Abstract
Background
The purpose of this study was to evaluate the accuracy of pedicle screw placement, its advantages, and limitations in posterior instrumentation of thoracolumbar and lumbar burst fractures assisted only by lateral fluoroscopic imaging.
Materials and methods
Pre- and postoperative computerized tomographic (CT) scans of 117 patients with thoracolumbar and lumbar burst fractures, who underwent posterior instrumentation with pedicle screw fixation, were prospectively analyzed. Accuracy of screw placement, reconstruction of the vertebral height, and correction of the kyphotic angle were studied. Position of the pedicle screws were determined, and cortical breach was graded on the postoperative axial CT scans. Percentage of vertebral height reconstruction and kyphotic angle correction were calculated from the postoperative midsagittal CT scans.
Results
Four hundred and sixty-eight pedicle screws in 234 motion segments were included in this study. 427 screws were centrally placed with an accuracy rate of 91.24%. Out of the 41 (8.76%) screws that breached the pedicle wall, 32 (6.84%) screws had violated the medial wall, while 9 (1.92%) screws breached the lateral wall. There were no “air-ball” screws. No screw penetrated the anterior wall. Postoperatively, none of the patients deteriorated neurologically, and no screw required revision. Postoperatively, there was significant restoration of vertebral height and correction of kyphosis (P < 0.05).
Conclusion
Pedicle fixation performed on a Relton-Hall frame is relatively simple and, when performed carefully using only lateral fluoroscopic imaging, has a lower potential for complications due to cortical breach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent times, there has been an increasing tendency toward internal fixation of the spine. The advancements in biomechanics, metallurgy, and safe anesthetic techniques have made internal fixation a method of choice in different disorders such as spinal injuries, deformities, and instabilities [1]. Presently, posterior segmental transpedicular constructs represent the most popular form of spinal instrumentation. Pedicle screws have evolved as the most preferred internal fixation device for the spine. Application of pedicle screws is based on the rationale that the pedicle is the strongest site accessible posteriorly through which a three-dimensional rigid fixation of the vertebra can be obtained [2]. The anatomy and structure of the pedicles provide a relatively rigid and stable construct for stabilization of the spine in a wide range of disorders. It has been proved that the pedicle is the strongest part of the vertebra, even in osteoporotic bone. Pedicle fixation can also be done in the absence of posterior elements.
In thoracolumbar and lumbar fractures, pedicle screws are considered to be the implant of choice, as short segmental stabilization can be achieved while other motion segments are preserved. The methods described for pedicle screw insertion are intersection technique, pars interarticularis technique, and mammillary process technique. The major concern with pedicle screw fixation is related to the safety of these devices. The complications of misplaced screws include pedicle wall breach, leading to spinal cord or nerve root injury and damage to other vital structures [3,4,5]. For accurate screw placement, intraoperative fluoroscopy, image-guided techniques or computerized navigation systems have been devised [6,7,8,9,10]. This study was undertaken to evaluate the accuracy of pedicle screw placement in thoracolumbar and lumbar spine with only lateral C-arm image assistance.
Materials and methods
In a prospective study, 135 consecutive patients with thoracolumbar and lumbar burst fractures who underwent posterior spinal stabilization using Moss-Miami transpedicular screw construct, between August 2009 and August 2014, were analyzed. In 18 patients, the available data were insufficient; thus, 117 remaining cases (a total of 468 pedicle screws at 234 motion segments) were included in the study. There were 72 patients with thoracolumbar fractures (D12 and L1), and 45 patients had fractures of the lumbar spine (L2, L3, and L4). The male-to-female ratio was 11.8:1. The mean age at the time of injury was 31.8 years (range 19–56 years). The most common mechanism of injury was fall from height, and most common level was L1. All patients included in this study were operated and followed up by the senior author. Institutional ethical committee clearance was obtained. All patients were operated within 24 h of presentation. The surgical technique was similar in all patients.
Clinical assessment
Neurological examination was done at presentation and every 6 h subsequently, until recovery from spinal shock. The neurological status was classified according to the American Spinal Injury Association’s modification of Frankel grading [11].
