Abstract
Purpose
The purpose of this study was to compare two types of posterior-stabilized (PS) mobile-bearing (MB) total knee arthroplasties (TKAs). The hypothesis was that no major differences were going to be found among the two TKA designs.
Methods
Two cohorts of patients who were divided according to implant design (Cohort A, new design gradually reducing radius PS MB TKA; Cohort B, traditional dual-radius PS MB TKA) were analyzed by means of intraoperative navigation. All operations were guided by a non-image-based navigation system that recorded relative femoral and tibial positions in native and implanted knees during the following kinematic tests: passive range of motion (PROM), varus–valgus stress test at 0° and 30° (VV0, VV30) and anterior/posterior drawer test at 90° of flexion (AP90).
Results
There were no significative differences in kinematic tests between the two implants. Cohort A, however, showed a different post-implant trend for VV0 and VV30 that were lower than the pre-implant ones, as expected, while for Cohort B, the trend is opposite. However, the gradually reducing radius prosthesis (Cohort A) showed a trend of improving stability (29% compared to the preoperative status) in mid-flexion (VV30) which the traditional dual-radius design (Cohort B) would not. Moreover, we found no differences among postoperative results of the two TKA designs.
Conclusion
Despite design variations, no difference has been found among the prostheses in terms of PROM, rotations and translations. Both design kinematics did not show paradoxical external rotations, but an increase in femoral translation in mid-flexion without affecting the functioning of the prosthesis.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is nowadays a widespread procedure. In 2010, 4.7 million individuals in the USA were living with TKA [19] and this number is expected to increase greatly in the next few years [19, 22, 25]. The aim of TKA is to restore the physiologic knee kinematics, resulting in recovering or improving knee functionality [11]. Various designs are available, including cruciate retaining (CR), postero-stabilized (PS), antero-stabilized (AS) and fixed- (FB) or mobile-bearing (MB) prosthesis.
This prospective cohort study aims to evaluate two different PS implants. This design has been adopted due to a more physiologic femoral rollback during flexion than CR implants [1], a better improvement of range of motion (ROM), prevention of posterior subluxation, increasing quadriceps muscle efficiency and an easier-to-perform soft tissue balancing. Disadvantages include recurrent patellar clunk syndrome and cam–post impingement [3, 12]. However, in recent studies Ünkar et al. [28] as well as Baier et al. [1] found that any significative difference was revealed using a PS or a CR implant. Other designs, such as AS implants, preserve the bone and decrease the wear rate, but they are unable to restore normal knee kinematics, showing significant decrease in condylar rollback [3].
Regarding the bearing, a FB implant resulted in higher clinical success rate, but implant loosening and polyethylene wear cause long-term late failure. MB model creates instead a durable articular surface, providing less tibiofemoral contact stresses [17]. Anyhow, there is no literature evidence in terms of survival and performance to prefer one type over the other [27], neither considering patient satisfaction, nor clinical, functional and radiological outcomes [5].
Navigation systems are a recent intraoperatory support for orthopedic surgeons in TKA [8, 29], allowing both to perform a more precise surgery and to acquire useful data in order to restore normal knee biomechanics. Such systems also allow to objectively examine and compare different types of implants, e.g., PS versus AS prosthesis [3] or ultra-congruent versus PS insert [14].
Kinematics, stability and passive ROM were intraoperatively examined in order to evaluate knee behavior before and after the procedure [3, 4, 8, 14]. These data can provide very useful insights and feedbacks to lean toward a specific type of implant considering each patient’s peculiar needs.
Clary et al. [9] proposed the comparative evaluation of standard fixed dual-radius implant versus gradually reduced radius implant by using a computational model (i.e., Kansas knee simulator) and then performing a cadaveric verification. The reducing radius seemed to improve performance in mid-flexion reducing the magnitude of paradoxical anterior translation of 21–68% depending on the conformity of tibial insert. Anyway, in our knowledge, there is no evidence in the literature about the performance of the sudden implant in intraoperative condition.
