Abstract
Graft-versus-host disease (GVHD) is the major complication post hematopoeitic stem cell transplantation (HSCT) causing significant morbidity and mortality. Colonic biopsies were performed in 25 post HSCT patients presenting the diarrhea for diagnosis of acute graft versus host disease (A-GVHD). The present study was undertaken to evaluate and illustrate histomorphological features of A-GVHD in GI biopsies and to grade them. Histopathological features of gastrointestinal biopsies from 25 allogeneic HSCT patients having clinical suspicion of A-GVHD were evaluated and compared with colonic biopsies from negative controls. A-GVHD was observed in 17 cases, CMV colitis was present in 3 cases and one case had herpes simplex infection diagnosed in conjunction with serological findings. A-GVHD was graded as grade 1 and 2 in 10 cases and grade 3 and 4 in 7 cases. Apoptosis of crypt epithelial cells was the cardinal feature for diagnosis. Grade 1 and grade 2 A-GVHD cases showed crypt apoptosis in all cases as well as pericryptal apoptosis in lamina propria in many cases. Occasional crypt loss was seen in grade 2 GVHD. Inflammatory infiltrate was composed of lymphocytes and plasma cells. Neutrophils were inconspicuous. Grade 3 and grade 4 A-GVHD cases showed contiguous areas of multiple crypt loss and ulceration with inflammatory infiltrate predominantly composed of lymphocytes and plasma cells, but neutrophils were more prominent than in grade 1 and 2 A-GVHD. Apoptosis of crypt epithelial cells was present in all grade 3 &4 cases except one case. CMV cases were diagnosed by CMV inclusions and IHC stain. Several factors including drug-induced side effects and infections can cause difficulty in histologic interpretation of gastrointestinal biopsies for GVHD. Proper histomorphological interpretation of intestinal A-GVHD is critical for clinical management. A-GVHD is treated with immunosuppression which may worsen infective condition, if present.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogeneic HSCT is an upcoming curative modality for selected patients with hematologic malignancies, nonmalignant hematologic disorders, immune deficiencies and genetic disorders. GVHD is the major complication after allogeneic HSCT and is attributable to donor T cell recognition of recipient alloantigen. A-GVHD is a significant cause of morbidity and mortality. It frequently involves skin, intestinal tract and liver. GI biopsies are often performed for diagnosis of GVHD. Several factors including drug-induced effects and infections can influence or cause difficulty in histologic interpretation of A-GVHD in GI biopsies. It is essential to recognize A-GVHD features for proper management of these cases.
The present study was done with our aim to evaluate histomorphological features of A-GVHD in GI biopsies and to grade them.
Materials and Methods
This study included 25 post transplant colonic biopsies of allogeneic HSCT patients with clinical symptoms suspicious of GVHD. These were compared with biopsies from negative controls who had colonic biopsies for irritable bowel syndrome (IBS) as these cases do not show significant pathology on colonic biopsies. Fourteen biopsies were taken from colon at the site of maximum involvement on endoscopy. Rest eleven were taken from recto-sigmoid area. In addition duodenal biopsies were also available in six cases. Clinical data of patients were noted which included age, indication for HSCT, post-transplant day of biopsy and CMV titres.
Card board mounted biopsies were received fixed in 10% neutral buffer formalin and processed in tissue processer. Properly orientated paraffin embedded 3 micron sections were cut. Minimum of eight step sections stained by haematoxylin and eosin were evaluated. Special stain for fungus was done in in 2 cases who had oral candidiasis. Grocott’s methenamine silver stain (GMS) was used for fungus. Both cases were negative for fungus. l Immunohistochemical (IHC) studies for CMV were done if the histological picture showed structures suspicious of CMV inclusions. Actively regenerating crypt epithelial cells can mimic CMV inclusions. The antibody used was Mouse anti cytomeaglovirus clone DDG9 and CCH2 ready to use antibody provided by Diagnostic Bio Systems along with Dako detection kit (Envision™ FLEX mini kit IPHC link). Positive control blocks are available for fungus and CMV. Sections are cut from the blocks and simultaneously stained along with the biopsies included in the study.
Histological features of biopsies were critically analysed for A-GVHD. Cases were assessed by three pathologists i.e. senior resident, consultant and senior consultant. All pathologists reached complete concordance. The diagnostic criteria for the GVHD was the minimum criteria discussed in NIH consensus project [1]. Cases with unequivocal diagnosis of A-GVHD were graded using following grading system [2]. This system is modification of grading system described by Lerner et al. [3] and Sale et al. [4].
