannarino, A. P., Walker, D. W., Langley, A. K., Gegenheimer, K. L., et al. (2010). Children’s mental health care following Hurricane Katrina: A field trial of trauma-focused psychotherapies. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 23, 223–231.
Kaplow, J. B., Rolon-Arroyo, B., Layne, C. M., Rooney, E., Oosterhoff, B., Hill, R., et al. (2019). Validation of the UCLA PTSD reaction index for DSM-5: A developmentally informed assessment tool for youth. Journal of the American Academy of Child and Adolescent Psychiatry, 59(1), 186–194.
Kataoka, S. H., Zhang, L., & Wells, K. B. (2002). Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. The American Journal of Psychiatry, 159, 1548–1555.
Langley, A. K., Gonzalez, A., Sugar, C. A., Solis, D., & Jaycox, L. (2015). Bounce back: Effectiveness of an elementary school-based intervention for multicultural children exposed to traumatic events. Journal of Consulting and Clinical Psychology, 83, 853.
Langley, A. K., Nadeem, E., Kataoka, S. H., Stein, B. D., & Jaycox, L. H. (2010). Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health, 2, 105–113.
Layne, C. M., Saltzman, W. R., Poppleton, L., Burlingame, G. M., Pašalić, A., Duraković, E., et al. (2008). Effectiveness of a school-based group psychotherapy program for war-exposed adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 1048–1062.
Lyon, A. R., & Bruns, E. J. (2019). From evidence to impact: Joining our best school mental health practices with our best implementation strategies. School Mental Health, 11, 106–114.
McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A., & Kessler, R. C. (2012). Childhood adversities and first onset of psychiatric disorders in a national sample of adolescents. Archives of General Psychiatry, 69, 1151–1160.
McLaughlin, K. A., Koenen, K. C., Hill, E., Petukhova, M., Sampson, N. A., Zaslavsky, A., et al. (2013). Trauma exposure and posttraumatic stress disorder in a US national sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 815–830. https://doi.org/10.1016/j.jaac.2013.05.011.
McLean, C. P., Yeh, R., Rosenfield, D., & Foa, E. B. (2015). Changes in negative cognitions mediate PTSD symptom reductions during client-centered therapy and prolonged exposure for adolescents. Behaviour Research and Therapy, 68, 64–69.
Nixon, R. D. V., Sterk, J., & Pearce, A. (2012). A randomized trial of cognitive behavior therapy and cognitive therapy for children with posttraumatic stress disorder following single-incident trauma. Journal of Abnormal Child Psychology, 40, 327–337.
Olatunji, B. O., Deacon, B. J., & Abramowitz, J. S. (2009). The cruelest cure? Ethical issues in the implementation of exposure-based treatments. Cognitive and Behavioral Practice, 16, 172–180.
Onken, L. S., Carroll, K. M., Shoham, V., Cuthbert, B. N., & Riddle, M. (2014). Reenvisioning clinical science: Unifying the discipline to improve the public health. Clinical Psychological Science, 2, 22–34. https://doi.org/10.1177/2167702613497932.
Ribbe, D. (1996). Psychometric review of Traumatic Event Screening Instrument for Children (TESI-C). In B. H. Stamm (Ed.), Measurement of stress, trauma, and adap- tation (pp. 144–151). Lutherville, MD: Sidran Pres.
Resick, P. A., Galovski, T. E., Uhlmansiek, M. O., Scher, C. D., Clum, G. A., & Young-Xu, Y. (2008). A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology, 76, 243–258.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41, 71–83. https://doi.org/10.1017/S0033291710000401.
Rolfsnes, E. S., & Idsoe, T. (2011). School-based intervention programs for PTSD symptoms: A review and meta-analysis. Journal of Traumatic Stress, 24, 155–165.
Rubel, J., Lutz, W., & Schulte, D. (2015). Patterns of change in different phases of outpatient psychotherapy: A stage-sequential pattern analysis of change in session reports. Clinical Psychology & Psychotherapy, 22, 1–14.
Salloum, A., & Overstreet, S. (2012). Grief and trauma intervention for children after disaster: Exploring coping skills versus trauma narration. Behaviour Research and Therapy, 50, 169–179. https://doi.org/10.1016/j.brat.2012.01.001.
Salloum, A., Wang, W., Robst, J., Murphy, T. K., Scheeringa, M. S., Cohen, J. A., et al. (2016). Stepped care versus standard trauma-focused cognitive behavioral therapy for young children. Journal of Child Psychology and Psychiatry, 57, 614–622.
Sanchez, A. L., Cornacchio, D., Poznanski, B., Golik, A. M., Chou, T., & Comer, J. S. (2018). The effectiveness of school-based mental health services for elementary-aged children: A meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 57, 153–165.
Santiago, C. D., Raviv, T., Ros, A. M., Brewer, S. K., Distel, L. M. L., Torres, S. A., et al. (2018). Implementing the Bounce Back trauma intervention in urban elementary schools: A real world replication trial. School Psychology Quarterly, 33, 1–9.
Schwartz, A. C., Bradley, R. L., Sexton, M., Sherry, A., & Ressler, K. J. (2005). Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatric Services, 56, 212–215. https://doi.org/10.1176/appi.ps.56.2.212.
Steinberg, A. M., Brymer, M., Decker, K., & Pynoos, R. S. (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports, 6, 96–100.
Steinberg, A. M., Brymer, M. J., Kim, S., Ghosh, C., Ostrowski, S. A., Gulley, K., et al. (2013). Psychometric properties of the UCLA PTSD Reaction Index: Part I. Journal of Traumatic Stress, 26, 1–9.
Stirman, S. W., Calloway, M. A., Toder, M. K., Miller, M. C. J., DeVito, M. A. K., Meisel, M. S. N., et al. (2013). Modifications to cognitive therapy by community mental health providers: Implications for effectiveness and sustainability. Psychiatric Services, 64, 1–6.
Tarrier, N., Liversidge, T., & Gregg, L. (2006). The acceptability and preference for the psychological treatment of PTSD. Behaviour Research and Therapy, 44, 1643–1656.
van Minnen, A., Hendriks, L., & Olff, M. (2010). When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behaviour Research and Therapy, 48, 312–320.
Wamser-Nanney, R., Scheeringa, M. S., & Weems, C. F. (2016). Early treatment response in children and adolescents receiving CBT for trauma. Journal of Pediatric Psychology, 41, 128–137.
Weisz, J. R., Chorpita, B. F., Frye, A., Ng, M. Y., Lau, N., Bearman, S. K., et al. (2011). Youth Top Problems: using idiographic, consumer-guided assessment to identify treatment needs and to track change during psychotherapy. Journal of consulting and clinical psychology, 79, 369–380.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
We would also like to acknowledge the contributions of our research assistants at West Chester University of Pennsylvania and University of Delaware, our collaborators within the Red Clay Consolidated School District, and, most importantly, our participants whose perseverance inspires us. A Delaware Department of Education Grant to the Red Clay Consolidated School District funded this work.
Rights and permissions
About this article
Cite this article
Grassetti, S.N., Haut, B., Beveridge, R.M. et al. When Do Posttraumatic Stress and Related Problems Abate During School-Based Group Therapy for Elementary Students?. School Mental Health 12, 689–702 (2020). https://doi.org/10.1007/s12310-020-09377-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12310-020-09377-8