Abstract
Objectives
This study was designed to evaluate, compare the mid-term functional outcome of revision anterior cruciate ligament reconstruction (ACLR) using different autografts and assess the cause of failure of primary ACLR in an Omani population with kneeling customs.
Materials and methods
Patients with failed primary ACLR who underwent revision ACLR using autografts were included in this retrospective study. The cause of primary ACLR failure and the functional outcome was assessed using the Tegner-Lyholm knee score and compared among bone patella tendon-bone (BPTB), quadriceps tendon (QT), semitendinosus gracilis (STG) autografts used.
Results
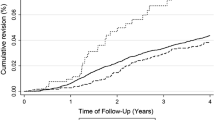
One hundred two patients (102 male) were included in the study with a minimum follow-up of 2 years. Thirty-one patients underwent revision with BPTB, 34 with STG and 19 with QT autografts. Majority of the patients (70.23%) achieved good-to-excellent functional outcome based on their Tegner–Lysholm scores. The functional outcome of different autografts was comparable to each other based on Kruskal–Wallis test. The causes of primary ACLR failure were failure due to trauma in 58.33% of patients, technical failure in 22.61% of patients, and nontraumatic failure in 19.04% of patients.
Conclusions
The functional outcome of revision ACLR in this Middle Eastern Asian Omani population was good-to-excellent, with the patients experiencing no difficulty in performing activities of daily living, including kneeling activities. The outcome of different autografts, BTPB, QT, STSG is similar in high knee flexion patients with no autograft found to be superior. The findings of this study add to the literature on functional outcomes after primary and revision ACLR in a customary kneeling population.
Level of evidence III
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) injuries are one of the most common lower limb injuries, with about 1 million ACL injuries recorded annually worldwide [1]. According to the literature, 5.4% of all ACL reconstruction (ACLR) patients undergo revision surgery within 5 years, with revision surgery accounting for 10% of the total number of ACLRs performed [2, 3]. With an increase in the number of people pursuing an active lifestyle, there is greater demand for an improved quality of life and satisfaction post revision ACLR. However, as shown in previous studies, the results of revision ACLR are poor compared to those of primary ACLR [4, 5]. In a systematic review of the Scandinavian knee ligament register, Hamrin et al. [6] reported significantly low clinical scores and poor patient-reported quality outcomes after revision ACLR. Their findings were similar to those of Kvist et al. [7] whose study was based on the Swedish national anterior cruciate register. Although previous studies have analyzed the outcome of revision ACLR in populations with non-kneeling customs, no studies have focused on populations with kneeling customs, where high knee flexion is required [4,5,6,7].
Kneeling is defined as a position where at least one knee is in contact with some part of the environment, usually the ground, and body weight is supported predominantly by the knee or knees [8]. Kneeling is common in Asian society. Kneeling with the knees fully flexed (i.e., 150–165 degrees) is important in Middle eastern countries for religious and cultural customs [9, 10]. Thus, it is important to assess functional outcomes after revision ACLR in populations with kneeling customs requiring high knee flexion.
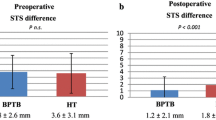
Autografts, especially bone patella tendon-bone (BPTB), are known to be associated with an increased incidence of kneeling pain and anterior knee pain, as highlighted in a systemic review of primary ACLR, as are quadriceps tendon (QT) autografts [11, 12]. Kneeling difficulty with a semitendinosus gracilis (STG) autograft was recently reported, with 77% of patients experiencing kneeling difficulty 1 year post-ACLR and 54% experiencing kneeling difficulty 2 years post-ACLR [13]. There are no studies on the ideal autograft for revision ACLR in this kneeling subset of patients.
The purpose of this study was as follows: (1) to assess the mid-term functional outcome and identify the ideal autograft for revision ACLR in patients with kneeling customs and (2) to analyze the cause of primary ACLR failure in an Omani population.
Materials and methods
This retrospective observational study uses the data of patients who were operated for arthroscopic revision ACLR between 2015 and 2018 at our tertiary care center under the care of two experienced knee surgeons. Patients who underwent revision ACLR using autografts with a minimum follow-up of 2 years were included in the study. Subjects with inflammatory diseases, coexisting multi-ligament injuries, lower limb mal-alignment same or contralateral side, those who underwent concomitant ligamentous reconstruction or alignment correction surgery were excluded. Failure due to infection requiring revision surgery was also excluded. The patients who underwent more than one revision, meniscal repair or previous lower limb surgeries were not included in the study.