- Grade 1:
-
Isolated apoptotic epithelial cells, without crypt loss. At least one crypt with apoptosis in one fragment
- Grade 2:
-
Individual crypt loss with apoptotic crypt abscess
- Grade 3:
-
Contiguous area of multiple crypt loss
- Grade 4:
-
Extensive crypt dropout with denudation of epithelium
Results
Histopathological study was done on 25 colonic biopsies of post HSCT patients received over a period of 2 years. Biopsies were performed from 06 to 62 (mean days: 29.2, median post-transplant day 17) days following stem cell transplant. Ages ranged from 06 to 64 (mean age: 26.2, median age 23 years) years. Out of 25 patients 14 were males (64%) and rest were females. The underlying diseases were thalassemia major (7 cases), acute myeloid leukemia (6 cases), myelodysplastic syndrome (3 cases), acute lymphoblastic leukemia (3 cases), primary amyloidosis (2 cases), primary myelofibrosis (1 case), Fanconi’s anemia (1case), non-Hodgkin lymphoma (1 case) and chronic myelomonocytic leukemia (1 case).
Out of 25 colonic biopsies, 17 biopsies (68%) showed evidence for A-GVHD. Three cases had features of cytomegalovirus (CMV) infection and one case of herpes simplex virus infection was diagnosed on serology. As per criteria for grading of A-GVHD in GI biopsies, five patients had pathological changes equivalent to Grade 1 (GVHD), five had Grade 2 (GVHD), six had Grade 3 (GVHD) and one had Grade 4 (GVHD) Table 1.
The relationship of A-GVHD grade with stool volume and skin and liver involvement is shown in Table 2.
A-GVHD grade had no relationship with status of engraftment.
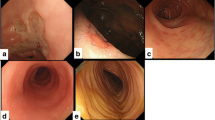
The frequency of various histological features in colonic biopsies are shown in Table 3. Most of the A-GVHD cases showed crypt epithelial cell apoptosis in 16/17 cases as well as pericryptal apoptosis in lamina propria in 11/17 cases (Fig. 1a, b). Apoptotic crypt abscess as were found in 8/17 cases, combined apoptotic and neutrophilic crypt abscess in 4 cases (Fig. 1b). Crypt loss was` found in 12/17 cases (Fig. 1c, d). Inflammatory infiltrate in lamina propria was composed of predominantly lymphocytes and plasma cells in 17/17 cases, however, eosinophils and neutrophils were also seen. One case showed focal fibrosis in lamina propria. A-GVHD cases did not show significant crypt dilatation and regenerative activity except in grade 3 and grade 4 cases.
a Crypts show many apoptotic bodies (grade 1 to 2-GVHD) (H&E, × 400), b crypt abscess- apoptotic and pericryptal apoptosis (grade 2-GVHD) (H&E, × 400), c contiguous area of multiple crypt loss (grade 3-GVHD) (H&E, × 200), d extensive crypt dropout with denudation of epithelium (grade 4-GVHD) (H&E, × 100)
The histological features of A-GVHD (Grade 1 to Grade 4), CMV colitis and control biopsies are shown in Table 3.
Grade 1 and grade 2 A-GVHD cases showed crypt apoptosis in all cases as well as pericryptal apoptosis in lamina propria in many cases. Inflammatory infiltrate was composed of lymphocytes and plasma cells. Neutrophils were inconspicuous.
Grade 3 and grade 4 A-GVHD cases showed crypt loss and ulceration with inflammatory infiltrate predominantly composed of lymphocytes and plasma cells, but neutrophils were more prominent than in grade 1 and 2 A-GVHD.
CMV cases were diagnosed by CMV inclusions and IHC stain (Fig. 2a, b). In our all three cases of CMV there was diffuse ulceration, granulation tissue on surface with crypt loss and predominantly neutrophilic infiltrate. Combined neutrophilic and apoptotic crypt abscess were present in all cases. Histological features of CMV cases are shown in Table 3.
Five control cases were selected who had complaint of GI symptoms and underwent a biopsy for IBS. These patients had history of neither HSCT nor CMV colitis. The control biopsies did not show evidence of apoptosis in crypts.
Both small and large intestinal biopsies were available in six cases to rule out GVHD. However in 5 cases, recto-sigmoid biopsies showed more well-defined histological findings than upper GI biopsies.
All cases were given small doses of steroids along with anti-infective agents after taking the biopsy by clinician. However, steroids were stopped in histologically negative cases and anti-infective agents continued for another three days. Resolution of symptoms was obtained within this time. Stool volume in all these cases was less than 2 L.