We decided to test those specific prostheses because the PFC SIGMA™ knee system has been the prosthesis of choice in our division at Rizzoli Orthopaedic Institute for many years, and while gradually switching to Attune Gradius™ system, we wanted to perform a kinematic comparison among the two. In this paper, kinematic intraoperative data from the two MB PS prostheses were acquired by using a navigation system and then compared.
The primary hypothesis was that both prostheses will show a pre- versus post-kinematic improvement, while secondary hypothesis was that no major kinematic differences were going to be found among the two prosthesis designs.
Materials and methods
This work was a prospective cohort study. Two cohorts of consecutive patients were selected among subjects with advanced knee OA, who were waiting to receive a cemented posterior-stabilized TKA at Rizzoli Orthopaedic Institute (Bologna, Italy). An a priori power analysis was conducted to evaluate the sample size. The parameter chosen was the AP translation. Based on a previous study in the literature [3] which analyzed the laxity reduction through kinematic assessment with navigation system, the standard deviation was set to 3 mm. The difference between the means was set to 2.5 mm, with a statistically significant p < 0.05. Using a power of 0.9, the total sample size resulted to be 14 per cohort group. A total of 30 patients were enrolled for this study and evaluated with the same navigation system. Cohort A was composed of 15 consecutive patients who received a MB PS TKA with gradually reduced radius (Attune Gradius™, DePuy Orthopaedics, Warsaw, IN, USA). Cohort B were composed by 15 consecutive patients who received a traditional dual-radius MB PS TKA (PFC SIGMA knee system™, DePuy Orthopaedics, Warsaw, IN, USA) (Table 1). All patients signed a written informed consent prior surgery. The inclusion criteria were: patient age under 85 years, navigation system usage during surgery and willing to participate to this study. The exclusion criteria were: secondary knee OA, extra-articular deformities and severe varus or valgus deformity (> 15°), requiring a hinged implant, incomplete cinematic data from navigator. All surgeries were performed by the same surgeon (SZ).
A surgical non-image-based navigation system (BLU-IGS, Orthokey Italia srl, Firenze, Italy) was used to measure intraoperative knee kinematics. The navigation system used does affect neither the normal surgical technique nor the knee kinematics. The nominal accuracy of the system is 0.5°/mm and inter-tester reliability > 0.8 (intraclass correlation coefficient ICC) with average standard deviation < 2°/mm [2, 7, 21]. All operations were performed under spinal anesthesia. A tourniquet was used for all patients. Two bicortical pins were inserted to fix the navigation trackers to the femur and tibia. After subcutaneous dissection, the capsule was opened to register patient anatomy, while preserving the cruciate ligaments, menisci and osteophytes. The measured bone resection technique was followed to obtain equal flexion and extension gaps and to facilitate soft tissue balancing. The medial third of the tibial tubercle was used as the anterior reference for the alignment of the tibial base plate.
All resections were performed using the mechanical instrumentation provided with the implant and verified with the navigation system. Hip–knee–ankle (HKA) angle has been corrected to zero (Table 1). The navigation system allowed to measure: knee flexion in degrees, leg axis in degrees (i.e., varus/valgus), anterior/posterior translation in millimeters and internal/external rotation in degrees. All measurements were obtained intraoperatively both: (1) in the preoperative condition, before section of the cruciate ligaments and (2) in the postoperative condition, subsequently to TKA implantation before capsule closure. The surgeon performed multiple kinematic tests on the patients’ knee:
-
1.
varus/valgus stress test in extension (VV0);
-
2.
varus/valgus stress test at mid-flexion (30° of flexion) (VV30);
-
3.
passive range of motion (PROM);
-
4.
anterior/posterior drawer test at 90° of flexion (AP90).
All the tests were executed manually by the operating surgeon and repeated at least three times for each patient. The average value of the repetitions was computed for each patient and recorded for data analysis.
The study was approved by the ethical committee of the Istituto Ortopedico Rizzoli (Bologna, Italy, protocol number 11551/CE/US/ml, 5 May 2006).
