Abstract
Purpose
Reverse shoulder arthroplasty becomes more widely used as treatment for patients with complex cuff arthropathy. Theoretically, a higher retroversion of the humeral component leads to an increase in external rotation ROM and a decrease in internal rotation ROM. There is no consensus in optimal retroversion orientation. We retrospectively describe the effect of retroversion of the humeral component. We hypothesize that 20° humeral retroversion improves postoperative ROM, strength or clinical outcome scores compared to neutral retroversion.
Methods
A retrospective clinical study is performed. An Aequalis reverse shoulder prosthesis was placed in 65 shoulders from 58 patients with a mean age of 73.8 years (95% CI 72.0–75.6). Between October 2006 and May 2012, the humeral component was placed in neutral retroversion in 36 shoulders (55%). From June 2012 to June 2014, it was placed in 20° retroversion in 29 shoulders (45%). After a mean follow-up of 36 months with a minimum of 12 months, patients were invited for a study visit. ROM, strength, Constant-Murley and Oxford Scores were measured.
Results
ROM, strength and Constant-Murley and Oxford Scores did not differ significantly between both groups.
Conclusions
With the Aequalis prosthesis, no significant effect of 0° or 20° retroversion on external and internal rotation ROM, strength or functional outcome scores was found.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reverse shoulder arthroplasty is a rapidly increasing treatment for complex cuff arthropathy [1]. However, restoring full range of motion (ROM) remains a problem, especially external and internal rotation [2]. Paul Grammont, the inventor of the Delta reverse shoulder prosthesis, already suggested increasing humeral component retroversion as a theoretical option to improve external rotation [3]. However, this will have a potentially negative effect on internal rotation. Currently there is no agreement on an optimal retroversion angle. Several authors described a wide range of optimal humeral component retroversion regarding stability, scapular notching and ROM, ranging from 0° to 40° [4–8]. However, those studies were performed on cadavers or computer models. To our best knowledge, only one clinical study assessed the influence of retroversion on ROM in vivo, describing no significant differences in ROM between 0° and 20° retroversion, but a significantly better score in the 0° group for activities in daily living (ADL) task back washing/doing up bra [9]. However, only a Korean population was studied, which on average has a different morphology than the European population as treated in our hospital [10]. This difference might affect changes in component positioning.
In this present study, we retrospectively describe the clinical effects of a different humeral component retroversion angle of 0° and 20° on ROM, strength and functional outcome scores. Retroversion between 0° and 20° was described in the surgical technique manual from the manufacturer of the prosthesis. From a theoretical point of view, a higher retroversion increases external rotation, but may decrease internal rotation ROM. Our hypothesis was that compared to neutral retroversion, 20° humeral component retroversion in vivo increases postoperative ROM, strength and functional outcome scores.
Materials and methods
Participants
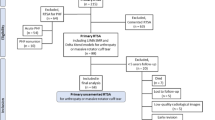
The study protocol was approved by the local ethics committee of the hospital (METC ZWH 14-009). A retrospective study was performed to evaluate the influence of humeral component retroversion on shoulder range of motion and functional outcome scores. All operations were performed by the senior author (PH) between October 2006 and June 2014. Operation indication was cuff arthropathy in all patients. Reasons for exclusion were death, lack of notation of retroversion in the operation report, treatment with fracture prosthesis or revision from previous shoulder prosthesis. A total of 127 patients were invited to participate in this study. Sixty-five shoulders from 58 patients with a mean age of 73.8 years at the time of surgery accepted participation. Minimum follow-up time was twelve months. From October 2006 to May 2012, 36 prostheses were placed with the humeral component in 0° retroversion. From June 2012 to June 2014, another 29 prostheses were placed in 20° retroversion.
Surgical technique
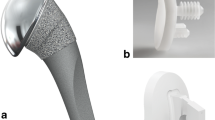
The deltopectoral approach was used to implant an Aequalis Reversed Shoulder prosthesis (Tornier, Montbonnot, France). Intraoperatively, the retroversion relative to the forearm was determined using the alignment guide supplied with the Aequalis prosthesis (Fig. 1). The glenoid component was placed in neutral position in all patients. Five prostheses were cemented (all in neutral group). Autologic bone grafting for the glenoid component (BIO-RSA) was used in six shoulders (two in neutral group, four in 20° group). The subscapularis tendon was repaired in 25 shoulders. The capsule was detached and repaired together with the subscapularis as one layer. Posterior capsule was released for optimal exposure of the glenoid. Biceps tenotomy was performed when present. No tendon transfers were done. Patients were instructed to wear a sling for 3 weeks postoperative. No active or passive external rotation more than the neutral position or active internal rotation was allowed in this period. Patients were allowed to move their arm within the pain limit and the current ROM.
