Abstract
Transcranial Doppler (TCD) detects stroke risk in patients with sickle cell anemia (SCA). Hydroxyurea therapy has the ability to induce increased levels of fetal hemoglobin in sickle cells thus decreasing tendency for red cell sickling. This study aimed to evaluate TCD findings in SCA patients on hydroxyurea and correlate the time-averaged mean velocity (TAMV) with their hematological parameters. Forty SCA patients of both sexes, aged 16–22 years with no history of stroke were screened with TCD for an elevated TAMV, divided into: Group T (20 patients on blood transfusion); and Group H (20 patients on daily hydroxyurea). For all, full medical history, clinical examination, hemoglobin, hematocrit, leukocytes, platelets, fetal hemoglobin and sickling test, in addition TCD to describe the pattern of cerebral blood flow abnormalities were done. TAMV in all cerebral arteries were significantly higher in Group T than Group H, the highest TAMV (147.5 ± 57.09 cm/s) was found in the right middle cerebral artery and correlated negatively with hematocrit in Groups H (P < 0.001). There were 2 (10%) abnormal TAMV results and 5 (25%) conditional in Group T, while all results were normal in Group H. Hydroxyurea therapy may lower TCD velocities and prevent the risk of primary stroke in SCA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sickle cell disease (SCD) is an autosomal recessively inherited β-hemoglobinopathy causing an abnormal hemoglobin (HbS) to be expressed in the erythrocyte, the homozygote SS form is known as SCA [1]. In the S-beta globin gene, a normal codon (GAG) is replaced by another (GTG), resulting in exchanging the sixth amino acid of the beta globin. This exchange of glutamic acid for valine causes polymerization of hemoglobin S, when exposed to media with low oxygen tension leads to sickling of red blood cells. This process is responsible for most of the clinical manifestations of SCD [2]. Stroke is one of the clinical complications of SCD [3]. About 5–10% of patients with SCA present stroke by the age of 20 years [4]. Cerebral infarction results from occlusion/stenosis of large arteries supplying the brain. The distal intracranial portions of the internal carotid artery and the proximal middle cerebral artery are particularly prone to stenosis, which can be detected by TCD [5]. TCD is a crucial investigation that can reveal elevated cerebral arterial flow velocities [6]. TCD studies measure flow velocity within the large intracranial arteries, which are the vessels most often involved in sickle cerebral vasculopathy and stroke [7]. It is useful because it is painless, requires no sedation, noninvasive, easy to perform and relatively inexpensive [8]. It is recommended as a routine screening test for patients with SCA, it enables early detection of arterial abnormalities, which is important for primary stroke prevention [9]. Adams et al. [5] conducted several studies using TCD to demonstrate the usefulness of this examination for evaluating stroke risk. Several factors influence the blood flow velocities obtained through TCD, of which hematocrit level, leukocyte and platelet counts [10]. The current standard therapy of monthly blood transfusions to reduce stroke risk can lead to problems such as antibody formation and iron overload, which are recognized as a source of morbidity in SCA patients. Hydroxyurea (HU) is considered as a possible alternative to chronic transfusions for secondary stroke prophylaxis in SCD patients, it acts by several underlying mechanisms [6]. It increases HbF levels, possibly because it is cytotoxic, and this toxicity causes regeneration of erythrocytes, increases hemoglobin, with a decrease in Hb S [11]. HU has been reported to be effective in improving survival and reducing morbidity in some SCD patients. The clinical outcomes include reduction in frequency of painful episodes, acute chest syndrome, transfusions and hospitalization, with no significant toxicities [12]. HU therapy is monitored by a number of laboratory parameters which include increased HbF levels, mean corpuscular volume, and reduction in WBC count. It has been found to be effective in the prevention of brain injury due to cerebrovascular disease [13].
In this study our aim was to evaluate the results of TCD examination in SCA patients on hydroxyurea therapy, and correlate TAMV with the hematological parameters.
