Abstract
Purpose
Ten percentage of all ankle fractures sustain an associated syndesmotic injury. TightRope is a relatively new technique for syndesmosis fixation, characterized by a non-absorbable FibreWire held tight between two cortical metal buttons. The purpose of this study was to evaluate the results obtained with the use of this device.
Methods
From January 2011 to December 2015, 54 patients with ankle diastases were treated. Eighteen patients were excluded from the study. Fractures of the fibula or tibia requiring fixation were internally fixed using standard AO techniques. Preoperative and the most recent postoperative ankle radiographs were reassessed for measurements of the tibiofibular clear space (TFCS), medial clear space (MCS) and tibiofibular overlap (TFO). Clinical outcomes were assessed at the time of follow-up using the American Orthopaedic Foot and Ankle Society (AOFAS) score, a self-administered Foot and Ankle Disability Index (FADI) score and patients satisfaction.
Results
The mean follow-up was 28, 64 months. Mean values for MCS, TFCS and TFO were 1.51–1.53 and 0.25 cm, respectively. The mean AOFAS score was 93.11, and the mean FADI score was 130.11. Twenty-nine (80.6 %) patients reported their outcome as excellent or very good.
Conclusions
TightRope technique can achieve flexible fixation of the syndesmosis and permit full range of motion of the tibiofibular joint. Patients can start rehabilitation exercise at an early stage after operation. The results of this study indicate that TightRope fixation is a valid option for syndesmotic injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle sprain is the most common trauma in sports. Every day 1 out of 10,000 people undergoes to an ankle injury, and in sports practice incidence becomes 5.23 out of 10,000 [1–3].
In 1–18 % of all ankle sprains occur an injury to the syndesmosis between the distal tibia and fibula, particularly after external rotation or dorsiflexion [4]. Symptoms are pain just above the ankle joint and difficulty at toe-off when running.
Approximately 10 % of all ankle fractures and up to 11 % of ankle soft tissue injuries sustain an associated syndesmotic injury [5, 6].
These injuries require stress radiographs with the foot in external rotation [7, 8]. Magnetic resonance imaging, which has been reported to have a sensitivity of 90 %, specificity of 95 % and accuracy of 93 %, is often used [9, 10]. Arthroscopy confirms the diagnosis [6]. Furthermore CT scan may be useful in preoperative planning [11]. Sometimes these injuries may remain undiagnosed, causing long-term disability, longer recovery periods, chronic instability, chronic pain, osteochondral lesions (also of the talus) or arthritic changes may develop [12].
Repair the syndesmotic complex is necessary to avoid further degeneration of the ankle articulation [13].
Several fixation implants have been reported: metal cortical screws, bioabsorbable screws, syndesmotic bolts and TightRope [14–19].
The most common treatment, recommended by the AO organization, is the metal cortical screw fixation. However, complications are not rare, such as screw loosening, screw breakage, stiffness, prolonged period of protected weight bearing, need for second operation and the risk of late diastasis after early removal or breakage of the screw [20–23].
Surgeons face multiple issues when choosing to repair the syndesmosis with screw fixation [5, 24–32]. Debates are: It would be better to place 3 cortices to allow micromotion or 4 cortices for near absolute rigidity; the length of time needed when the syndesmotic screw should be removed; level of screw placement above the tibial plafond; the weightbearing restrictions to avoid syndesmotic screw breakage; and, if breakage does occur, which has been reported to be as high as 10–29 %, should additional surgery and removal be performed [21, 22].
Another surgical method is the syndesmotic bolt that is more flexible than metal cortical screw fixation, permitting some degree of micromovement [33]. However, it cannot permit the normal range of motion of distal tibiofibular joint, especially the rotation of the fibula [33].
Syndesmotic TightRope and even more flexible fixator have been recently introduced [18, 19, 34–37].
Few studies have reported on the clinical outcomes of TightRope, and the major complication reported is soft tissue irritation over the prominent lateral knot [36–39].