Femoral and tibial anatomical reference systems were calculated, and the relative tibiofemoral movement was decomposed using Grood and Suntay (G&S) algorithm [15]. The femoral coordinate system was established using Whiteside’s line for the AP axis, the mechanical femoral axis (femoral head center to distal inter-condylar notch) for the proximal–distal (PD) axis and the cross product of these two for the medio-lateral (ML) axis, and further cross product of PD and ML axes was done to obtain an orthogonal reference system. The tibial reference system was calculated using the line connecting the tibial spine to the medial third of the tibial tuberosity for the AP axis, the mechanical tibial axis (tibial spine to midpoint of malleoli) for the PD axis and the cross product of these two for the ML axis, and further cross product of PD and AP axes was done to obtain an orthogonal reference system.
The raw data were processed using a smooth curve fitting function that enabled direct comparison of patient data at 5° intervals. The internal–external (IE) rotation, recorded during PROM, was plotted against knee flexion, whereas in the antero-posterior test the tibial translation on AP tibial axis was evaluated.
Statistical analysis
All data from navigation system were acquired and exported and subsequently processed using MATLAB® R2016b (The MathWorks, Inc., Natick, MA, USA) for statistical analysis.
The Kolmogorov–Smirnov test was applied in order to reveal whether the acquired data during surgeries had a parametric or nonparametric distribution. Since each intraoperative kinematic parameter resulted in a nonparametric distribution, Wilcoxon’s rank-sum test was implemented to investigate the statistical significance of the difference for each test between pre-implant and post-implant data. The significance level was set at p value < 0.05.
Wilcoxon’s rank-sum test was also applied to compare post-kinematic data among the two cohorts of patients who received the two different types of implants (i.e., Attune Gradius™ and PFC SIGMA™).
Results
A comparison of intraoperative data acquired with the navigation system was made. As reported in Table 2, statistically significative difference at Wilcoxon’s rank-sum test has been observed between pre- and post-varus/valgus test in extension (VV0) for both cohorts (31%, p = 0.01 for Cohort A, 31%, p = 0.048 for Cohort B) and between pre- and post-antero-posterior drawer test at 90° of flexion (AP90) for both cohorts (29%, p = 0.046 for Cohort A, 26%, p < 0.01 for Cohort B). No significative difference has been found at Wilcoxon’s rank-sum test for varus/valgus test at mid-flexion (VV30).
No significative difference has been found, as reported in Table 3, between varus/valgus test in extension (VV0), varus/valgus test at mid-flexion (VV30) and antero-posterior test at 90° of flexion (AP90) when comparing Cohort A and Cohort B among them pre- and post-surgery.
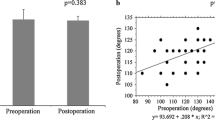
Comparing varus/valgus stress test at mid-flexion (VV30) between Cohort A and Cohort B did not show any significative difference (Fig. 1). Nevertheless, as shown in Fig. 2, for Cohort A (Attune Gradius™ prosthesis) post-implant data for VV30 were lower than the pre-implant ones as expected, while Cohort B (PFC SIGMA™ prosthesis) showed a different trend, with no major difference between pre- and post-implant data for VV30 (Fig. 3).
Tibial rotation during flexion
All patients had similar pre-implant data for internal–external rotation during PROM stress test, which was on average 7.2° ± 3.2° for Cohort A and 7.2° ± 2.7° for Cohort B (p = 1). Similarly, also for post-implant data, any significative difference was revealed, with average data of 6.4° ± 4.5° for Cohort A and 4.4° ± 1.8° for Cohort B (p = 0.25) (Figs. 4 and 5).
The implanted knees did not show paradoxical external rotation.
Differently, a significative difference resulted from the comparison of pre-implant and post-implant intraoperative data for PFC SIGMA prosthesis (p < 0.01), while a value just above the significant threshold was calculated for Attune prosthesis (p = 0.056). Compared to preoperative data, a reduction in tibial rotation was observed post-implant throughout the whole flexion range (i.e., 5°–115°).