Radiological evaluation
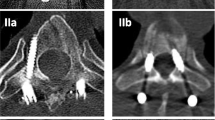
Antero-posterior and lateral radiographs of the spine were obtained to determine the level and type of spinal injury. Computerized tomographic (CT) scans were done in all patients. On the midsagittal CT scan, the segmental kyphotic angle across the fractured vertebra was measured by Cobb’s method [12], and loss of vertebral body height was calculated by the formula described by Mumford et al. [13]. The least midsagittal dimension of the spinal canal was calculated in the axial CT scans as described by Hashimoto et al. [14] (Fig. 1). The same formulae were subsequently used to determine the immediate postoperative kyphotic angle, vertebral height restoration, and canal decompression. Postoperative axial CT scans, at the levels of pedicle screw fixation were evaluated to determine the accuracy of screw placement in the pedicle and breach of the anterior wall. Medial or lateral pedicle wall violations were graded as per the method described by Gertzbein et al. [3] (Fig. 2). The screw path length, screw diameter, and pedicle screw path angle were measured in all cases to analyze the accuracy of the inserted screws. The preoperative CT scans at the levels that had medial or lateral wall breach were re-assessed to determine the cause of pedicle breach. All digitalized CT scans were analyzed using image analysis software Digimizer version 4.6.1 by two independent investigators in a blinded fashion (MPK&GSG).
a Preoperative midsagittal CT scan showing loss of vertebral height and kyphosis. b Postoperative midsagittal CT scan showing restoration of vertebral height and correction of kyphosis. c Preoperative axial CT scan showing narrowing of spinal canal. d Postoperative CT scan showing decompression of canal due to ligamentotaxis
Operative technique
The anesthetized patient was positioned prone on a Relton-Hall frame, to allow postural reduction of the fracture and decompression of abdominal contents (Fig. 3). Pedicle screw insertion assisted only by lateral fluoroscopic image was carried out, in the following steps. The spine was meticulously exposed up to the transverse processes, bilaterally, through a posterior midline approach. Using a bone nibbler, 3–5 mm of the inferior part of the facet joint was exposed, and the base of the superior facet was identified. The pedicle insertion site was localized using the intersection technique. The C-arm was positioned and adjusted so that the right and left pedicles were perfectly superimposed. A pilot hole was made using a sharp-tipped awl to create a posterior cortical breach, 5 mm in depth (Fig. 4). A gearshift probe (2-mm blunt tip pedicle finder) was introduced into the pilot hole and advanced, searching for a cancellous “soft-spot,” indicating passage into the pedicle. The probe was inserted without excessive force into the body up to a depth of 30–35 mm. Antero-posterior images were not used. A blunt K-wire was introduced to palpate 5 distinct bony borders: four walls (medial, lateral, superior, and inferior) and the floor (Fig. 5). If a breach was noted, the probe was redirected to an appropriate position in the pedicle. The pedicle was tapped along the whole tract. Following this, the tract was palpated again to make sure that all five osseous borders were still intact (Fig. 6). The screw was then placed along the pedicle into the vertebral body in the same alignment. Lateral fluoroscopic imaging was used throughout the procedure to ensure accurate placement of the screw. After all the screws were inserted, contoured rods were fixed to the screws, and optimal distraction was done (Figs. 7, 8). Screws were torqued with the rods, and the construct was stabilized with a transverse device. At the end of the procedure, the position of implants was verified on fluoroscopic imaging (Fig. 9). Wound closure was done in layers. In general, 30-mm-long screws, 5 mm in diameter, were used in the lower thoracic pedicles and 35–40-mm-long screws, 6 mm in diameter, for lumbar pedicles [15].
a Exposure of the spine one level above and one level below the fractured vertebra, through a posterior midline approach. Sharp tipped awl placed at entry point of the pedicle screw. b Localization of the pedicle screw entry point using intersection technique. c Lateral fluoroscopic view to ensure sharp tipped awl is in the center of the pedicle
Postoperatively, the patients were immobilized in a polyethylene molded body jacket. Associated injuries and complications were treated accordingly. Antero-posterior, lateral radiographs and CT scan were obtained. They were followed up every 3 months for neurological and radiological assessment for a minimum period of 18 months.
Statistical analysis
Statistical calculations were made using Statistical Package for Social Sciences (SPSS) for Windows version 13. The interobserver and intraobserver variation for all measurements were analyzed using interclass correlation coefficient. No significant difference was noted. Postoperative reconstruction of the vertebral height, correction of the kyphotic angle, and percentage of canal decompression were assessed using paired student’s t test. For all statistical tests, P < 0.05 was considered to be significant.
