Abstract
The association between methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism and susceptibility to Alzheimers disease (AD) was controversial in previous studies. The present meta-analysis was designed to investigate the association of MTHFR C677T polymorphism with AD. Nine studies were identified by search of PubMed, Google Scholar, Elsevier, Springer Link databases, up to January 2013. Odds ratios (ORs) with corresponding 95 % confidence interval (CI) were calculated using fixed effects model or random effects model. All statistical analysis was done by Mix version 1.7. MTHFR C677T polymorphism had a significant association with susceptibility to AD in all genetic models (for T vs C: OR 1.29, 95 % CI 1.15–1.44, p < 0.0001; for TT + CT vs CC: OR 1.38, 95 % CI 1.16–1.364, p = 0.0002; for TT vs CC: OR 1.60, 95 % CI 1.25–2.04, p = 0.0001; for CT vs CC: OR 1.28, 95 % CI 1.1–1.53, p < 0.008; for TT vs CT + CC: OR 1.37, 95 % CI 1.12–1.67, p = 0.002). Results from present meta-analysis supported that the MTHFR C677T polymorphism was associated with an increased risk of AD in Asian population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a neurodegenerative disorder and is the leading cause of dementia in the elderly [1]. It is a genetically complex disorder that causes progressive memory loss in mid-to-late adult life. Some individuals inherit this form of dementia before the age of 65 (referred to as early-onset or familial AD); but most often, AD occurs late in life [2]. AD results from selective degeneration of neurons in neocortex, hippocampus, and basal forebrain cholinergic system. Affected regions show senile plaques, comprised of neurites displayed around extracellular deposits of beta-amyloid peptides; and many neurons develop neurofibrillary tangles were developed in neurons due to accumulation of abnormal intracytoplasmic filaments, composed of hyperphosphorylated tau protein [3]. In the quest for genetic risk factors for late-onset AD only APOE gene has been convincingly identified. Recently clinical and epidemiological studies show a relation between vascular disorders and late-onset AD [4]. Vascular risk factors such as diabetes, hyperlipidemia, high serum homocysteine (Hcy), hypertension and heart diseases are reportedly candidate risk factors for AD. Elevated levels of Hcy have been linked to several vascular diseases [5] and AD [6]. Cell culture experiments have shown that Hcy can cause brain damage through several mechanisms such as impairment of DNA repair, enhancement of beta-amyloid peptide generation and by sensitization of neurons to amyloid toxicity [7, 8].
There are nutritional, hormonal, and genetic determinants of Hcy level. Metabolism of Hcy requires enzymatic action, involving mainly the methylenetetrahydrofolate reductase (MTHFR) and vitamins, namely folic acid, B6, and B12. MTHFR mediates the irreversible conversion of 5,10-methylenetetrahydrofolate (5,10-MTHF) to 5-methyltetrahydrofolate (5-MTHF). Several MTHFR gene polymorphisms have been identified. A common genetic variation in the MTHFR gene, in which cytosine is replaced by thymidine at base position 677 [9] is associated with reduced enzyme activity (60 %) and results in approximately 20 % rise in serum Hcy levels [10]. The T-allele frequency ranges from 0.20 to 0.55 in Europeans, 0.11 to 0.35 in Americans, 0.063 to 0.094 in Africans, and from 0.04 to 0.38 in Asian population [11–13]. MTHFR functions in dimeric form and FAD works as a co-factor for this enzyme, but variant MTHFR (222 V) dissociates into monomers and its enzymatic activity reduces. It is established by docking study that the mutant enzyme (222 V) shows less affinity towards FAD than wild enzyme (222 A) [14]. Some studies showed that the T allele and TT genotype (or the T allele) increases Hcy levels (particular in folate deficiency state) [9, 15, 16], whereas others did not [17]. Its impact on AD development has also been controversial [18, 19]. The results of case control studies on role of MTHFR gene polymorphism in the pathogenesis of AD have been conflicting and inconclusive, hence present meta-analysis was designed to shed some light on the association of MTHFR C677T polymorphism and risk of AD disease in Asian population.
Methods
Identification of Studies
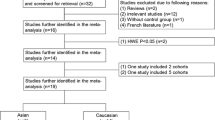
A systematic search was done on published literature using the keywords ‘MTHFR and AD’, ‘folate metabolism and AD’, ‘MTHFR C677T polymorphism and AD’ through ‘Pubmed’, ‘Elsevier’, ‘Springer Link’ and ‘Google Scholar’ up to January, 2014. Detailed information for each study on C677T polymorphism in AD such as the purpose and design of the study, presentation of the data, genotyping method used, inclusion and exclusion criteria of the cases and controls was collected.