The theoretical advantages of a suture-button device over a metallic syndesmotic screw are that it allows physiologic motion at the syndesmosis while maintaining the reduction, less risk of hardware pain and subsequent implant removal, and it permits earlier return to motion as there is no risk of screw breakage and subsequent recurrent syndesmotic diastasis.
The purpose of this study was to evaluate the results obtained with the use of TightRope in syndesmotic injury.
Materials and methods
From January 2011 to December 2015, 54 patients with ankle diastases were treated with Arthrex TightRope.
The inclusion criterion was that patients sustained distal tibiofibular syndesmotic diastasis with or without ankle fractures, follow-up more than 6 months. Syndesmotic diastasis was defined as tibiofibular clear space (TFCS) more than 6.0 mm on the anteroposterior or mortise radiographs, tibiofibular overlap (TFO) less than 6.0 mm on the anteroposterior radiograph or less than 1.0 mm on the mortise radiographs [40] or medial clear space (MCS) more than superior clear space or 5.0 mm on the anteroposterior radiographs [41]. The exclusion criteria included open ankle fractures or multiple traumas in the ipsilateral lower extremities, the associated pilon fracture, diabetes, neuropathic arthropathy, systemic diseases, dementia, pathological fractures and other problems which made patients unable to comply with instructions.
Eighteen patients were excluded from the study for insufficient follow-up.
The age ranged between 16 and 66 years (average age 34.28 ± 13.43) at the time of surgery.
Twenty-eight patients were male, and eight patients were female. Twenty-four of the ankles were the left and twelve the right.
The mean patient’s weight was 74.83 ± 9.93 kg (range 56–90 kg), and the mean BMI was 24.92.
All the 36 fractures were classified according to the AO classification and the Weber classification (Table 1).
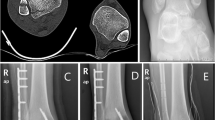
The different traumas were surgical treated by three surgeons (the authors). Fractures of the fibula or tibia requiring fixation were internally fixed using standard AO techniques, and syndesmosis integrity was evaluated using the hook test under fluoroscopy after fixation of the fractures (Fig. 1a–c).
All four cortices were drilled from the open lateral side, 30° anterior to the coronal plane under image guidance, using a 3.5-mm drill bit provided in the prepacked set [42]. The drill hole was performed through one of the empty plate holes, if available. The leading needle was passed through the holes and out from the intact medial skin along with the pull-through sutures, keeping only the white suture under tension and leaving the other slack to keep the oblong button aligned with the holes. Once the leading button passed through the medial tibial cortex, confirmed by imaging, the green and white pull-through sutures were used to toggle the oblong button while giving tension on the FiberWire from the lateral side. Once both the buttons were seated flush with the bone, the free ends of FiberWire on the lateral side were hand tied and cut 0.5 cm long.
All patients were immobilized in a below-knee non-weightbearing cast for 4 weeks followed by physiotherapy and allowed full weight bearing as tolerated. Patients were clinically and radiologically evaluated at 1, 3, 6 and 12 months after surgery.
Clinical outcomes were assessed at the time of follow-up using the American Orthopaedic Foot and Ankle Society (AOFAS) score.
Preoperative and the most recent postoperative ankle radiographs were reassessed by the authors for measurements of MCS, TFCS and TFO. Furthermore, all patients were contacted at the time of this study to collect latest data using a confidential questionnaire and a self-administered Foot and Ankle Disability Index (FADI) score [43, 44] at the time of follow-up.
Measurements were obtained with digital radiographic software (PACS, Syngo Imaging, Siemens Healthcare, Italy).
All measurements were made on an anteroposterior radiograph, 1 cm proximal to the ankle joint [32]. The tibiofibular clear space (TFCS), medial clear space (MCS) and tibiofibular overlap (TFO) measurements were recorded [40]. Non-weightbearing radiographs were excluded.
Patients were asked to indicate the degree of overall satisfaction with postoperative pain management according to the method proposed by Coughlin (0 = unsatisfied/poor, 1 = somewhat satisfactory/adequate, 2 = satisfactory/adequate, 3 = very good, 4 = excellent) [45].
