Abstract
Monomorphic epitheliotropic T-cell lymphoma (MEITL) of gastrointestinal tract is an aggressive T-cell lymphoma that can rarely involve the brain. We present detailed descriptions of clinical and autopsy neuropathological findings of a rare case of an elderly woman who had surgery and chemotherapy for MEITL of the small intestine. Following her surgery, she progressively exhibited neurologic decline towards the end of her treatment. The patient eventually succumbed to her illness and was found to have MEITL with intracranial involvement on autopsy. Brain autopsy was performed and examination of tissues with hematoxylin–eosin staining under optical microscopy with 100 X magnification. Immunostaining for CD3, CD4, CD5, CD7, CD8, CD56, CD20, beta-amyloid, c-Myc, TCR-beta, TCR-delta, and EBER-ish was conducted on the formalin-fixed paraffin-embedded (FFPE) brain tissues. A neuropathological exam revealed multifocal friable necrotic and hemorrhagic areas in the supratentorial region. Histologically, monotonous small to medium-sized atypical lymphocytes infiltrated the brain parenchyma, prominently around the vessels. The immunophenotype of the atypical lymphocytes was positive for CD-3, CD-7, and CD-56 and negative for CD-5, CD-4, CD-8, CD-20, and c-Myc. EBER-ish was negative. The histology and immunophenotype confirmed the MEITL brain involvement. Neurologic decline and cognitive changes in patients with known MEITL can be the first clue of brain involvement upon which prompt evaluation is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monomorphic epitheliotropic intestinal T-cell lymphoma (MEITL), formerly known as type II enteropathy-associated T-cell lymphoma (EITL type II), is a rare aggressive primary intestinal T cell lymphoma that can rarely involve the brain [1]. Neuropathological manifestation of MEITL involvement can include neurologic symptoms such as focal motor deficits, cognitive decline, headache, and seizure [2]. Here, we describe a detailed case of METL with brain involvement along with descriptions of clinical and autopsy neuropathological findings.
Case report
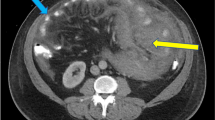
This is a case of a 72-year-old African American woman with a history of remote breast cancer treated by radiotherapy and monomorphic epitheliotropic T-cell lymphoma (MEITL) of the small intestine. About sixteen months ago before her death she presented with abdominal pain, nausea and vomiting, and unintentional weight loss and was found to have small bowel obstruction secondary to a jejunal mass. She had a small bowel resection with jejunojejunostomy at an outside hospital. The jejunal mass was diagnosed as MEITL with an immunohistochemical profile showing atypical lymphocytes that are positive for CD3, CD56, CD8 (variable), beta-F1 (variable), TIA, granzyme B, and perforin (subset), while negative for CD5, CD4, CD30, CD10, BCL6, TCR-delta, ALK, and EBER-ish. PCR for TCR gamma and beta were negative by outside consult. Staging PET/CT after surgery showed widely disseminated diseases involving lungs, liver, pancreas, other portions of the bowel, adnexa, and peritoneum. The patient was seen in our facility one month later for interventional radiology guided needle biopsy of right upper quadrant peritoneal mass which showed T cell lymphoproliferative disorder with similar immunophotype: positive for CD3 with partial loss of CD5, CD4, and CD8 and negative for CD10 and CD30 with Ki67 rate about 40–50% and compatible with her recent diagnosis of MEITL. Immunostains performed were limited due to insufficient sample. She subsequently received chemotherapy and was told by her primary care physician her lymphoma was in remission. Towards the end of her treatment, six months after her initial diagnosis of MEITL, she began to have cognitive decline with dementia symptoms. Additionally, she experienced a traumatic fall that led to bilateral hip and spinal fractures and has lived in a nursing home since then. She was initially diagnosed with encephalopathy with features suggestive of autoimmune encephalopathy which responded to steroid treatment. However, her neurologic status declined, resulting in multiple admissions for altered mental status, hypothermia, and hypotension. Brain MRI showed an enhancing lesion in the right cavernous sinus and other changes possibly representing CNS lymphoma (Fig. 1). A brain biopsy was performed in an outside institution that only revealed amyloid angiopathy. Her neurological status kept declining, and eventually, she succumbed to her illness eleven months after her neurological presentation. Autopsy was performed and confirmed the brain involvement by a patient’s known history of MEITL. No reoccurrence of primary intestinal MEILT was found in the abdominal organs including remaining the bowels, liver, pancreas, adnexa, or peritoneum or in the lungs.