Our institutional review board (IRB.KH:7318-2567-26) approved the study and waived the requirement for informed consent because it was a retrospective study using existing medical records and posed a minimal risk to the patients.
The data regarding primary ACLR failure were retrieved from the hospital medical records. Reoccurring instability after primary ACLR was evaluated by clinical test and neograft failure confirmed radiologically using magnetic resonance imaging (MRI). The surgical details and the cause of autograft failure were based on a review of the medical records. Onset of instability preceding or after trauma was noted. Data on the chondral grade of the articular surfaces according to the Outerbridge classification system, meniscal status, condition of the primary graft, type of revision graft, and thickness of revision grafts were obtained from the patients’ records. The chondral grade was based on the highest recorded score for each of the knee compartments. The Tegner–Lysholm knee score was used to assess the functional outcome at 2 years following the revision surgery by an orthopedician who was not involved in the surgical management of these patients. In total, 102 patients later underwent revision ACLR with STG, BPTB, or QT autografts, of these, 84 patients were included in the final study. Three patients excluded as they were re-revision ACLR, one patient excluded because of infection, and 14 patients were lost to follow-up.
Surgical technique
All the patients underwent revision ACL reconstruction using autografts either STG, BPTB, or QT. All surgeries performed using all endoscopic, arthroscopic-assisted with femoral tunnel drilled using trans-portal technique. Fixation of all patellar tendon grafts was with interference screw. Hamstring and Quadriceps fixation was variable, with staple, interference screw, and endobutton techniques utilized.
Rehabilitation
Subjects in the study underwent a common institutional rehabilitation protocol post the revision ACLR. All the groups of patients were allowed full passive range of motion after surgery. Early emphasis was placed on patellar and extensor mechanism mobility to prevent stiffness and scarring. Physical therapy commenced 24 h after surgery to gain early range of motion and muscle reactivation and to control edema. Rehabilitation included straight-leg raises in an immobilizer until the patient was able to perform them without any extension lag.
Partial weight bearing allowed for 2 weeks with general weight bearing at 6 weeks. Squats and single leg exercises were started at 8 weeks, with supervised sports specific exercises at 20 weeks after the quadriceps strength normalized.
Clearance for full competitive activity was based on a successful completion of knee sports test at 6 months postoperatively.
Statistical analysis
The Statistical Package for Social sciences, version 22 software was used for statistical analysis of the data. Continuous variables were given as mean, standard deviation and nominal variable as number. To compare the functional outcome using the different autografts, the Kruskal–Wallis test was applied, with a p value ≤ 0.05 considered significant.
Results
All the 84 patients in this study were male of average age 29 years (std. dev ± 8.4). Seventy-seven characteristics are presented in Table 1. The right knee was affected in 54 patients (64.28%), and the left knee was affected in 30 (35.71%) patients. The mean gap between the primary and revision surgeries was 54.7 months (range: 9–228 months) (Table 1). The minimum follow-up time in this study was 2 years (range: 2–5 years). BPTB was the thickest at followed by QT and STSG thinnest. Majority had had medial meniscal tear (35.7%), lateral meniscal tear (10.7%) of which 15.4% (6) underwent partial meniscectomy and rest meniscal debridement.
The distribution of autografts used in primary ACLR was majorly STG autograft in 75 (89.28%) cases and BPTB autograft in 9 (10.71%) cases. The causes of failure were defined as traumatic (n = 49, 58.33%), technical (n = 19, 22.61%), and nontraumatic (n = 16, 19.04%) (Table 2). Contact sport was the most common cause of traumatic failure, with 81.6% reporting that the trauma occurred while playing football. Tunnel malposition, endo button failure, and technique-related errors were considered technical failures. In this regard, there was one case of endo button pull-out, and 18 patients had tunnel malposition warranting revision of the femoral tunnel (Table 2). All the patients underwent single-stage revision ACLR, with tunnel revision performed in 18 (21.6%) patients. Nontraumatic failure was defined as a complaint of knee instability, with no history of significant preceding trauma. All the patients with nontraumatic failure complained of knee instability less than 1-year post-ACLR revision.