The preoperative data were correlated with the results of the final follow-up using the Student’s t test. A p value <0.05 was considered significant. Statistical analysis was performed using Microsoft Office Excel (2007 version).
Results
The mean follow-up for the 36 patients was 28.64 months (range 6–60 months) after TightRope implantation.
Radiographic measurements were taken on the preoperative, on the postoperative and at follow-up in anteroposterior ankle radiographs 1 cm proximal to the tibial plafond.
Mean values for MCS, TFCS and TFO were 1.51 ± 1.32–1.53 ± 1.34 and 0.25 ± 0.24 cm, respectively, preoperatively, 0.42 ± 0.07–0.46 ± 0.13 and 0.70 ± 0.08 while the follow-up mean MCS was 0.40 ± 0.08 cm, TFCS was 0.46 ± 0.11 cm and TFO was measured as 0.71 ± 0.08 cm (Table 2).
The mean AOFAS score was 93.11 ± 4.38 (range, 86–98) and the mean FADI score was 130.11 ± 2.52 (range, 126–134). Twenty-nine (80.6 %) patients reported their outcome as excellent or very good, while six (16.6 %) reported outcome as good and 1 fair (2.8 %) (Fig. 2).
Only 1 patients required removal of TightRope because of complications related to the lateral knot. It was removed after 6 months because of a prominent knot causing skin irritation. At the removal of TightRope, there was no sign of diastasis on the radiographs.
Discussion
TightRope is a relatively new technique for syndesmosis fixation. It comprises of a non-absorbable FibreWire held tight between two cortical metal buttons. As the TightRope provides semirigid fixation of syndesmosis, it obviates the need for routine removal of the implant, allows early weight bearing and patients can start physical exercises earlier.
Wiker_y et al. [46], in 2010, performed a long-term review of 48 patients who had been followed up for 8.4 years after syndesmotic rupture. They compared the operative and non-operative limb and found those patients who demonstrated more than 1.5 mm widening of the syndesmosis compared with the contralateral limb had inferior clinical results.
In 2005, Thornes et al. [36] performed a clinical and radiological comparison of 16 patients. In the suture-button group demonstrated significantly better AOFAS score and returned to work earlier than the screw group.
Nonetheless, the obvious benefit of leaving the implant intact indefinitely while resuming full activity avoids, not only a second operation, but also resolves the debatable issue of appropriate timing for syndesmotic screw removal [27].
Longer immobilization and protected weight bearing can lead to joint stiffness and decrease in functional capacity [26].
The physiologic motion of the fibula with normal migrational changes throughout the gait cycle and weight bearing has been described [21, 28, 47–49].
TightRope technique can achieve flexible fixation of the syndesmosis and permit full range of motion of the tibiofibular joint. Patients can start rehabilitation exercise at an early stage after operation. In addition, the TightRope does not require removal and there is no concern about hardware breakage [37].
Teramoto et al. [50] showed a significant increase in diastasis during external rotation force acting on the injured syndesmosis of cadaveric specimens fixed with TightRope, when compared with those fixed with a 4.5-mm cortical screw inserting across 4 cortices. Another potential concern is that the medial button might be pulled into the metaphyseal cortex, leading to reduction failure [51].
The device should be placed at the proper level and orientation. Miller et al. [52] reported that the implant inserted 5 cm proximal to the tibiotalar joint could provide improved pull-out strength.
We insert the TightRope at a mean of 1.73 cm (range 1.24–2.52) from the tibiotalar plateau.
Schepers et al. [23] reported a 22.4 % complication rate from routine syndesmotic screw removal. They also reported recurrent diastasis after removal in 5 (6.6 %).
The rate of implant removal might be as high as 10 % [53].
In the literature on syndesmotic screw fixation, this percentage is dependent on hospital protocol and is slightly over 50 % on average. In a recent review, the functional outcome did not differ in cases with retained or removed syndesmotic screws [27].
The routine removal of syndesmotic screws has been associated with a high complication rate of over 20 %, with both recurrent diastasis and wound infection following elective screw removal occurring in up to 10 % [23, 54].