Axial FLAIR MRI demonstrating expansile bilateral areas of abnormal signal intensity in the region of the nucleus accumbens (blue arrows) and external/extreme capsules (red arrows) (A). Coronal T2-weighted MRI demonstrating areas of abnormal signal intensity in the subcortical (green arrows) and subinsular (yellow arrows) white matter (B)
Materials and methods
Brain autopsy was performed and histological examination of tissues with hematoxylin–eosin (H&E) staining under optical microscopy with 4 × to 400 × magnification. Immunostaining for CD3, CD4, CD5, CD7, CD8, CD56, CD20, beta-amyloid, c-Myc, TCR-beta, TCR-delta, and EBER-ish was conducted on the formalin fixed paraffin embedded (FFPE) brain tissues. All antibodies for immunophenotyping are obtained from Roche Ventana Medical Systems (Tucson, AZ) and performed on Ventana XT instrument according to standard recommended protocols for each antibody. TcR-beta and TcR-delta immunostains were performed at Mayo Clinic Medical Laboratory (Rochester, MN) and interpreted at Downstate Medical Center.
Results
The patient’s brain weighs 1340 g. It was roughly symmetrical and of the usual external configuration. Coronal sections of the cerebrum revealed multifocal friable necrotic and hemorrhagic areas (Fig. 2) involving the left anterior medial frontal lobe, cingulate cortex, left inferior medial temporal lobe including hippocampus/entorhinal cortex, left basal ganglia, right frontal pole, and right insular cortex. In addition, a 2 × 1 cm mass encasing the right carotid artery was identified with a homogenous gray-white cut surface. Microscopically, the hemorrhagic and necrotic areas showed dense infiltration of monotonous small to medium-sized atypical lymphocytes in the brain parenchyma and perivascular space. These necrotic areas contain various amounts of macrophages, granulation tissue, and reactive gliosis (Fig. 3A, B). These atypical lymphocytes are positive for CD3, CD7, granzyme B, and TIA-1, focally and weakly positive for CD56 while negative for CD4, CD5, CD8, CD20, c-Myc, and EBER-ish. The immunohistochemical stains for TcR delta and TcR beta are negative indicating tumor cells with silent T cell receptor expression for both alpha/beta and gamma/delta subunits (Fig. 3C–K). The overall morphology and immunophenotypic findings are similar to the patient’s previously diagnosed MEITL of the jejunal mass and right upper quadrant peritoneal mass as described above. Sections from the grossly unremarkable cerebral lobes also displayed patchy perivascular infiltration of similar atypical lymphocytes with microinfarctions and reactive gliosis.
Autopsy neuropathological examinations showed a patchy hemorrhagic area at the left inferior temporal lobe (A, red arrow) and mildly dilated aqueduct with brown discoloration (A, green arrow). Coronal sections disclose multiple friable necrotic and hemorrhagic areas involving left anterior medial frontal/cingulate cortex (B, red arrow), left basal ganglia (C, green arrow), subcortical white matter of right insular cortex (C, red arrow), and left inferior medial temporal lobe involving hippocampus/entorhinal cortex (D, red arrow) and right frontal pole
Histomorphologic features and immunophenotype of MEITL with brain involvement. The H&E stain shows diffuse infiltration of brain parenchyma of atypical lymphocytes that also surrounds the vessels. It has patchy areas of necrosis (A, 100x). The atypical lymphocytes are monotonous small to medium-sized lymphocytes (B, 400x). The atypical lymphocytes are diffusely positive for CD3 (C,100x) and CD7 (D,100x); and most express cytotoxic markers, granzyme B (E, 200x) and TIA-1 (F, 100x). The atypical lymphocytes are negative for CD5 (G, 100x), CD4 (positivity in the figure is staining of background histiocytes and macrophages) (H, 100x), CD8 (I,100x), TcR beta (J, 200x), TcR delta (K, 200x), c-MYC, or EBER-ish
In addition, cerebral amyloid angiopathy was identified in many small and medium blood vessels in the meninges and superficial cortex including the hemorrhagic and necrotic areas. They are positive for beta-amyloid by immunohistochemical stain (Fig. 4A). Frequent diffuse amyloid plaques and moderate neuritic plaques are present in the frontal, temporal, occipital cortices and CA regions (Fig. 4B). Tau immunostain highlights neurofibrillary tangles in the temporal, entorhinal cortex, and CA regions, but not in the frontal or occipital cortex. The above findings are consistent with an intermediate level of Alzheimer’s disease-associated neuropathological changes. The lesion in the right cavernous sinus encasing the carotid artery was a benign meningioma exhibiting typical meningothelial cell proliferation.