Procedure
The patients were asked for a study visit at the outpatient clinic. At this follow-up examination, the ROM was measured by the same independent researcher for all patients, using a goniometer, which included active abduction, glenohumeral abduction (GHA), forward flexion, external rotation in 0°–90° abduction. Internal rotation was measured and scored as a component of the Constant-Murley Score [11]. An electronic spring balance device was used to measure abduction strength, measured with the patient standing, with the arm in 90° of abduction. Abduction strength was not measured when the patient was unable to reach this position. Internal rotation strength was measured in 0° of abduction in the shoulder and 90° of flexion in the elbow. Two clinical outcome scores were completed, the Constant-Murley Score and the Oxford Shoulder Score [12].
Statistical analysis
An independent sample t test was used to compare ROM, strength and outcome scores between the two groups using SPSS 17.0 (IBM Co., Armonk, NY, USA). Results were adjusted for follow-up time using linear regression. A two-tailed p value less than 0.05 was considered to be statistically significant.
Results
Demographics
Demographics did not differ significantly between the two groups, except for follow-up period (Table 1). Mean follow-up time in the 0° group was 51 months with a minimum of 24 and 18 months in the 20° group with a minimum of 12 months. This differs significantly because of the consecutive change from 0° to 20° retroversion from June 2012. Results were adjusted for the difference in follow-up time. As possible complications, five patients reported pain in hand or forearm, when specifically asked for. After acute conditions were ruled out, no further examinations were performed because of the long-time existence and mild complaints, comorbidity, potential preexistence and patients’ demands. One patient reported to have had temporary sensory impairment in the n. ulnaris region after loco-regional anesthesia. At study follow-up, no infections or dislocations were reported.
ROM, strength and clinical outcome scores
Postoperative ROM, strength and clinical outcome scores did not significantly differ between 0° and 20° of humeral component retroversion (Figs. 2, 3 , 4). Abduction strength could not be measured in five patients, because of inability to reach 90° abduction. Internal rotation ROM measured as part of the Constant-Murley Score was similar in both groups (p = 0.82) (Fig. 5). Patients who had bilateral surgery had similar results as patients who had unilateral surgery. Cementation of the prosthesis or BIO-RSA did not influenced functional outcome.
Discussion
Our present study did not find any statistically significant differences in ROM, strength or functional outcome scores between 0° and 20° retroversion. The found differences in ROM in all directions are only small, between 2° and 6°. It is unlikely that these differences are of any clinical influence. Since a minimal clinically important difference of 10 points for the Constant-Murley Score was reported before [13], the small differences found in our present study in the partly subjective Oxford and Constant-Murley Scores suggest similar patient satisfaction and ability to perform daily activities in both groups.
Several authors have assessed the influence of retroversion on stability, scapular notching and ROM in cadaver or radiologic studies, leading to various outcomes, leaving the optimal retroversion angle in vivo unclear [4–8, 14]. It was suggested that retroversion of many factors has only little effect on stability [15]. A biomechanical study was performed by Favre et al. [14], controversially recommending neutral version or even anteversion to avoid instability. Although increased retroversion theoretically improves external rotation, internal rotation is decreased because of later posterior impingement and earlier anterior impingement. However, with the shoulder abducted more than 60°, no impingement occurs in vitro [5]. A biomechanical cadaver study performed by Berhouet et al. [8] described a native retroversion of 17.25° and a decrease in internal rotation and a significant increase in external rotation with higher retroversion of implanted humeral components, suggesting retroversion between 0° and 20° to give the best balance. Whereas Berhouet et al. found a mean external rotation ROM of 33.8° for the worst experimental setting and over 100° for the best setting, our present study found a mean overall external rotation ROM of 30°. These findings suggest the presence of other limits in vivo that are not simulated in cadaver studies, such as capsular or tissue adhesions, muscle stiffness or differences in scapula movement. The only clinical study available also did not find a significant difference in ROM and Constant-Murley Score between 0° and 20° retroversion [9]. Mean reported Constant Murley Score was somewhat higher than in our present study. This might be explained by the higher age in our population compared to the population studied by Rhee et al. Higher age on average tends to decrease the Constant-Murley Score [16]. Rhee et al. [9] reported a significantly better score for ADL task back washing/doing up bra in the 0° group. Our present study did not specifically research this ADL task. However, no significant difference in internal rotation was found. Previously reported instability [7] did not occur in our study group; therefore, this could not be compared between the groups. The same applies to scapular notching, which was reported to be prevented in cadaver shoulders by placing the humeral component in 10° or 20° retroversion [17]. Since our present study did not evaluate scapular notching, we can support nor argue these findings.