Some cases of TightRope removal are reported in the literature because of soft tissue inflammation and tibialis anterior tendon entrapment from the medial button [34, 36–39, 55].
We report one case of soft tissue irritation on the lateral side requiring removal of implant at 6 months. We identified that the lateral knot remains prominent especially in thin individuals and may lead to soft tissue irritation, inflammation or sinus formation.
New discussions have risen whether one or two suture buttons should be used and in which configuration. Naqvi et al. placed a second TightRope in 26 % and DeGroot et al. [34, 35] used more than one in 75 % of their patients.
A final point of consideration is the additional costs and subsequent cost-effectiveness of the TightRope system versus a syndesmotic screw. The additional costs of a syndesmotic screw removed in daycare surgery in Italy are around 700 Euro, which is approximately the cost of two TightRope systems. There is currently no prospective research on the hospital and socioeconomic cost-effectiveness of the TightRope system versus a syndesmotic screw, which takes the following items into consideration: additional surgery for implant removal, complications, number of follow-up clinic appointments, return to work and additional absence from work.
Conclusions
The results of this study, according to the literature [36, 50, 51], indicate that TightRope fixation is a valid option for syndesmotic injuries. As with any technique, there is a learning curve. The insertion technique is simple and provides syndesmosis stabilization without eliminating normal tibiofibular motion and also obviates the need for a routine second operation for hardware removal, making it potentially cost-effective.
The combination of excellent AOFAS and FADI scores suggesting high patient satisfaction and the objective clinical correlation of radiographic maintenance of the ankle mortise strongly suggest that the TightRope® is a valid option. Not only has the TightRope® addressed several key issues related to fixation, but it has also demonstrated 2-year follow-up data with reliable results for patients who had sustained syndesmotic compromise.
References
Fong DTP, Hong Y, Chan LK, Yung PSH, Chan KM (2007) A systematic review on ankle injury and ankle sprain in sports. Sports Med 37(1):73–94
Magnan B, Samaila E, Bondi M, Vecchini E, Micheloni GM, Bartolozzi P (2012) Three-dimensional matrix-induced autologous chondrocytes implantation for osteochondral lesions of the talus: midterm results. Adv Orthop 2012:942174. doi:10.1155/2012/942174
Nelson AJ, Collins CL, Yard EE, Fields SK, Comstock RD (2007) Ankle injuries among United States high school sports athletes, 2005–2006. J Athl Train 42(3):381–387
Rammelt S, Zwipp H, Grass R (2008) Injuries to the distal tibiofibular syndesmosis: an evidence-based approach to acute and chronic lesions. FCL 13:611–633 (vii–viii)
Stuart K, Panchbhavi V (2011) The fate of syndesmotic screws. Foot Ankle Int 32:S519–S525
Wagener M, Beumer A, Swierstra B (2011) Chronic instability of the anterior tibiofibular syndesmosis of the ankle: arthroscopic findings and results of anatomical reconstruction. BMC Musculoskelet Disord 12:212–225
Dattani R, Patnaik S, Kantak A, Srikanth B, Selvan TP (2008) Injuries to the tibiofibular syndesmosis. J Bone Joint Surg Br 90:405–410
Sman AD, Hiller CE, Refshauge KM (2012) Diagnostic accuracy of clinical tests for diagnosis of ankle syndesmosis injury: a systematic review. Br J Sports Med Jul 47(10):620–628
Han SH, Lee JW, Kim S, Suh J-S, Choi YR (2007) Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int 28:336–342
Magan A, Golano P, Maffulli N, Khanduja V (2014) Evaluation and management of injuries of the tibiofibular syndesmosis. Br Med Bull 111(1):101–115. doi:10.1093/bmb/ldu020