Discussion
The most common location is the small intestine, as seen in this patient, but it can also be seen in the duodenum, stomach, and colon. The other areas it can spread to are the lungs and skin [1]. The rare occurrence of brain involvement has been described by a few case reports (Table 1); but to our knowledge, the descriptions of gross appearance and histopathological and immunohistochemical features of brain involvement of this entity are still limited. MEITL is more prevalent among Asian and Hispanic descent and is usually not associated with celiac disease [1, 3, 8]. To the best of our knowledge, five cases of MEITL with intracranial involvement have been reported, all of which were published in Asia and assumed to be described in patients of Asian descent (Table 1). Thus far, this is the first case report of MEITL with brain involvement in a patient of African descent. The incidence of this disease is still unknown for this ethnicity [9].
The patient presented with a cognitive decline associated with dementia symptoms towards the end of her chemotherapy suggesting possible brain involvement. The presentations are consistent with other previously reported T-cell lymphoma involving the central nervous system (CNS). In a case series described by Gandhi et al., they identified 12 peripheral T-cell lymphoma (PTCL) with CNS involvement in their institution from 2000 to 2019 and found that all patients presented with neurologic symptoms such as focal motor deficits, cognitive decline, headache, and seizure [2]. Similarly, the case report and review of literature by Chuah et al. reported that patients with EATL/MEITL that involves the supratentorial area of the brain presented with altered mental status, headache, and weakness while the patient who had an infratentorial spread presented with ataxia and slurred speech [3]. Other neurologic presentations reported were rapid progressive mental deterioration, leg paralysis, and facial paralysis [4,5,6]. The multifocal widespread of MEITL in multiple brain cortices and deep grey matter of our patient is likely the reason for the rapid progressive deterioration of her neurologic functions. Her rapid cognitive decline and dementia symptoms most likely contribute to disease progression of MEITL involving the hippocampus and frontotemporal lobes and her intermediate level of Alzheimer’s neuropathologic changes. Approximately 11 months after her first notable neurologic symptoms, the patient succumbed to her illness and died. The aggressive behavior of PTCL involving the CNS was also noted in the case series by Ghandi et al. wherein their median overall survival from the time of diagnosis is 16 months (95% CI: 2.8–173) [2]. Most of the case reports reviewed with intracranial involvement of MEITL reported similar aggressive behavior seen with our patient leading to demise a few months after the initial presentation of brain involvement [3,4,5]. Henceforth, periodic assessment of cognition and neurologic function in patients with MEITL is suggested to promptly recognize and properly assess intracranial involvement.
To our knowledge, there is no current literature that describes the gross pathological changes that can occur to the brain with intracranial MEITL. The presence of multifocal gross hemorrhages and friable necrosis seen in our patient correlates well with the known usual microscopic findings seen in this entity. The histopathologic characteristics and immunophenotypic profile in the small intestine and brain of our case are similar to the classic MEITL described by WHO Classification of Tumors, 5th ed [1]. They consisted of small to medium-sized, monomorphic atypical lymphocytes infiltrating the brain parenchyma, most prominent in perivascular areas, and associated with patchy necrosis, hemorrhages, reactive gliosis, and granulation tissue. The immunophenotypic profile of the atypical lymphocytes are as follows: positive for CD3 and CD7; weakly positive for CD56; and negative for CD4, CD5, CD8, CD20, TcR-beta, TcR-delta, and c-Myc. Cytotoxic marker expression of TIA-1 and granzyme B are noted as well. In situ hybridization for Epstein-Barr virus (EBER-ish) is negative confirming that this lesion was not associated with EBV. The immunohistochemical profile of the brain lesion corresponded with the primary tumor in the small intestine. Other case reports of MEITL with extranodal involvement also had a similar immunophenotype as the original tumor [4,5,6]. A case report by Suzuki et al. reported a lung biopsy that was re-evaluated after MEITL of the small intestine was diagnosed. They found that the lung harbored the same malignant lymphocytes using immunohistochemical stains [7]. The monotonous nature of the neoplastic cells can pose possible difficulty in recognizing them in biopsy samples, especially if the patient has no known history of MEITL. The brain biopsy of our patient done at an outside institution only showed that the amyloid angiopathy was probably due to the sampling limitation innately seen in biopsy procedure and the patchy distribution of the tumor cells seen in this disease [10].