The most commonly used autograft for revision ACLR was an STG graft (40.47%) with a mean thickness of 8.4 ± 0.8 mm, followed by a BPTB graft (36.9%) at 9.8 ± 0.7 mm and QT graft (22.61%) at 9.6 ± 0.8 mm (Table 2). The Tegner–Lysholm score was excellent in 54.76% of patients, good in 15.47% of patients, fair in 11.90% of patients, and poor in 13.09% of patients (Table 3). The mean Tegner–Lysholm score was 85.08 (std. dev ± 16.04) (Table 4). Statistical analysis with Kruskal–Wallis test showed that there was no significant difference between the functional outcomes using different autografts (p = 0.86) (Table 4).
Discussion
To the best of our knowledge, this study is the first to investigate the functional outcome after revision ACLR and the factors affecting revision ACLR in a Middle Eastern Asian Omani population with kneeling customs. This population performs high flexion knee functional activities, such as kneeling, squatting for prayers, and social customs, for prolonged durations. An individual following Islamic practices is expected to pray five times a day and may regularly flex their knees as often as 70 times per day, with their knees fully flexed up to 150–165 degrees [9, 10, 14]. This degree of flexion exceeds that found in population without kneeling customs by an average of 15 degrees [9, 10, 14]. Sustained deep knee flexion is proved to cause functional joint instability and manifest as altered knee kinematics [15]. Native ACL, even though when relaxed in flexion is demonstrated to develop ligament creep during kneeling resulting in structural changes to its viscoelastic nature [15]. Thus, in a kneeling population, we believe the neograft would be at an increased risk of failure compared to the native ACL due to the ongoing ligamenatization and revascularization.
In our study, most of the patients (70.23%) reported a good-to-excellent functional outcome. None of the patients reported any difficulties performing routine activities of daily living, including kneeling. The mean Tegner–Lysholm score of 85.08 at 2-year postoperatively was consistent with that reported in earlier studies on subjects with non-kneeling customs. Boyle et al. reported a mean score of 86.1 in 51 revision ACLR cases using BPTB and STSG autografts, and Jiang et al. reported a score of 87.7 in 34 revision ACLR cases using the same [16, 17]. Based on a meta-analysis of 31 studies of revision ACLR with autografts, Andrilo et al. [18] reported a mean score of 87.5.
Graft choice is controversial, not only in primary ACLR but also in in revision ACLR because of the limited options available due to the previously used graft [19]. The best autograft for revision ACLR remains very much a topic of debate. To the best of our knowledge, no previous studies have analyzed this issue in a population with kneeling customs. Donor site morbidity is an important deciding factor for patients who routinely kneel, as in our study group. The BPTB autograft is known to be associated with anterior knee pain and patellofemoral symptoms affecting kneeling [20]. Patients reported inferior short- and long-term outcomes after revision ACLR with BPTB grafts [21]. A systematic review of the literature based on 2-year follow-ups found a 52% incidence of anterior knee pain and a 65% incidence of kneeling pain with BPTB grafts [22]. Quadriceps are also known to be associated with anterior knee pain and donor site morbidity [22]. Although the literature is limited, donor site morbidly affecting kneeling activities was lower after revision ACLR with QT autografts than revision ACLR with BPTB autografts [22]. A hamstring autograft is preferred in revision ACLR [3, 23]. However, a recent prospective study on 104 patients who received hamstring autografts reported kneeling difficulty in 77% of patients 1 year later and in 54% of patients 2 years later [13]. We found good compliance with each of the autografts used, and these autografts did not restrict prolonged kneeling activities in our study group. In our study, no autograft among the BPTB, STSG, QT was functionally superior among kneeling population, similar to the study in military recruits with a mean follow-up of 40 months comparing BPTB and STSG [23]. As our study population is accustomed to kneeling since an early age, we believe the same may not be true for populations not accustomed to prolonged kneeling.
In previous studies, the study populations comprised of females in majority [24, 25]. In contrast, all the patients in our study were males who underwent single-stage revision, thereby providing a homogenous population for the evaluation of functional outcomes and factors affecting these outcomes. The most common cause of primary failure in our study was trauma (58.33%), with patients presenting with a history of injury, followed by knee effusion. The incidence of trauma as a cause of primary failure in our study was nearly double that found in the MARS cohort, which reported a figure of 32% [25]. In our study, contact sporting activity (i.e., football) was the most common cause of trauma induce failure. As reported previously, activities involving cutting and pivoting pose a very high risk of retears [3]. Although the majority of the patients (70.23%) in our study were satisfied with the functional outcome, these patients reported not returning to sports at preinjury levels, in accordance with the literature [5, 26]. We believe that the latter was due to apprehension about re-trauma and subsequent ACL rupture, which would necessitate another operation.