Femoral translation during flexion
Pre-implant data for AP translation during AP90 stress test were on average 16.0 ± 7.8 mm for Cohort A and 1 ± 10.7 mm for Cohort B (p = 0.01). Similarly, also for post-implant data, a significative difference was revealed, with average data of 18.3 ± 10.7 mm for Cohort A and 12.2 ± 9.2 mm for Cohort B (p < 0.01) (Figs. 6 and 7). No significative difference in AP translation was revealed comparing pre- and postoperative data for both cohorts (Cohort A, p = 0.06, Cohort B, p = 0.16).
Femoral translation was almost identical than the native knee in early flexion (0–40° for Cohort A, 0–15° for Cohort B). In mid-flexion, both prosthesis designs showed an increase in anterior femoral translation without anyway affecting the functioning of the implant. In deep flexion beyond 100°, both prostheses showed again a similar translation compared to the native knee.
Discussion
The most important finding of the present study was that no significative differences showed among pre- and postoperative kinematic tests of the two different prosthesis designs in varus–valgus stress test at 0° (VV0), 30° (VV30) and in anterior–posterior drawer test at 90° (AP90) (Table 3). No paradoxical external tibial rotation has been noted.
Both prostheses showed a significative increase in stability at 0° (p = 0.01 for Cohort A, p = 0,048 for Cohort B) and in antero-posterior translation of implant (p = 0.46 for Cohort A, p < 0.01 for Cohort B).
We decided to analyze two very similar PS MB prosthesis designs; both validated in improving OA knee biomechanics, as demonstrated by Ranawat et al. [24]. We decided to match the Attune Gradius™ prosthesis with a well-validated implant, such as the PFC SIGMA knee system™, in order to compare two of the most used in our institute. This led us to a much more challenging study, due to very close data and the foreseen difficulty of extrapolating significative data.
PFC Sigma™ is a traditional dual-radius knee prosthesis, showing a J Curve-shaped femoral component. This technology improved old prostheses with fixed radius of curvature, allowing to enhance implant-to-bone contact until 130°–150° of flexion and thereby reducing stress contact points [18]. The sudden transition between the different femoral radii is the main flaw with this implant design and can negatively influence varus–valgus mid-flexion stability.
The Attune Gradius™ femoral sagittal design allows a gradual decreasing of the main curve and therefore a potential improvement in mid-flexion stability. This is achieved by multiple different radii points along the curve, which in turn reduces the sudden transition between the two radii seen in the traditional J Curve designs and is designed to prevent sudden changes in knee stability [13].
When comparing Cohort A and Cohort B, as given in Table 1 and Fig. 2, although values are just above statistical significance, varus–valgus stress test at 30° shows a different trend among the implants. While Cohort B data show similar results compared to pre-surgery stress test, Cohort A shows an improvement in mid-flexion stability with respect of the OA native knee.
This behavior matches the results observed by Hino et al. [16] in their paper, showing an improvement in mid-flexion stability, with a stable increase among ROM values from 20° to 120°. In the authors’ opinion, this behavior can be perceived by the patient in the way they can feel a better stability of their knee during weight-bearing knee flexion, mostly in the 0°–90° range. Those findings are in line with those reported by Carey and Harty [6] and Ranawat et al. [24] in their paper. Carey and Harty compared PFC™ and Attune™ knee systems, showing slight, but significative, improvement in patients’ clinical outcomes. Ranawat et al. did not find significative difference in KSS, but less anterior knee pain in the Attune™ group. Clary et al. in their work [9] discussed how exchanging a dual-radius implant for a gradually reducing radius consistently attenuated the paradoxical anterior slide. This led to evidence that femoral design influence knee kinematics, despite surgical and patient variability.
According to Casino ed al. [7], who evaluated with our same surgical navigator a series of 10 patients treated with PFC™ knee system, our results showed as well how the AP femoral translations trend during flexion was very similar in all cases analyzed. Values of AP pre-operatory translations in our study were significantly different between Cohort A and Cohort B; however, evaluating absolute values of the difference among pre- and post-operatory, those are comparable among them (p = 0.037).
Additionally, in pristine OA knees we noticed an increase in femoral rollback in flexion, in accord with results reported in both in vivo and in vitro studies. Conversely, after TKA we observed in Cohort A, an abnormal femoral anterior translation up to 30° followed by a small femoral rollback comparable with the OA knee. This trend is similar to those observed in previous studies on posterior-stabilized TKA knees and can be clarified by the posterior cam action after 30°–60° [10, 20, 26]. In conclusion, femoral rollback was homogeneous in all subjects analyzed and it was also comparable with other postoperative evaluations.