Diffuse cerebral amyloid angiopathology (CAA) is also identified in this patient which might be an age-related finding. Although CAA itself may be associated with cerebral hemorrhages, infarction, and CAA-related inflammation or vasculitis, the inflammatory lymphocytic responses in CAA are usually vascular-centric or perivascular and not the dense sheets of monotonous atypical lymphocytes in brain parenchyma seen in this case [11]. The CAA-related reactive lymphocytes generally show CD3 + , CD4 + , CD8 + , and CD5 + which are different from this case which shows loss of CD5.
Conclusion
Monomorphic epitheliotropic T-cell lymphoma is an aggressive hematolymphoid malignancy that can rarely involve the brain. A patient with a history of MEITL that presents with cognitive changes, neurologic decline, and even Alzheimer’s Disease type presentation may suggest intracranial involvement and warrants prompt evaluation. However, despite early suspicion or discovery of extranodal organ involvement, the prognosis of the disease is still poor due to the lack of effective therapy at this time.
Data availability
The authors confirm that all data generated or analyzed during this study are included in this published article.
References
Chan J et al (n.d.) Monomorphic epitheliotropic intestinal T-cell lymphoma. Hematolymphoid Tumours (5th ed.). WHO Classification of Tumours online. https://tumourclassification.iarc.who.int/chaptercontent/63/225. Accessed 11 Oct 2022
Gandhi S et al (2019) Central nervous system involvement in peripheral T-cell lymphoma. Blood 134(Supplement_1):5293. https://doi.org/10.1182/blood-2019-131965
Chuah YY et al (2020) Enteropathy-associated T-cell Lymphoma (EATL) with intracranial metastasis: a rare and dismal condition. Acta Gastro-Enterolofica Belgica 83:77–80
Nishida H et al (2015) Isolated central nervous system relapse in type II enteropathy-associated T cell lymphoma. Rinsho Ketsueki 55(6):692–698. https://doi.org/10.11406/rinketsu.56.692
Morimoto A et al (2021) Monomorphic epitheliotropic intestinal T-cell lymphoma invades the brain. Internal Med 60(5):815–816. https://doi.org/10.2169/internalmedicine.5925-20
Kubota, Y et al (2018) Monomorphic epitheliotropic intestinal T-cell lymphoma involving the central nervous system. American Society of Hematology. Image Bank. https://imagebank.hematology.org/image/61420/monomorphic-epitheliotropic-intestinal-tcell-lymphoma-involving-the-central-nervous-system. Accessed 14 Nov 2022
Suzuki Y et al (2020) Monomorphic epitheliotropic intestinal T-cell lymphoma involving the lung and brain: a rare case stud. Internal Med 59(20):2559–2563. https://doi.org/10.2169/internalmedicine.4710-20
Chen C et al (2021) Clinicopathological and molecular genomic features of monomorphic epitheliotropic intestinal T-cell lymphoma in the Chinese population: a study of 20 cases. Diagnostic Pathol 16:114. https://doi.org/10.1186/s13000-021-01173-5
Fisher A et al (2019) Truth lies below: a case report and literature review of typical appearing polyps yet with an atypical diagnosis. World J Gastrointest Endosc 11(1):54–60. https://doi.org/10.4253/wjge.v11.i1.54
Hall W et al (2001) Improving diagnostic yield in brain biopsy: coupling spectroscopic targeting with real-time needle placement. J Magn Reson Imaging. 13 (1). https://doi.org/10.1002/1522-2586(200101)13:1<12::AID-JMRI1002>3.0.CO;2-Q
Eng JA et al (2004) Clinical manifestations of cerebral amyloid angiopathy-related inflammation. Ann Neurol 55:250–325
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This is an observational study. The SUNY Downstate Research Ethics Committee has confirmed that no ethical approval is required.
Informed consent
For this type of study, formal consent is not required.
Consent for publication
Consent for publication was obtained for every individual person’s data included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Talabong, D.J.A., Laguerre, E., Chen, N.N. et al. Monomorphic epitheliotropic intestinal T-cell lymphoma involving the central nervous system: a rare case report with comprehensive autopsy neuropathological examinations. J Hematopathol 16, 155–160 (2023). https://doi.org/10.1007/s12308-023-00557-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12308-023-00557-4