Black EM, Antoci V, Lee JT, Weaver MJ, Johnson AH, Susarla SM, Kwon JY (2013) Role of preoperative computed tomography scans in operative planning for malleolar ankle fractures. Foot Ankle Int 34(5):697–704. doi:10.1177/1071100713475355
Porter DA (2009) Evaluation and treatment of ankle syndesmosis injuries. Instr Course Lect 58:575–581
Mukhopadhyay S, Metcalfe A, Guha A, Mohanty K, Hemmadi S, Lyons K, O’Doherty D (2011) Malreduction of syndesmosisdare we considering the anatomical variation? Inj Int J Care Inj 42:1073–1076
Ahmad J, Raikin SM, Pour AE, Haytmanek C (2009) Bioabsorbable screw fixation of the syndesmosis in unstable ankle injuries. Foot Ankle Int 30:99–105
Beumer A, Campo MM, Niesing R, Day J, Kleinrensink GJ, Swierstra BA (2005) Screw fixation of the syndesmosis: a cadaver model comparing stainless steel and titanium screws and three and four cortical fixation. Injury 36:60–64
Cox S, Mukherjee DP, Ogden AL, Mayuex RH, Sadasivan KK, Albright JA, Pietrzak WS (2005) Distal tibiofibular syndesmosis fixation: a cadaveric, simulated fracture stabilization study comparing bioabsorbable and metallic single screw fixation. J Foot Ankle Surg 44:144–151
Naqvi GA, Cunningham P, Lynch B, Galvin R, Awan N (2012) Fixation of ankle syndesmotic injuries: comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med 40:2828–2835
Rigby RB, Cottom JM (2013) Does the arthrex TightRope provide maintenance of the distal tibiofibular syndesmosis? a 2-year follow-up of 64 TightRopes in 37 patients. J Foot Ankle Surg 52:563–567
Storey P, Gadd RJ, Blundell C, Davies MB (2012) Complications of suture button ankle syndesmosis stabilization with modifications of surgical technique. Foot Ankle Int 33:717–721
Bell DP, Wong MK (2006) Syndesmotic screw fixation in Weber C ankle injuries—should the screw be removed before weight bearing? Injury 37(9):891–898
Manjoo A, Sanders D, Tieszer C (2010) Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma 24:2–6
Melvin J, Downing K, Ogilvie K (2008) A technique for removal of broken cannulated tricortical syndesmotic screws. J Orthop Trauma 22:648–651
Schepers T (2012) Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop (SICOT) 36:1199–1206
Casillas M (2006) Operative treatment of acute syndesmotic injuries with screw fixation and without direct exposure or repair of the syndesmotic ligaments. Tech Foot Ankle Surg 5:27–33
Fanter N, Inouye S, McBryde A (2010) Safety of ankle trans-syndesmotic fixation. Foot Ankle Int 31:433–440
Hoiness P, Stromsoe K (2004) Tricortical versus quadricortical syndesmosis fixation in ankle fractures: a prospective, randomized study comparing two methods of syndesmosis fixation. J Orthop Trauma 18:331–337
Schepers T (2011) To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg 131:879–883
Scranton P (2002) Isolated syndesmotic injuries: diastasis of the ankle in the athlete. Tech Foot Ankle Surg 1:88–93
Teramoto A, Suzuki D, Kamiya T, Chikenji T, Watanabe K, Yamashita T (2011) Comparison of different fixation methods of the suture-button implant for tibiofibular syndesmosis injuries. Am J Sports Med 39:2226–2232
Thordarson D, Samuelson M, Shepherd L, Merkle P, Lee J (2001) Bioabsorbable versus stainless steel screw fixation of the syndesmosis in pronation-lateral rotation ankle fractures: a prospective randomized trial. Foot Ankle Int 22:335–338
Thornes B, McCartan D (2006) Ankle syndesmosis injuries treated with the TightRope suture-button kit. Tech Foot Ankle Surg 5:45–53
Weening B, Bhandari M (2005) Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma 19:102–108
De Vil J, Bonte F, Claes H, Bongaerts W, Verstraete K, Verdonk R (2009) Bolt fixation for syndesmotic injuries. Injury 40:1176–1179