Inclusion and Exclusion Criteria
The following inclusion criteria were set for the meta-analysis: (i) each study should be an independent case–control study; (ii) study should have enough information to calculate the odds ratio; (iii) inclusion of the patients was done according to the standard diagnosis parameter [Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), Mini Mental State Examination (MMSE)]. The exclusion criteria included: (i) study not providing enough information (incomplete raw data) and (ii) not well-described.
Data Extraction
Genotype data for MTHFR C677T polymorphism related to AD was extracted. Following information were extracted from each included article- first author name, year of publication, ethnicity of study population, country name, number of cases and controls and allele and genotype frequency was collected.
Statistical Analysis
The present meta-analysis examined the overall association of mutant T allele with the risk of AD relative to the C allele. The strength of association between the MTHFR C677T polymorphisms and AD risk was evaluated by OR and 95 % CI according to allele contrast (T vs C), homozygote (TT vs CC), heterozygote (TC vs CC), recessive (TT vs TC + CC), and dominant (TT + TC vs CC) models. A pooled OR was estimated on the basis of the individual ORs. The OR was estimated by using fixed effects [20] and random effects [21] model depending upon heterogeneity. When there is considerable heterogeneity between studies then the pooled OR is preferably estimated using the RE model [22, 23]. The heterogeneity between studies was tested using the Q-statistic and heterogeneity between studies was quantified using the I2 statistic [24]. If I2 > 50 % then random effect model was used (which gives wider confidence intervals) otherwise fixed effect model applied. Genotype data for control population was analyzed for fitness in the Hardy–Weinberg Equilibrium. For this purpose, control data was analyzed using calculator available at http://ihg.gsf.de/cgi-bin/hw/hwa1.pl.
Publication Bias
Publication bias was investigated by using the funnel plots; viz. funnel plot of standard error by log odds ratio and funnel plot of precision (1/SE) by log odds ratio. Different statistical tests such as Begg and Mazumdar rank correlation [25] and Egger’s regression intercept [26] were adopted to assess the publication bias. All p values are two tailed with a significance level at 0.05. All statistical analyses were undertaken using the freely available program MIX version 1.7 [27].
Result
Study characteristics were summarized in Table 1. Total nine articles that investigated the association between C677T polymorphism and AD were found suitable for the inclusion in the present meta-analysis [18, 19, 28–34]. The studies were published between 1998 and 2013. All these nine studies were performed in different countries—China [19, 29, 32], India [33, 34], Iran [30], Israel [18], Japan [28], and Korea [31].
In all nine studies, total cases were 1146 with CC (385), CT (509) and TT (252), and controls were 1946 with CC (699), CT (879), and TT (368) genotypes. In controls genotypes, percentage of CC, CT and TT were 35.92, 45.17, and 18.91 % respectively. In total cases, genotype percentage of CC, CT, and TT was 33.59, 44.42 and 21.99 % respectively. Frequencies of CC and CT genotypes were highest in both cases and controls (Table 2). In cases and controls, the allele C was the most common. The genotype distributions among the controls of all studies followed Hardy–Weinberg equilibrium.
Meta-analysis
Meta-analysis with allele contrast showed significant association with fixed effect (ORTvsC 1.29; 95 % CI 1.15–1.44; p = <0.0001; I2 = 39.97 %; Pheterogeneity = 0.10) (Fig. 1) and random effect model (ORTvsC 1.34; 95 %CI 1.13–1.58; p = 0.0005) (Table 3).
There was evidence of association of the MTHFR TT genotype with the risk of AD relative to the MTHFR CC genotype with both fixed effect (ORTTvsCC 1.60; 95 % CI 1.25–2.04; p = 0.0001; I2 = 39.65 %; Pheterogeneity = 0.10) (Fig. 2) and random effect (ORTTvsCC 1.74; 95 % CI 1.2–2.5; p = 0.003) models. There was significant association of the MTHFR CT genotype with the risk of AD relative to the CC genotype using fixed and random effect models (ORCTvsCC 1.28; 95 % CI 1.1–1.53; p = 0.008; I2 = 0; Pheterogeneity = 0.49). Dominant model (TT + CT vs CC) also showed significant association with fixed effect (ORTT + CTvsCC 1.38; 95 % CI 1.16–1.64; p = 0.0002; I2 = 5.19 %; Pheterogeneity = 0.39) and random effect (ORTT + CTvsCC 1.39; 95 % CI 1.16–1.66; p = 0.0004) models (Fig. 3). Recessive model also showed significant association with AD with fixed effect (ORTTvsCT + CC 1.37; 95 % CI 1.12–1.67; p = 0.002; I2 = 46.03 %; Pheterogeneity = 0.06) and random effect (ORTTvsCT + CC 1.48; 95 % CI 1.06–2.07; p = 0.02) models.