Patients and Methods
This was a single-center observational cross-sectional study on 40 patients with SCA, their age ranged 16–22 years, and had no previous clinical diagnosis of stroke or acute crises. Patients refused to undergo TCD examination were excluded. Participants were already on transfusion or hydroxyurea therapy with variable time periods before starting the study and we just observe the difference between the two groups. The patients divided into two groups; Group T (transfusion group) received monthly transfusions to maintain sickle hemoglobin level lower than 30%, Group H (hydroxyurea group) received oral hydroxyurea 20 mg/kg per day. Patients were invited to participate in the study after getting informed consent and the steps and aim of the research were explained to participants. The patients were recruited from clinical hematology unit, Internal Medicine department, Assuit University Hospital and Health Insurance, Assiut, Egypt from January 2016 to October 2016.
Laboratory blood tests including hemoglobin, hematocrit level, leukocyte and platelet counts, hemoglobin S assay by means of hemoglobin electrophoresis and fetal hemoglobin assay.
TCD Screening Protocol
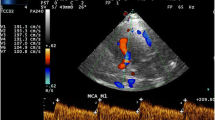
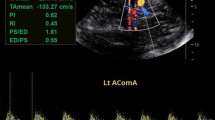
TCD studies were performed in the Department of Radiology Assuit University Hospital. All TCD exams were performed by radiologist. With the patient in the supine position, a 3–5 MHz hand-held convex probe of Logic P6 Pro GE machine was placed in the temporal region of the scalp Using right and left temporal approaches. By manipulating probe angulation, probe position and the depth setting of the instrument, the ultrasound sample volume was placed on major arterial segments of the circle of Willis. The TAMV were measured in the middle cerebral arteries, the internal carotid arteries, the anterior cerebral arteries, and the posterior cerebral arteries in centimeters per second. Multiple measurements were taken at varying depths on either side and for each vessel, between 40 and 60 mm. The highest recorded mean velocity for each artery was assumed to be the most representative and this was recorded as the time-averaged mean velocity (TAMV). All the measurements were recorded. All TCD studies were classified based on the highest TAMV in the ICA or MCA based on STOP criteria as normal (<170 cm/s), conditional (170–199 cm/s), and abnormal (200 cm/s or higher). Studies where readings were unable to be obtained in the ICA and MCA bilaterally were classified as inadequate, unless one side was clearly abnormal.
Statistical Analysis
The data obtained was statistically analyzed using SPSS software data analysis program version 17. Non parametric tests were used due to small sample size: Mann–Whitney test was used to compare means of quantitative variables while Fisher exact test was used to compare percents of qualitative variables, spearman correlation coefficient was also used, P value <0.05 was considered to be statistically significant.
Results
40 patients (22 male and 18 female) with SCA were studied. 20 patients as Group T (transfusion group) and 20 patients as Group H (hydroxyurea group). There were no statistically significant differences as regard age and sex between the two groups, but there were a statistical significant increase of (Hb level, hematocrit, MCVand Hb F) in Group H than Group T (P = 0.001, 0.002, 0.009 and 0.001) respectively, while no significant differences as regard total WBC count and platelet count (Table 1).
TAMV in cm/s were statistically higher in the major intracranial arteries in Group T than Group H. The highest velocities in each patient were recorded in the middle and posterior cerebral arteries (Table 2).
TAMV on TCD studies, among 20 patients on transfusion, 13 (65%) patients had normal velocities TAMV < 170 cm/s, 5 (25%) patients had conditional velocities TAMV > 170 cm/s, while 2 (10%) patient had an abnormal TAMV > 200 cm/s (TAMV of 293.2 and 240.8 cm/s). None of Group H patients showed abnormal TCD velocities (Table 3; Fig. 1).
No evidence of clinical stroke was identified in either treatment group. Vaso-occlusive pain was the most common adverse event in both groups, 3 (15%) patients in Group H and 5 (25%) patients in Group T.
This study showed a significant negative correlation between hematocrit (r = −0.818, P = 0.001) and TAMV in Group H. There was no correlation with total WBC count, hemoglobin level, fetal hemoglobin percentage or total platelet count. None of the hematological parameters were significantly correlated with TAMV in Group T (Table 4).
These results suggest that hydroxyurea treatment could decrease time-averaged mean velocities in SCA patients.