Our study had some weaknesses. First, it was a retrospective study. The study had a high loss of follow-up, mainly due to high age of our patients. Common reasons to deny participation were transport or health problems not related to the operated shoulder. Minimum follow-up was short, 1 year; 57% of the patients in our study had follow-up of more than 2 years. However, comparison of middle- and long-term follow-up shows similar results. Further, the operation technique was not fully equal in all patients since five patients received a cemented prosthesis and BIO-RSA was used in six patients. However, this did not influence functional outcome. Further, there were no systematic preoperative data available. Since retroversion might have different effects on clinical outcome with a different prosthesis design, further research on other prosthesis designs might be necessary.
Conclusion
Our present study did not find any significant effects on ROM, strength or functional outcome scores of 0° or 20° retroversion of the humeral component with the Aequalis reverse shoulder prosthesis. Therefore, the humeral component in reverse shoulder arthroplasty can be implanted in any retroversion between 0° and 20°.
References
Oppermann J, Celik E, Bredow J et al (2016) Shoulder arthroplasty in Germany: 2005–2012. Arch Orthop Trauma Surg 136:723–729. doi:10.1007/s00402-016-2417-9
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elb Surg 14(S1):S147–S161. doi:10.1016/j.jse.2004.10.006
Grammont PM, Baulot E (1993) Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 16:65–68
Stephenson DR, Oh JH, Rick Hatch GF, Lee TQ (2011) Effect of humeral component version on impingement in reverse total shoulder arthroplasty. J Shoulder Elb Surg 20:652–658. doi:10.1016/j.jse.2010.08.020
Gulotta LV, Choi D, Marinello P, Knutson Z, Lipman J, Wright T, Cordasco FA, Craig EV, Warren RF (2012) Humeral component retroversion in reverse total shoulder arthroplasty: a biomechanical study. J Shoulder Elb Surg 21:1121–1127. doi:10.1016/j.jse.2011.07.027
Karelse AT, Bhatia DN, De Wilde LF (2008) Prosthetic component relationship of the reverse Delta III total shoulder prosthesis in the transverse plane of the body. J Shoulder Elb Surg 17:602–607. doi:10.1016/j.jse.2008.02.005
Nalbone L, Adelfio R, D’arienzo M et al (2014) Optimal positioning of the humeral component in the reverse shoulder prosthesis. Musculoskelet Surg 98:135–142. doi:10.1007/s12306-013-0274-z
Berhouet J, Garaud P, Favard L (2013) Influence of glenoid component design and humeral component retroversion on internal and external rotation in reverse shoulder arthroplasty: a cadaver study. Orthop Traumatol Surg Res 99:887–894. doi:10.1016/j.otsr.2013.08.008
Rhee YG, Cho NS, Moon SC (2015) Effects of humeral component retroversion on functional outcomes in reverse total shoulder arthroplasty for cuff tear arthropathy. J Shoulder Elb Surg 24:1574–1581. doi:10.1016/j.jse.2015.03.026
Ji JH, Jeong JY, Song HS et al (2013) Early clinical results of reverse total shoulder arthroplasty in the Korean population. J Shoulder Elb Surg 22:1102–1107. doi:10.1016/j.jse.2012.07.019
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164. doi:10.1097/00003086-198701000-00023
Dawson J, Fitzpatrick R, Carr A (1996) Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 78:593–600
Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aärimaa V (2013) Investigating minimal clinically important difference for constant score in patients undergoing rotator cuff surgery. J Shoulder Elb Surg 22:1650–1655. doi:10.1016/j.jse.2013.05.002
Favre P, Sussmann PS, Gerber C (2010) The effect of component positioning on intrinsic stability of the reverse shoulder arthroplasty. J Shoulder Elb Surg 19:550–556. doi:10.1016/j.jse.2009.11.044
Berliner JL, Regalado-Magdos A, Ma CB, Feeley BT (2015) Biomechanics of reverse total shoulder arthroplasty. J Shoulder Elb Surg 24:150–160. doi:10.1016/j.jse.2014.08.003
Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR (2005) Normalization of the constant score. J Shoulder Elb Surg 14:279–285. doi:10.1016/j.jse.2004.10.009
Berhouet J, Garaud P, Favard L (2014) Evaluation of the role of glenosphere design and humeral component retroversion in avoiding scapular notching during reverse shoulder arthroplasty. J Shoulder Elb Surg 23:151–158. doi:10.1016/j.jse.2013.05.009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
de Boer, F.A., van Kampen, P.M. & Huijsmans, P.E. Is there any influence of humeral component retroversion on range of motion and clinical outcome in reverse shoulder arthroplasty? A clinical study. Musculoskelet Surg 101, 85–89 (2017). https://doi.org/10.1007/s12306-016-0443-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-016-0443-y