For what concerns tibial rotations, we noticed that the movement pattern during flexion was modified by the rotating platform, but the amount of rotation during whole motion remained similar before (7.2° ± 3.2° for Cohort A and 7.2° ± 2.7° for Cohort B) and after TKA (6.4° ± 4.5° for Cohort A and 4.4° ± 1.8° for Cohort B). The axial rotation values observed in our intraoperative study are comparable with the amount of rotation found by Ranawat et al. [23] in a postoperative video fluoroscopic study on the same TKA implant that was assessed in our study. They compared a mobile bearing with a fixed-bearing implant and found that the total amount of axial rotation was, respectively, of 7° and 4°.
A limit of our study was the intraoperatory alignment evaluation which has been performed prior to knee capsule suture. This has been led to higher values in translations and rotations with respect of pristine knee. Our data, however, are comparable with that of Bignozzi et al. which evaluated three different PS TKAs with the same surgical navigator we used [3]. We used this paper to compare our data in order to find any procedural error and to double check our results. Both tibial rotations during flexion and anterior–posterior drawer test gave us similar results. It has to be noted that the intraoperative kinematic assessments have to be performed with open joint capsule to allow the surgeon to check the implant before suturing the wound.
Another limit of our study was certainly the small number of cases although surgical navigator data can lead to a statistically significative result with much lesser patients than clinical studies. A bigger group would have surely given benefits in increasing statistical significance. However, we do not believe there are many differences in outcome between the two designs, except from a better stability (as already highlighted by the trend shown in our data) in mid-flexion. We can observe that in fact, as predicted, both prostheses are performing well and give major advantages in restoring normal knee biomechanics. Newer implant shows minor improving, which could, however, have quite a big impact in patients’ knee feedback.
Conclusion
Despite design variations, no difference has been found among the prostheses in terms of PROM, rotations and translations. Both design kinematics did not show paradoxical external rotations, but an increase in femoral translation in mid-flexion without affecting the functioning of the prosthesis.
References
Baier C, Springorum HR, Götz J, Schaumburger J, Lüring C, Grifka J, Beckmann J (2013) Comparing navigation-based in vivo knee kinematics pre- and postoperatively between a cruciate-retaining and a cruciate-substituting implant. Int Orthop 37:407–414
Bignozzi S, Lopomo N, Martelli S, Bruni D, Marcacci M (2008) Accuracy, reliability, and repeatability of navigation systems in clinical practice. Oper Techn Orthop 18:154–157
Bignozzi S, Zaffagnini S, Akkawi I, Marko T, Bruni D, Neri MP, Colle F, Marcacci M (2014) Three different cruciate-sacrificing TKA designs: minor intraoperative kinematic differences and negligible clinical differences. Knee Surg Sports Traumatol Arthrosc 22:3113–3120
Bontempi M, Cardinale U, Bragonzoni L, Macchiarola L, Grassi A, Signorelli C, Marcheggiani Muccioli GM, Zaffagnini S (2017) Total knee replacement: intraoperative and postoperative kinematic assessment. Acta Biomedica 88:32–37
Capella M, Dolfin M, Saccia F (2016) Mobile bearing and fixed bearing total knee arthroplasty. Ann Transl Med 4:127
Carey BW, Harty J (2018) A comparison of clinical- and patient-reported outcomes of the cemented ATTUNE and PFC sigma fixed bearing cruciate sacrificing knee systems in patients who underwent total knee replacement with both prostheses in opposite knees. J Orthop Surg Res 13:54
Casino D, Zaffagnini S, Martelli S, Lopomo N, Bignozzi S, Iacono F, Russo A, Marcacci M (2009) Intraoperative evaluation of total knee replacement: kinematic assessment with a navigation system. Knee Surg Sports Traumatol Arthrosc 17:369