Discussion
Stroke is a significant cause of morbidity and mortality in SCD [14]. It occurs in 10–15% of homozygous patients under the age of 10 years [15]. The risk is higher in patients with low baseline hemoglobin, low fetal hemoglobin, high white blood cell count, Hb SS disease and could be candidates for early and aggressive therapy with disease modifying agents [16]. TCD is a procedure commonly used to screen individuals with the major hemoglobin S diseases. Flow velocities above 200 cm/s have been shown to identify patients at elevated risk for cerebral infarction [17] and is an indication for starting hypertransfusion therapy [18]. Noteworthy, the standard therapy of monthly blood transfusions to reduce stroke risk is not without risks, but added more risks, hence, the need for close monitoring and prompt iron chelation when indicated [19]. The estimated mean annual cost of hypertransfusion in SCD patient is about 3276 US Dollars, also, treatment of iron overload increased the cost [20]. Currently, HU is the only disease-modifying therapy approved for SCD. It is efficacious in children and adults; with an increase in Hb F%, reduction in hospitalizations and pain crises. Hence, there is great interest in understanding more about its use in treating patients with SCA [21]. More controlled multi-center trials on the use of hydroxyurea would be extremely valuable in determining the efficacy of this drug in primary and secondary stroke prevention, particularly in Africa where blood is not readily available, quite expensive, and transfusions are associated with a potential risk of transmission of infections [22]. TWiTCH which is the first Phase III randomized clinical trial compared standard therapy of monthly erythrocyte transfusions with daily HU, for children with elevated TCD velocities and high risk of stroke, they reported that HU has a similar benefit as transfusion [23]. Zimmerman et al. [8] evaluated the effect of HU on TAMV, reported a statistically significant decline in TCD velocities.
However, it is better to prevent stroke than to treat it. So, these data urge us to evaluate TCD cerebral blood flow velocities comparing hydroxyurea therapy versus blood transfusion for prevention of primary stroke in sickle cell patients.
Evidence for primary stroke prevention was limited to observational data. Three studies found decreased stroke rates in those administered hydroxyurea compared with no treatment [24,25,26].
Hydroxyurea, the only medication approved as a disease-modifying agent by the United States Food and Drug Administration and the European Medicines Agency, and is probably associated with decreased mortality among children with SCD. It is usually under-used, especially in developing countries [26, 27]. Ware et al. [23] stated that, HU lower TCD velocities, which lower the risk of stroke. These data support the results of the current study. Our results showed that, patients receiving HU therapy had lower TCD velocities, these results were in agreement with [8, 28] who found that, patients receiving HU had reduced TCD velocities.
Our results were also in concord with the study by Kratovil et al. [29] who assessed the effect of HU on TCD velocities, reported lower velocities in comparison with no HU. Also, Gulbis et al. [30] which stated that, HU may decrease risk of primary stroke in patients with SCD. Platt [15] concluded that, HU therapy reduces CBF, though less effective, HU maybe considered an alternative to chronic transfusion therapy, where transfusion is not feasible. Also with [31] who reported that HU appears to significantly reduce TCD velocities in Nigerian patients with SCA and elevated velocities with beneficial effect on the hematological profile, he added HU may provide an effective approach to primary stroke prevention, particularly in Africa.
This study showed a higher hematocrit percent was associated with lower TAMV in SCA patients. This was consistent with the findings of [8, 20, 32] which reported an association between decline in TCD velocities and increase in Hct percent in their patients while on HU therapy, and with [33] who stated that TCD values were inversely correlated with the hematocrit. Moreover, many other studies on HU-treated patients have shown the same findings [8, 34]. These results support the results of the present study.
Our study showed 5 (25%) patients had conditional velocities, TAMV > 170 cm/s, while 2 (10%) patients had an abnormal TAMV > 200 cm/s (TAMV of 293.2 cm/s and 240.8 cm/s), but clinically they remained stable. This was in agreement with [11].
In the view of these facts, cerebral arterial flow velocities obtained by TCD were lower in HU-treated SCA patients than in transfusion patients. It is possible that, a lower Doppler velocity in HU group due higher level of Hb, Hb F and decreased HbS. Hence, in hydroxyurea treated patients a different Doppler velocity range for stroke could be obtained. Further studies are needed in large sample size with long follow up, to see whether doppler limits needs to be recalibrated for such risk in HU treated patients with Sickle cell anaemia for better inference and to increase the power of the study. Our personal opinion that HU therapy and TCD screening represents a major step to prevent stroke.