Results
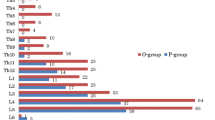
Out of 468 screws that were implanted from D11 to L5, 427 screws were centrally placed in the pedicle with no medial or lateral pedicle wall violation, with an overall accuracy rate of 91.24%. Forty-one screws (8.76%) violated the pedicle wall (either medially or laterally) of which nine screws (1.92%) penetrated the lateral pedicle cortex, whereas 32 screws (6.84%) penetrated the medial pedicle cortex (Table 1). None of the screws penetrated the anterior vertebral body cortex, and there were no “air-ball” screws. When the transverse pedicle width and screw path length at different levels (measured by preoperative CT scans) and the dimensions of the pedicle screw inserted (measured by postoperative CT scans) were compared, it was found that the screw diameter and screw length were always significantly less than the pedicle dimensions.
In the 41 cases of pedicle wall violation, comparison between transverse pedicle angle (measured on preoperative CT scans) and pedicle screw path angle (measured by postoperative CT scans) revealed a statistically significant difference between the angle of screw insertion and transverse pedicle angle of the vertebra. When the pedicle screw violated the medial wall, the mean ± SD transverse screw angle was 16° ± 4.1°, whereas the mean ± SD transverse pedicle angle measured preoperatively at the same levels was 8.6° ± 2.6°. When the pedicle screw violated the lateral wall, the mean ± SD transverse screw angle was 6.7° ± 1.6°, whereas the mean ± SD transverse pedicle angle measured at the same levels was 7.7° ± 1.9° (Table 2). None of the breaches were due to morphological abnormalities of the pedicle. This explains that the screws breached the pedicle wall due to an error in the angle of insertion. There was a statistically significant difference between the preoperative and postoperative kyphotic angle, loss of vertebral height, and canal compromise (Table 3).
Discussion
The technique for pedicle screw insertion described in this study is relatively simple and provides the following advantages. The patient is positioned prone on a Relton-Hall frame; thereby the decompression of abdominal contents prevents inadvertent injury to anterior vital structures and decreases blood loss. It also produces postural reduction and allows easy identification of facet joints and the entry point for pedicle screws. The lateral view on fluoroscopy ensures accurate placement of the screws. The relative stability of the construct allows restoration of vertebral height by distraction and the contoured rods correct kyphosis. Even though restoration of vertebral height and kyphotic angle is controversial, we are of the opinion that restoration of normal anatomy is paramount. Optimal restoration of vertebral height is crucial, as indirect decompression of the spinal canal is achieved by ligamentotaxis [16,17,18,19,20].
For accurate pedicle screw placement by conventional technique, both antero-posterior and lateral fluoroscopic images are commonly used. Recently, computerized navigation has been advocated to increase the accuracy of pedicle screw placement. In the current study, the accuracy of pedicle screw insertion with only lateral fluoroscopic image assistance was found to be comparable to the results of Odgers et al. [21] and other methods (Table 4). The poor results in some of the earlier studies on conventional method of pedicle screw insertion were mainly due to non-adherence to the morphological characteristics of the pedicles [9]. When analyzed, it was seen that an erroneous angle of screw insertion was the major cause of wall violations [9, 22]. Assuming a constant starting point is chosen and the screw is inserted at an angle corresponding to the transverse pedicle angle as determined from the preoperative CT scan, the pedicle wall violation can be avoided [23]. The pedicle diameter, screw path length, and transverse pedicle angle are different at different spinal levels [5]. Majority of the breaches in this study were less than 4 mm. None of the cases required revision, and no patient had postoperative neurological deterioration. The high rate of accuracy in our study can be attributed to the following reasons: selection of the correct entry point, placement of the probe and tap along the center of the pedicle seen in the lateral fluoroscopic view, and directing the pedicle screws along the exact pedicle angle up to the appropriate depth.
The advantages of using only lateral fluoroscopic images are: The fixation can be performed using a conventional operation theater table, whereas, for antero-posterior fluoroscopic image, a special radiolucent operating table is required. Secondly, the patient is positioned on a Relton-Hall spinal extension frame which allows postural reduction of the fracture. Thirdly, lateral image assistance helps in assessing the correction of kyphotic angle and restoration of vertebral height. Lower radiation exposure to both the surgeon and the patient is achieved without compromising on accuracy. The drawback of this study is the lack of a control group, in whom both antero-posterior and lateral fluoroscopic image assistance is used for insertion of pedicle screws. However, as our patients were positioned on a Relton-Hall frame, which is radio-opaque and interferes with antero-posterior imaging, no such control group could be studied.
Conclusion
Pedicle fixation done as per the current study is relatively easy and has a lower potential for complications and lesser radiation exposure. The accuracy of pedicle screw placement using technique by intraoperative lateral C-arm images (and no antero-posterior images) in thoracolumbar and lumbar spine was found to be comparable to other methods of pedicle fixation.