Publication bias
Begg’s funnel plot and the Egger’s test were conducted to estimate the publication bias of articles. Both the results of Begg’s and Egger’s test did not show any evidence of publication bias (T vs C Begg’s test, p = 0.25, Egger’s test, p = 0.20; CT vs CC Begg’s test, p = 0.25, Egger’s test, p = 0.22; TT vsCC Begg’s test, p = 0.17, Egger’s test, p = 0.16; dominant model TT + CT vs CC, Begg’s test, p = 0.92, Egger’s test, p = 0.26; recessive model TT vs CT + CC, Begg’s test, p = 0.60, Egger’s test, p = 0.23)(Fig. 4).
Discussion
Folate is an essential ingredient of one-carbon metabolism, which is required for the remethylation of Hcy. Several epidemiological and experimental studies have linked folate deficiency and resultant increased Hcy levels with AD. Polymorphism of folate metabolizing gene MTHFR C677T may predispose individuals to elevated plasma levels of Hcy [35, 36]. MTHFR is an essential enzyme in the folate mediated one-carbon transfer reactions and any genetic deficiency in this enzyme could induce severe hyperhomocysteinemia [37]. Elevated Hcy has been reported to be a risk factor for several psychiatric and neurodevelopmental disorders like neural tube defects, depression, bipolar disorder and schizophrenia.
Hcy is implicated in increased oxidative stress, DNA damage, the triggering of apoptosis and excitotoxicity, all important mechanisms in neurodegeneration [37, 38]. It is rapidly taken up by neurons through a specific membrane transporter, leading to high intracellular levels of Hcy [38]. Brain may be particularly vulnerable to high level of Hcy in the blood because it lacks two major metabolic pathways for its elimination: betaine remethylation and transsulfuration [38]. Several mechanisms are proposed by which Hcy causes AD—(i) Hcy can induce calcium influx and oxidative stress, generate free oxygen radicals, accelerate DNA damage and eventually lead to neuron apoptosis [39], (ii) Hcy participates in the amyloid pathway that is involved in the pathophysiology of AD and (iii) Hcy impairs vascular endothelial function, stimulates vascular smooth muscle proliferation [39], breaks balance between coagulation and bleeding pathway and mediates thrombosis. Ultimately, these adverse effects reduce blood supply to the brain and accelerate the neurons apoptosis [39].
Meta-analysis is usually used to combine comparative studies to enlarge the sample size and statistical power and reach more obvious conclusion. Numerous meta-analyses were published considering MTHFR C677T polymorphism as risk for several diseases like—neural tube defects [40], Down syndrome [41], cleft lip with/without palate [42], recurrent pregnancy loss [43], stroke [44], schizophrenia [45], bipolar [46], depression [45], migraine [47] and vascular dementia [48] etc.
Some limitations of present meta-analysis should be acknowledged like—(i) crude OR is used, (ii) study number (only nine studies) and sample size are small, (iii) controls were not uniform in all included studies, (iv) since only the papers published in English language were included in the present meta-analysis, selection bias may have occurred, (iv) other risk factors that have relativity to MTHFR gene or AD, such as hypertension, coronary artery disease and cancer should also be considered and (iv) gene–gene or gene-environment interactions may modify the AD risk and; however, such stratified analysis could not be performed owing to lack of data.
In conclusion, results of present meta-analysis support a strong overall significantly increased risk of AD associated with the C677T polymorphism. However, a very large number of subjects are needed to establish the genetic association between the C677T polymorphism and migraine.
References
Fernandez LL, Scheibe RM. Is MTHFR polymorphism a risk factor for Alzheimer disease like APOE? Arq Neuropsiquiatr. 2005;63:1–6.
Wingo TS, Lah JJ, Levey AI, Cutler DJ. Autosomal recessive causes likely in early-onset Alzheimer disease. Arch Neurol. 2012;69:59–64.
Prince DL, Sisodia SS, Borchett DR. Alzheimer disease: when or why? Nat Genet. 1998;19:314–6.
Luchsinger JA, Tang MX, Shea S, Miller J, Green R, Mayeux R. Plasma homocysteine levels and risk of Alzheimer disease. Neurology. 2004;62:1972–6.
Castro R, Rivera I, Blom HJ, Jakobs C, de Almeida IT. Homocysteine metabolism, hyperhomocysteinaemia and vascular disease: an overview. J Inherit Metab Dis. 2006;29:3–20.