Discussion
GVHD is major complication in 30–50% of cases undergoing stem cell transplantation [5]. The classification of A-GVHD as occurring on less than 100 days after HSCT and chronic GVHD after 100 days is not recognized now as use of reduced intensity conditioning regimens has led to later occurrence (after 100 days) of A-GVHD. In fact chronic GVHD in GI is not well recognized. Upper esophageal webs, strictures or concentric rings documented by endoscopy or barium studies are considered diagnostic of chronic GVHD [6]. Clinical criteria should define chronic GVHD and not the time frame [7]. In our study out of twenty-five cases included four were negative for A-GVHD diagnosis, of A-GVHD could be made on 17 biopsies, 3 cases had CMV infection and one case had herpes simplex virus infection. Diagnostic criteria for A-GVHD was the minimum criteria discussed in NIH consensus project i.e. apoptotic body per biopsy piece to total number of apoptotic bodies at least equal to number of biopsy pieces, to scattered apoptotic bodies in more than one crypt [1]. Eight serial sections are recommended to avoid false negative. The proposed recommendations for final diagnosis categories for biopsy reporting from NIH consensus project are : (1) Not GVHD, (2) Possible GVHD (the cases with evidence of GVHD but other possible explanations for findings such as CMV, MMF—associated colitis etc., (3) Consistent with GVHD (clear histologic change of GVHD but with mitigating factors, such as limited sample, minimal findings or recent chemotherapy and radiotherapy, (4) GVHD (unequivocal evidence of GVHD) [1]. However in our study the biopsies were classified as (1) No GVHD and (2) A-GVHD (unequivocal GVHD). Efforts were made to exclude other possible causes such as CMV infection and drug associated changes on clinical, serological and IHC studies. Diagnosis of Grade 1 and 2 A-GVHD was made on presence of apoptotic cells in the crypts and individual crypt loss. Severe GVHD showed in addition contiguous areas of multiple crypt loss along with denudation of mucosal epithelium. Similar findings have been reported earlier [2, 4, 5].
In our study histological Grade 1 GVHD was found in 30% (5/17 cases), Grade 2 also identified in 30% (5/17 cases) of patients and Grade 3 and 4 occurring in 40% (7/17 cases) of patients.
Crypt cell apoptosis is a cardinal feature for diagnosis of A-GVHD [6]. Usually this is focal in nature and results in membrane bound debris of apoptotic bodies in the crypts. Occasional large number of apoptotic bodies are seen in single cell of crypt resulting in intra cytoplasmic vacuoles filled with nuclear dust or karyorrhectic debris called as “exploding crypt cells” [4]. Pericryptal apoptosis is also seen in about 70% of cases [8]. In our study also crypt cell apoptosis was the most helpful feature for diagnosis of A-GVHD along with pericryptal apoptosis. Apoptosis is most prominent in the regenerative compartment of the crypts which has been reported earlier as well [6]. Focal increase in density of lymphocytes, plasma cells, and occasional eosinophils were noted in the lamina propria in our cases, however, the cellular infiltrate in lamina propria was sparse. This feature has also been noted in earlier studies [9].
Apoptosis in the surface epithelial cells can at times be due to physiological turnover or due to bowel preparatory regimens [6]. However, none of our control cases of IBS showed evidence of apoptosis in surface epithelial cells.
A-GVHD is usually considered only after 20 days of transplant as conditioning regiments can cause apoptosis and crypt cell regeneration in early transplant period. Presence of severe injury after this period is likely to represent GVHD [10].
A-GVHD in GI biopsies has to be differentiated from drug induced changes and infections. CMV, adenovirus, MMF colitis can mimic A-GVHD [11,12,13].
In our study in comparison to GVHD, CMV colitis showed extensive ulceration accompanied by neutrophils along with lymphoplasmacytic infiltrate. Crypt loss was extensive and apoptosis was not prominent. Neutrophilic infiltrate was present in CMV colitis, whereas A-GVHD showed predominantly lymphocytes, plasma cells along with eosinophils, however neutrophils were present in severe GVHD as well. Presence of CMV inclusions and IHC confirmed the diagnosis of CMV colitis. Features which can help to distinguish GVHD from CMV colitis are sparse predominant mononuclear infiltrate in lamina propria, presence of apoptotic bodies, apoptotic crypt abscesses, whereas CMV colitis shows relatively more cellular infiltrate in lamina, neutrophilic crypt abscesses and apoptosis is not very prominent. Serology for CMV also helps. However, cases of CMV with co-existent GVHD have management difficulties as treatment of these two disorder is exactly opposite.
MMF colitis can be indistinguishable from A-GVHD. MMF causes mixed acute and chronic inflammation in lamina propria, focal ulcers and increased crypts cell apoptosis [13]. The features which can help to distinguish it from GVHD are focal nature of ulcers, presence of eosinophils and clinical response to MMF therapy cessation. Involvement of other sites such as skin, liver are also suggestive of GVHD and help in excluding drug induced colitis and infective disorders.
Both small and large intestinal biopsy available in six cases to rule out GVHD, however, in 5 cases, biopsy of the recto-sigmoid showed well defined histological findings and was found to be the most informative. Earlier studies also revealed that recto-sigmoid biopsies had the highest sensitivity, specificity for diagnosing GI GVHD [14]. However, in upper GI biopsies duodenal biopsy gives highest yield [15].