DeGroot H, Al-Omari A, Ghazaly S (2011) Outcomes of suture button repair of the distal tibiofibular syndesmosis. Foot Ankle Int 32:250–256
Naqvi GA, Shafqat A, Awan N (2012) Tightrope fixation of ankle syndesmosis injuries: clinical outcome, complications and technique modification. Injury 43:838–842
Thornes B, Shannon F, Guiney AM, Hession P, Masterson E (2005) Suture-button syndesmosis fixation: accelerated rehabilitation and improved outcomes. Clin Orthop Relat Res 431:207–212
Willmott HJ, Singh B, David LA (2009) Outcome and complications of treatment of ankle diastasis with tightrope fixation. Injury 40:1204–1206
Cottom JM, Hyer CF, Philbin TM, Berlet GC (2008) Treatment of syndesmotic disruptions with the Arthrex Tightrope: a report of 25 cases. Foot Ankle Int 29(8):773–780
Bayer T, McKenna J (2015) Technical tips for the removal of TightRope ankle syndesmosis fixation. Foot Ankle Surg 21(3):214–215
Jordan T, Talarico R, Schuberth J (2011) The radiographic fate of the syndesmosis after trans-syndesmotic screw removal in displaced ankle fractures. J Foot Ankle Surg 50:407–412
Lin CF, Gross ML, Weinhold P (2006) Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther 36:372–384
Arthrex. Surgical Technique. (Online): www.ankletightrope.com
Martin RL, Burdett RG, Irrgang JJ (1999) Development of the foot and ankle disability index (FADI). J Orthop Sports Phys Ther 29:A32–A33
Sheri AH, Hertel J (2005) Reliability and sensitivity of the foot and ankle disability index in subjects with chronic ankle instability. J Athl Train 40(1):35–40
Coughlin MJ (1991) Treatment of bunionette deformity with longitudinal diaphyseal osteotomy with distal soft tissue repair. Foot Ankle 11(4):195–203
Wiker_y A, Hoiness P, Andreassen G, Hellund J, Madsen J (2010) No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma 24:17–23
Forsythe K, Freedman K, Stover M, Patwardhan A (2008) Comparison of a novel FiberWire-button construct versus metallic screw fixation in a syndesmotic injury model. Foot Ankle Int 29:49–54
Klitzman R, Zhao H, Zhang L, Strohmeyer G, Vora A (2010) Suture-button versus screw fixation of the syndesmosis: a biomechanical analysis. Foot Ankle Int 31:69–75
Miller A, Paul O, Boraiah S, Parker R, Helfet D, Lorich D (2010) Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma 24:12–16
Teramoto A, Kura H, Uchiyama E, Suzuki D, Yamashita T (2008) Three-dimensional analysis of ankle instability after tibiofibular syndesmosis injuries: a biomechanical experimental study. Am J Sports Med 36:348–352
Coetzee C, Ebeling P (2009) Treatment of syndesmosis disruptions: a prospective, randomized study comparing conventional screw fixation vs TightRope_ fiber wire fixation-medium term results. SA Ortho J 33:32–37
Miller RS, Weinhold PS, Dahners LE (1999) Comparison of tricortical screw fixation versus a modified suture construct for fixation of ankle syndesmosis injury: a biomechanical study. J Orthop Trauma 13:39–42
Schepers T, Van Lieshout E, de Vries M, Van der Elst M (2011) Complications of syndesmotic screw removal. Foot Ankle Int 32:1040–1044
Hsu YT, Wu CC, Lee WC, Fan KF, Tseng IC, Lee PC (2011) Surgical treatment of syndesmotic diastasis: emphasis on effect of syndesmotic screw on ankle function. Int Orthop 35:359–364
Welck MJ, Ray P (2013) Tibialis anterior tendon entrapment after ankle tightrope insertion for acute syndesmosis injury. Foot Ankle Spec 6(3):242–246. doi:10.1177/1938640013477131
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Rights and permissions
About this article
Cite this article
Bondi, M., Rossi, N., Pizzoli, A. et al. The use of TightRope fixation for ankle syndesmosis injuries: our experience. Musculoskelet Surg 100, 217–222 (2016). https://doi.org/10.1007/s12306-016-0421-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-016-0421-4