References
Steffee AD, Biscup RS, Sitkowskj DJ (1986) Segmental spine plates with pedicle screw fixation a new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop Relat Res 203:45–53
Roy-Camille R, Saillant G, Berteaux D, Salgado V (1976) Osteosynthesis of thoraco-lumbar spine fractures with metal plates screwed through the vertebral pedicles. Reconstr Surg Traumatol 15:2–16
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 15:11–14
Yahiro MA (1994) Comprehensive literature review: pedicle screw fixation devices. Spine 19(20):2274S–2278S
Puvanesarajah V, Liauw JA, Lo SF, Lina IA, Witham TF (2014) Techniques and accuracy of thoracolumbar pedicle screw placement. World J Orthop 5(2):112
Kalfas IH, Kormos DW, Murphy MA et al (1995) Application of frameless stereotaxy to pedicle fixation of the spine. J Neurosurg 83:641–647
Amiot LP, Lang K, Zippel H, Labelle H (1998) Comparative accuracy between conventional and computer-assisted pedicle screw installation. Presented at the annual meeting of the international society for the study of the lumbar spine, Brussels, Belgium
Merloz P, Tonetti J, Pittet L et al (1998) Pedicle screw placement using image guided techniques. Clin Orthop 354:39–48
Schwarzenbach O, Berleman U, Jost B et al (1997) Accuracy of computer-assisted pedicle screw placement. An in vivo computed tomography analysis. Spine 22:452–458
Laine T, Schlenzka D, Mäkitalo K et al (1997) Improved accuracy of pedicle screw insertion with computer-assisted surgery. Spine 22:1254–1258
Maynard FM et al (1997) International standards for neurological and functional classification of spinal cord injury. Spinal Cord 35:266–274
Cobb JR (1948) Outline for the study of scoliosis. In: Edwards JW (ed) Instructional course lectures, vol 5. The American Academy of Orthopedic Surgeons, Ann Arbor, pp 261–275
Mumford J, Weinstein JN, Spratt KF, Goel VK (1993) Thoracolumbar burst fractures: the clinical efficacy and outcome of non-operative management. Spine 18:955–970
Hashimoto T, Kaneda K, Abumi K (1988) Relationship between traumatic spinal canal stenosis and neurologic deficits in thoracolumbar burst fractures. Spine 13:1268–1272
Olsewski JM, Simmons EH, Kallen FC, Mendel FC, Severin CM, Berens DL (1990) Morphometry of the lumbar spine: anatomical perspectives related to transpedicular fixation. J Bone Joint Surg 72(4):541–549
Gaines RW (2000) The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am 82-A:1458–1476
Krag MH, Weaver DL, Beynnon BD, Haugh LD (1988) Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine (Phila Pa 1976) 13:27–32
Zou D, Yoo JU, Edwards WT, Donovan DM, Chang KW, Bayley JC, Fredrickson BE, Yuan HA (1993) Mechanics of anatomic reduction of thoracolumbar burst fractures| comparison of distraction versus distraction plus lordosis, in the anatomic reduction of the thoracolumbar burst fracture. Spine 18(2):195–203
Harrington RM, Budorick T, Hoyt J, Anderson PA, Tencer AF (1993) Biomechanics of indirect reduction of bone retropulsed into the spinal canal in vertebral fracture. Spine 18(6):692–699
Mohanty SP, Bhat SN, Ishwara-Keerthi C (2011) The effect of posterior instrumentation of the spine on canal dimensions and neurological recovery in thoracolumbar and lumbar burst fractures. Musculoskelet Surg 95(2):101–106
Odgers CJ, Vaccaro AR, Pollack ME, Cotler JM (1996) Accuracy of pedicle screw placement with the assistance of lateral plain radiography. J Spinal Disord 9(4):334–338
Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S (1996) Accuracy of pedicle screw placement in lumbar vertebrae. Spine 21:1320–1324
Weinstein JN, Spratt KF, Spengler D, Brick C (1998) Spinal pedicle fixation: reality and validity of roentgenogram – based assessment and surgical factors on successful screw placement. Spine 13:1012–1016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Institutional ethical clearance was obtained before starting the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Mohanty, S.P., Bhat, S.N., Pai Kanhangad, M. et al. Pedicle screw fixation in thoracolumbar and lumbar spine assisted by lateral fluoroscopic imaging: a study to evaluate the accuracy of screw placement. Musculoskelet Surg 102, 47–55 (2018). https://doi.org/10.1007/s12306-017-0498-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-017-0498-4