Previous studies reported technical failure as the most common cause of revision ACLR, constituting up to 77–95% of revision cases [3, 26, 27]. However, in our study group, technical failure accounted for only 22.61% of revision ACLR cases, which we believe is due to the use of radiographic assistance when placing the tunnels in primary ACLR at our institute. In our study, femoral tunnel malpositioning accounted for 94.73% of all technical failures, which is similar to that reported in the literature [26, 28]. Nontraumatic causes accounted for 19.04% of failures, which was similar to that reported by Di et al., who reported a figure of 19.1%, but more than double that found by Wright et al., who reported a figure of 7% [24, 26]. We believe that a lack of graft incorporation and lack of ligamentization are the most likely causes of nontraumatic failure. The high incidence of nontraumatic failure after primary ACLR requires further investigation, as it leads to complaints of persistent instability post-ACLR during the rehabilitation phase within the first year after surgery.
The limitations of our study are that it is a retrospective study, with a subjective functional scoring and no pre-revision scores for comparison.
Conclusions
The functional outcome of revision ACLR in this Middle Eastern Asian Omani population was good-to-excellent, with the patients experiencing no difficulty in performing activities of daily living, including kneeling activities. The outcome of different autografts, BTPB, QT, STSG is similar in high knee flexion patients with no autograft found to be superior. The findings of this study add to the literature on functional outcomes after primary and revision ACLR in a customary kneeling population.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACLR:
-
Anterior cruciate ligament reconstruction
- SPSS:
-
Statistical package for social sciences
- MRI:
-
Magnetic resonance imaging
- STG:
-
Semitendinosus gracilis
- BPTB:
-
Bone-patella tendon-bone
- QT:
-
Quadriceps tendon
- MOON:
-
Multicenter orthopaedic outcome network
- MARS:
-
Multicenter ACL revision study
References
Lyman S, Koulouvaris P, Sherman S (2009) Epidemiology of anterior cruciate ligament reconstruction. J Bone Jt 91:2321–2332. https://doi.org/10.2106/JBJS.H.00539
Lind M, Menhert F, Pedersen AB (2009) The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-008-0654-3
Erickson BJ, Cvetanovich GL, Frank RM, Riff AJ, Jr BRB (2017) Revision ACL Reconstruction. 1–10. https://doi.org/10.2106/JBJS.RVW.16.00094
Hettrich CM, Dunn WR, Reinke EK (2013) Spindler KP (MOON Group): The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med 41:1534–1540. https://doi.org/10.1177/0363546513490277
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39:199–217. https://doi.org/10.1177/0363546510370929
Hamrin Senorski E, Svantesson E, Baldari A, Ayeni OR, Engebretsen L, Franceschi F (2018) Factors that affect patient re- ported outcome after anterior cruciate ligament reconstruction-a systematic review of the Scandinavian knee ligament registers. Br J Sports Med 53:410–417. https://doi.org/10.1136/bjsports-2017-098191
Kvist J, Kartus J, Karlsson J, Forssblad M (2014) Results from the Swedish national anterior cruciate ligament register. Arthroscopy 30:803–810. https://doi.org/10.1016/j.arthro.2014.02.036
Prost JH (1974) Varieties of human posture. Hum Biol 46:1–19. https://doi.org/10.1016/j.arthro.2014.02.036
Hefzy MS, Kelly BP, Cooke TD, Al-Baddah AM, Harrison L (1996) Knee kinematics in-vivo of kneeling in deep flexion examined by bi-planar radiographs. Biomed Sci Inst 33:453–458
Meghani WZ (1996) Why this interest in minority ethnic groups? Br J Occup Ther. https://doi.org/10.1177/030802269605901009
Poehling-Monaghan KL, Salem H, Ross KE, Secrist E, Ciccotti MC, Tjoumakaris F (2017) Long-term outcomes in anterior cruciate ligament reconstruction: a systematic review of patellar tendon versus hamstring autografts. Orthop J Sports Med. https://doi.org/10.1177/2325967117709735
Lund B, Nielsen T, Faunø P (2014) Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy 30:593–598. https://doi.org/10.1016/j.arthro.2014.01.012