Conclusion
So we conclude that apoptosis is a cardinal feature diagnostic of A-GVHD. In comparison to GVHD, CMV colitis in our cases showed extensive ulceration accompanied by combined neutrophilic and apoptotic crypt abscess, whereas A-GVHD showed predominantly lymphocytes, plasma cells along with eosinophils and apoptotic crypt abscesses. Presence of CMV inclusions and IHC confirms the diagnosis of CMV colitis. GVHD cases did not show crypt dilatation, distortion and regenerative activity in crypt epithelium except in severe cases.
Thus proper histomorphological interpretation of A-GVHD in GI biopsies in post allogeneic HSCT is critical for proper management as GVHD needs augmentation of immunosupression which can flare infective disorder if present.
Abbreviations
- HSCT:
-
Hematopoietic stem cell transplantation
- GVHD:
-
Graft versus host disease
- A-GVHD:
-
Acute-graft versus host disease
- GI biopsies:
-
Gastrointestinal biopsies
- CMV:
-
Cytomegalovirus
- IBS:
-
Irritable bowel syndrome
References
Shulman HM, Kleiner D, Lee SJ et al (2006) Histopathologic diagnosis of chronic graft-versus-host disease: National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: II. Pathology working group report. Biol Blood Marrow Transplant 12:31–47
Cogbill GH, Drobyski WR, Komorowski RA et al (2011) Gastrointestinal pathology of autologous graft-versus-host disease following hematopoietic stem cell transplantation: a clinicopathological study of 17 cases. Mod Pathol 24:117–125
Lerner KG, Kao GF, Buckner CD, Clift RA, Thomas ED (1974) Histopathology of graft vs host reaction (GvHR) in human recipient of marrow from HL-A matched sibling donors. Transplant Proc 6:367–371
Sale GE, Shulman HM, McDonald GB, Thomas ED (1979) Gastrointestinal graft-versus- host- disease, in man: a clinicopathologic study of the rectal biopsy. Am J Surg Pathol 3:291–299
Langer F, Puls F, Buchholz S et al (2011) Histopathology of graft vs host disease. Pathologue 32:144–151
Washington K, Jagasia M (2009) Pathology of graft-versus-host disease in the gastrointestinal tract. Hum Pathol 40:909–917
Dignan FL, Clark A, Amrolia P, Cornish J, Jackson G, Mahendra P et al (2012) Diagnosis and management of acute graft-versus-host disease. Br J Haematol 158:30–45
Shidham Vinod B, Chang Chung-Che, Shidham Ganesh et al (2003) Colon biopsies for evaluation of acute graft-versus-host disease (A-GVHD) in allogeneic bone marrow transplant patients. BMC Gastroenterol 3:5
Bombi JA, Nadal A, Carreras E et al (1995) Assessment of histopathologic changes in the colonic biopsy in acute graft-versus-host disease. Am J Clin Pathol 103:690–695
Epstein RJ, McDonald GB, Sale GE, Shulman HM, Thomas ED (1980) The diagnostic accuracy of the rectal biopsy in acute graft-versus-host disease: a prospospective study of thirteen patients. Gastroenterology 78:764–771
Wong NA (2015) Gastrointestinal pathology in transplant patients. Histopathology 66:467–479
Snover DC (1985) Mucosal damage simulating acute graft versus host reaction in cytomegalovirus colitis. Transplantation 39:669–670
Papadimitrious JC, Darchenberg CD, Beskow CO et al (2001) Graft versus host disease like features in mycophenolate mofetil-related colitis. Transpl Proc 33:2237–2238
Ma C, Maluf HM, Liu TC (2015) Acute graft-versus-host disease is more prevalent and severe in the lower than the upper gastrointestinal tract. Hum Pathol 46:1480–1487
Ip S, Marquez V, Schaeffer DF, Donnellan F (2016) Sensitivities of biopsy sites in the endoscopic evaluation of graft-versus-host disease: retrospective review from a tertiary center. Dig Dis Sci 61:2351–2356
Acknowledgements
Authors acknowledge secretarial help provided by Ms. Noora Baweja.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicting interest
All authors declare that they have no conflict of interest.
Ethical Statement
No experipmental procedures were performed in this retrospective and descriptive, laboratory-based-study that reviewed routinely obtained pathological material. Hence. A separate ethics clearance was not taken.
Informed Consent
Informed consent of patients is taken for biopsy.
Rights and permissions
About this article
Cite this article
Azad, S., Malhotra, V., Kirtani, P. et al. Gastrointestinal Biopsies for Evaluation of Acute Graft-Versus-Host Disease in Allogeneic Hematopoietic Stem Cell Transplant Patients. Indian J Hematol Blood Transfus 35, 83–88 (2019). https://doi.org/10.1007/s12288-018-0969-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-018-0969-2