Quadri P, Fragiacomo C, Pezzati R, Zanda E, Forloni G, Tettamanti M, et al. Homocysteine, folate, and vitamin B-12 in mild cognitive impairment, Alzheimer disease, and vascular dementia. Am J Clin Nutr. 2004;80:114–22.
Kruman II, Culmsee C, Chan SL, Kruman Y, Guo Z, Penix L, et al. Homocysteine elicits a DNA damage response in neurons that promotes apoptosis and hypersensitivity to excitotoxicity. J Neurosci. 2000;20(18):6920–6.
Kruman II, Kumaravel TS, Lohani A, Pedersen WA, Cutler RG, Kruman Y, et al. Folic acid deficiency and homocysteine impair DNA repair in hippocampal neurons and sensitize them to amyloid toxicity in experimental models of Alzheimer’s disease. J Neurosci. 2002;22:1752–62.
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995;10:111–3.
Beilby J, Rossi E. Number 58: homocysteine and disease. Pathology. 2000;32:262–73.
Wilcken B, Bamforth F, Li Z, Zhu H, Ritvanen A, Renlund M, et al. Geographical and ethnic variation of the 677C > T allele of 5,10-methylenetetrahydrofolate reductase (MTHFR): findings from over 7000 newborns from 16 areas worldwide. J Med Genet. 2003;40:619–25.
Spiridonova MG, Stepanov VA, Maksimova NR, Puzyrev VP. Population study of frequency of methylenetetrahydrofolate reductase C677T gene polymorphism in Yakutia. Genetika. 2004;40:704–8.
Rai V, Yadav U, Kumar P. Prevalence of methylenetetrahydrofolate reductase C677T polymorphism in eastern Uttar Pradesh. Indian J Hum Genet. 2012;18:43–6.
Yadav U, Kumar P, Rai V. Docking study of MTHFR with FAD by hex. J Comput Intell Bioinform. 2011;4:171–8.
Kluijtmans LA, Young IS, Boreham CA, Murray L, McMaster D, McNulty H, et al. Genetic and nutritional factors contributing to hyperhomocysteinemia in young adults. Blood. 2003;101(7):2483–8.
Devlin AM, Clarke R, Birks J, Evans JG, Halsted CH. Interactions among polymorphisms in folate-metabolizing genes and serum total homocysteine concentrations in a healthy elderly population. Am J Clin Nutr. 2006;83:708–13.
McIlroy SP, Dynan KB, Lawson JT, Patterson CC, Passmore AP. Moderately elevated plasma homocysteine, methylenetetrahydrofolate reductase genotype, and risk for stroke, vascular dementia, and Alzheimer disease in Northern Ireland. Stroke. 2002;33:2351–6.
Chapman J, Wang N, Treves TA, Korczyn AD, Bornstein NM. ACE, MTHFR, factor V Leiden, and APOE polymorphisms in patients with vascular and Alzheimer’s dementia. Stroke. 1998;29:1401–4.
Wang B, Jin F, Kan R, Ji S, Zhang C, Lu Z, et al. Association of MTHFR gene polymorphism C677T with susceptibility to late-onset Alzheimer’s disease. J Mol Neurosci. 2005;27:23–7.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Zintzaras E, Ioannidis JP. Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol. 2004;24:1–15.
Zintzaras E, Koufakis T, Ziakas PD, Rodopoulou P, Giannouli S, Voulgarelis M. A meta-analysis of genotypes and haplotypes of methylenetetrahydrofolate reductase gene polymorphisms in acute lymphoblastic leukemia. Eur J Epidemiol. 2006;21:501–10.
Higgins JP, Thompson SE. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Smith GD, Schneider M, Minde C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Bax L, Yu LM, Ikeda N, Tsuruta H, Moons KG. Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol. 2006;6:50.
Kida T, Kamino K, Yamamoto M, Kanayama D, Tanaka T, Kudo T, et al. C677T polymorphism of methylenetetrahydrofolate reductase gene affects plasma homocysteine level and is a genetic factor of late-onset Alzheimer’s disease. Psychogeriatrics. 2004;4:4–10.
Zhang YD, Ke XY, Shen W, Liu Y. Relationship of homocysteine and gene polymorphisms of its related metabolic enzymes with Alzheimer’s disease. Chin Med Sci J. 2005;20:247–51.
Keikhaee MR, Hashemi SB, Najmabadi H, Noroozian M. C677T methylentetrahydrofolate reductase and angiotensin converting enzyme gene polymorphisms in patients with Alzheimer’s disease in Iranian population. Neurochem Res. 2006;31:1079–83.
Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Shin HY, et al. Methylenetetrahydrofolate reductase gene and risk of Alzheimer’s disease in Koreans. Int J Geriatr Psychiatry. 2008;23:454–9.
Bi XH, Zhao HL, Zhang ZX, Zhang JW. Association of RFC1 A80G and MTHFR C677T polymorphisms with Alzheimer’s disease. Neurobiol Aging. 2009;30:1601–7.
Mansoori N, Tripathi M, Luthra K, Alam R, Lakshmy R, Sharma S, et al. MTHFR (677 and 1298) and IL-6-174 G/C genes in pathogenesis of Alzheimer’s and vascular dementia and their epistatic interaction. Neurobiol Aging. 2012;33:1003.e1–8.
Divyakolu S, Tejaswini Y, Thomas W, Thumoju S, Sreekanth VR, Vasavi M, et al. Evaluation of C677T polymorphism of the methylenetetrahydrofolate reductase (MTHFR) gene in various neurological disorders. Neurol Disord. 2013;2(1):1000142.
Kumar J, Das SK, Sharma P, Karthikeyan G, Ramakrishnan L, Sengupta S. Homocysteine levels are associated with MTHFR A1298C polymorphism in Indian population. J Hum Genet. 2005;50:655–63.
Religa D, Styczynska M, Peplonska B, Gabryelewicz T, Pfeffer A, Chodakowska M, et al. Homocysteine, apolipoproteine E and methylenetetrahydrofolate reductase in Alzheimer’s disease and mild cognitive impairment. Dement Geriatr Cogn Disord. 2003;16:64–70.
Mattson MP, Shea TB. Folate and homocysteien metabolism in neural plasticity and neurodegenerative disorders. Trends Neurosci. 2003;26:137–46.
Sachdev PS. Homocysteine and brain atrophy. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:1152–61.
Zhang MY, Miao L, Li YS, Hu GY. Meta-analysis of the methylenetetrahydrofolate reductase C677T polymorphism and susceptibility to Alzheimer’s disease. Neurosci Res. 2010;68:142–50.
Yadav U, Kumar P, Yadav SK, Mishra OP, Rai V. Polymorphisms in folate metabolism genes as maternal risk factor for neural tube defects: an updated meta-analysis. Metab Brain Dis. 2014. http://www.ncbi.nlm.nih.gov/pubmed/25005003. Accessed on 9 Jul 2014.
Wu X, Wang X, Chan Y, Jia S, Luo Y, Tang W. Folate metabolizing gene polymorphisms MTHFR C677T and A1298c and risk for Down syndrome offspring: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;167(2):154–9.
Zhao M, Ren Y, Shen L, Zhang Y, Zhou B. Association between MTHFR C677T and A1298C polymorphisms and NSCL/P risk in Asians: a meta-analysis. PLoS One. 2014;9:e88242.
Rai V. Methylenetetrahydrofolate reductase gene A1298C polymorphism and susceptibility to recurrent pregnancy loss: a meta-analysis. Cell Mol Biol. 2014;60:27–34.
Yadav S, Hasan N, Marjot T, Khan MS, Prasad K, Bentley P, Sharma P. Detailed analysis of gene polymorphisms associated with ischemic stroke in South Asians. PLoS One. 2013;8(3):e57305.
Gilbody S, Lewis S, Lightfoot T. Methylenetetrahydrofolate reductase MTHFR) genetic polymorphisms and psychiatric disorders: a HuGE review. Am J Epidemiol. 2007;165(1):1–13.
Rai V. Evaluation of methylenetetrahydrofolate reductase gene variant (C677T) as risk factor for bipolar disorder. Cell Mol Biol. 2011;57:OL1558–66.
Schürks M, Rist PM, Kurth T. 5-HTTLPR polymorphism in the serotonin transporter gene and migraine: a systematic review and meta-analysis. Cephalalgia. 2010;30(11):1296–305.
Liu H, Yang M, Li GM, Qiu Y, Zheng J, Du X, et al. The MTHFR C677T polymorphism contributes to an increased risk for vascular dementia: a meta-analysis. J Neurol Sci. 2010;294:74–80.
Acknowledgments
Authoress is highly grateful to Leon Bax (Chief Scientific Officer at BiostatXL, UMC Utrecht) for his valuable suggestions, which help me in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rai, V. Folate Pathway Gene Methylenetetrahydrofolate Reductase C677T Polymorphism and Alzheimer Disease Risk in Asian Population. Ind J Clin Biochem 31, 245–252 (2016). https://doi.org/10.1007/s12291-015-0512-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12291-015-0512-2