Calvert ND, Smith A, Ackland T Kneeling difficulty is common following anterior cruciate ligament reconstruction with hamstring autograft and correlates with outcome measures. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03401-x
Benfayed R, Hamilton D, Moran M, Simpson AHRW, MacDonald D (2017) Interpretation of kneeling. Orthop Muscul Syst 6:240. https://doi.org/10.4172/2161-0533.1000240
Kajaks T, Costigan P (2015) The effect of sustained static kneeling on kinetic and kinematic knee joint gait parameters. Appl Ergon 46:224–230
Boyle C, Pagoti R, Eng K, McMahon S, Nicholas R (2018) Revision ACL reconstruction with autograft: long-term functional outcomes and influencing factors. Eur J Orthop Surg Traumatol 18:29. https://doi.org/10.1007/s00590-018-2277-9
Jiang C, Chen G, Chen P (2018) Double-bundle revision anterior cruciate ligament reconstruction is effective in rescuing failed primary reconstruction and re-introduction patients to physical exercise. Exp Ther Med 15:2074–2080. https://doi.org/10.3892/etm.2017.5647
Andriolo L, Filardo G, Kon E (2015) Revision anterior cruciate ligament reconstruction: clinical outcome and evidence for return to sport. Knee Surg Sports Traumatol Arthrosc 23:2825–2845. https://doi.org/10.1007/s00167-015-3702-9
Wright RW (2014) Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the multicenter ACL revision study (MARS) cohort. Am J Sports Med 11:2301–2310. https://doi.org/10.1177/0363546514549005
Horvath A, Senorski EH, Westin O Outcome After anterior cruciate ligament revision. Curr Rev Musculoskelet Med. 12:397–405 https://doi.org/10.1007/s12178-019-09571-5
Chee MY, Chen Y, Pearce CJ (2017) Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy 33:450–463. https://doi.org/10.1016/j.arthro.2016.09.020
Widner M, Dunleavy M, Lynch S (2019) Outcomes following ACL reconstruction based on graft type: are all grafts equivalent? Curr Rev Musculoskelet Med. https://doi.org/10.1007/s12178-019-09588-w
Balazs GC, Grimm PD, Donohue MA, Keblish DJ, Rue JP (2016) Revision anterior cruciate ligament reconstruction in military personnel. J Knee Surg 29:464–470. https://doi.org/10.1055/s-0035-1564725
Wright RW, Dunn WR, Amendola A (2007) Anterior cruciate ligament revision reconstruction: two-year results from the MOON cohort. J Knee Surg 308:311. https://doi.org/10.1055/s-0030-1248066
MARS Group, Wright RW, Huston LJ (2010) Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med 38:1979–1986. https://doi.org/10.1177/0363546510378645
Di BP, Di BE, Fiocchi A, Beltrame A, Causero A (2016) Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res 1:319–324. https://doi.org/10.5792/ksrr.16.007
Valis P, Sklensky J, Repko M, Rouchal M, Novak J, Otasevic T (2014) Most frequent causes of autologous graft failure in anterior cruciate ligament replacement. Acta Chir Orthop Traumatol Cech 81:371–379
Diamantopoulos AP, Lorbach O, Paessler HH (2008) Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med 36:851–860. https://doi.org/10.1177/0363546507312381
Funding
No funding received.
Author information
Authors and Affiliations
Contributions
SS contributed to conceptualization, data collection, data analysis, drafting manuscript; SAG contributed to conceptualization, drafting manuscript; MAR contributed to conceptualization, review of manuscript; IAH contributed to data collection; SMP contributed to statistical analysis; WAK contributed to data collection; HAS contributed to data collection; SNH contributed to data collection; SRA contributed to data collection, data analysis.
Corresponding author
Ethics declarations
Conflict of interest
No competing interest and funding received by the author and co-authors.
Ethics approval
Ethical approval received.
Data availability
All data are collected from the patient records who underwent surgery at our center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Supreeth, S., Ghanami, S.A., Riyami, M.A. et al. Revision anterior cruciate ligament reconstruction and outcomes with different autografts in a population with kneeling customs. Musculoskelet Surg 107, 171–177 (2023). https://doi.org/10.1007/s12306-022-00739-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-022-00739-w