Clarke JV, Deakin AH, Picard F, Riches PE (2017) Lower limb alignment and laxity measures before, during and after total knee arthroplasty: a prospective cohort study. Clin Biomech 47:61–65
Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ (2013) The influence of total knee arthroplasty geometry on mid-flexion stability: an experimental and finite element study. J Biomech 46:1351–1357
Dennis DA, Komistek RD, Colwell CE, Ranawat CS, Scott RD, Thornhill TS, Lapp MA (1998) In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res 356:47–57
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster J-Y (2004) Health-related quality of life in total hip and total knee arthroplasty. J Bone Joint Surg 86:963–974
Fantozzi S, Catani F, Ensini A, Leardini A, Giannini S (2006) Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res 24:2222–2229
Fitzpatrick CK, Clary CW, Rullkoetter PJ (2012) The role of patient, surgical, and implant design variation in total knee replacement performance. J Biomech 45:2092–2102
Fritzsche H, Beyer F, Postler A, Lützner J (2017) Different intraoperative kinematics, stability, and range of motion between cruciate-substituting ultracongruent and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1–6
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136
Hino K, Kutsuna T, Watamori K, Ishimaru Y, Kiyomatsu H, Shiraishi Y, Miura H (2018) Bi-cruciate substituting total knee arthroplasty provides varus–valgus stability throughout the midflexion range. Knee 25:897–902
Huang C-H, Liau J-J, Cheng C-K (2007) Fixed or mobile-bearing total knee arthroplasty. J Orthop Surg Res 2:1
Indelli PF, Marcucci M, Pipino G, Charlton S, Carulli C, Innocenti M (2014) The effects of femoral component design on the patello-femoral joint in a PS total knee arthroplasty. Arch Orthop Trauma Surg 134:59–64
Kremers MH, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ (2015) Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg 97:1386–1397
Li G, Most E, Otterberg E, Sabbag K, Zayontz S, Johnson T, Rubash H (2002) Biomechanics of posterior-substituting total knee arthroplasty: an in vitro study. Clin Orthop Relat Res 404:214–225
Martelli S, Zaffagnini S, Bignozzi S, Bontempi M, Marcacci M (2006) Validation of a new protocol for computer-assisted evaluation of kinematics of double-bundle ACL reconstruction. Clin Biomech 21:279–287
Nemes S, Rolfson O, W-Dahl A, Garellick G, Sundberg M, Kärrholm J, Robertsson O (2015) Historical view and future demand for knee arthroplasty in Sweden. Acta Orthop 86:426–431
Ranawat CS, Komistek RD, Rodriguez JA, Dennis DA, Anderle M (2004) In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res 418:184–190
Ranawat CS, White PB, West S, Ranawat AS (2017) Clinical and radiographic results of attune and PFC sigma knee designs at 2-year follow-up: a prospective matched-pair analysis. J Arthroplas 32:431–436
Singh JA (2011) Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J 5:80–85
Siston RA, Giori NJ, Goodman SB, Delp SL (2006) Intraoperative passive kinematics of osteoarthritic knees before and after total knee arthroplasty. J Orthop Res 24:1607–1614
Tjørnild M, Søballe K, Hansen PM, Holm C, Stilling M (2015) Mobile- vs. fixed-bearing total knee replacement. Acta Orthop 86:208–214
Ünkar EA, Öztürkmen Y, Şükür E, Çarkçi E, Mert M (2017) Posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty for osteoarthritis with severe varus deformity. Acta Orthop Traumatol Turcica 51:95–99
Young KL, Dunbar MJ, Richardson G, Wilson JLA (2015) Intraoperative passive knee kinematics during total knee arthroplasty surgery. J Orthop Res 33:1611–1619
Funding
The authors declare that they did not receive and will not receive any benefits or funding from any commercial party related directly or indirectly to the subjects of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marcheggiani Muccioli, G.M., Fratini, S., Roberti Di Sarsina, T. et al. Two different posterior-stabilized mobile-bearing TKA designs: navigator evaluation of intraoperative kinematic differences. Musculoskelet Surg 105, 173–181 (2021). https://doi.org/10.1007/s12306-020-00643-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-020-00643-1