References
Renella R (2016) Clinically-oriented proteomic investigation of sickle cell disease: opportunities and challenges. Proteomics Clin Appl. doi:10.1002/prca.201500133
Huttenlocher PR, Moohr JW, Johns L, Brown FD (1984) Cerebral blood flow in sickle cell cerebrovascular disease. Pediatrics 73(5):615–621
Ohene-Frempong K, Weiner SJ, Sleeper LA, Miller ST, Embury S, Moohr JW, Wethers DL, Pegelow CH, Gill FM (1998) Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 91(1):288–294
Balkaran B, Char G, Morris JS, Thomas PW, Serjeant BE, Serjeant GR (1992) Stroke in a cohort of patients with homozygous sickle cell disease. J Pediatr 120(3):360–366
Adams RJ, Nichols FT III, Aaslid R, McKie VC, McKie K, Carl E, Stephens S, Thompson WO, Milner P, Figueroa R (1990) Cerebral vessel stenosis in sickle cell disease: criteria for detection by transcranial Doppler. Am J Pediatr Hematol Oncol 12(3):277–282
Suliman H, Wali Y, Al Saadoon M, Zechariah M, William RR, Gujjar A, Pathare A (2009) Hydroxyurea or chronic exchange transfusions in patients with sickle cell disease: role of transcranial Doppler ultrasound in stroke prophylaxis. J Pediatr Hematol Oncol 31(1):42–44. doi:10.1097/MPH.0b013e318190d707
Rothman SM, Fulling KH, Nelson JS (1986) Sickle cell anemia and central nervous system infarction: a neuropathological study. Ann Neurol 20(6):684–690. doi:10.1002/ana.410200606
Zimmerman SA, Schultz WH, Burgett S, Mortier NA, Ware RE (2007) Hydroxyurea therapy lowers transcranial Doppler flow velocities in children with sickle cell anemia. Blood 110(3):1043–1047. doi:10.1182/blood-2006-11-057893
Switzer JA, Hess DC, Nichols FT, Adams RJ (2006) Pathophysiology and treatment of stroke in sickle-cell disease: present and future. Lancet Neurol 5(6):501–512. doi:10.1016/s1474-4422(06)70469-0
Adams R, McKie V, Nichols F, Carl E, Zhang DL, McKie K, Figueroa R, Litaker M, Thompson W, Hess D (1992) The use of transcranial ultrasonography to predict stroke in sickle cell disease. N Engl J Med 326(9):605–610. doi:10.1056/nejm199202273260905
Brousse V, Gandhi S, de Montalembert M, Height S, Dick MC, O’Driscoll S, Abihsera G, Rees DC (2013) Combined blood transfusion and hydroxycarbamide in children with sickle cell anemia. Br J Haematol 160(2):259–261. doi:10.1111/bjh.12104
Wang WC, Ware RE, Miller ST, Iyer RV, Casella JF, Minniti CP, Rana S, Thornburg CD, Rogers ZR, Kalpatthi RV, Barredo JC, Brown RC, Sarnaik SA, Howard TH, Wynn LW, Kutlar A, Armstrong FD, Files BA, Goldsmith JC, Waclawiw MA, Huang X, Thompson BW (2011) Hydroxycarbamide in very young children with sickle-cell anemia: a multicentre, randomised, controlled trial (BABY HUG). Lancet 377(9778):1663–1672. doi:10.1016/s0140-6736(11)60355-3
Ware RE, Steinberg MH, Kinney TR (1995) Hydroxyurea: an alternative to transfusion therapy for stroke in sickle cell anemia. Am J Hematol 50(2):140–143
Akingbola TS, Kolude B, Aneni EC, Raji AA, Iwara KU, Aken’Ova YA, Soyannwo OA (2011) Abdominal pain in adult sickle cell disease patients: a nigerian experience. Ann Ib Postgrad Med 9(2):100–104
Platt OS (2005) Preventing stroke in sickle cell anemia. N Engl J Med 353(26):2743–2745. doi:10.1056/NEJMp058274
Curtis SA, Danda N, Etzion Z, Cohen HW, Billett HH (2015) Elevated steady state WBC and platelet counts are associated with frequent emergency room use in adults with sickle cell anemia. PLoS ONE 10(8):e0133116. doi:10.1371/journal.pone.0133116
Gorman MJ, Nystrom K, Carbonella J, Pearson H (2009) Submandibular TCD approach detects post-bulb ICA stenosis in children with sickle cell anemia. Neurology 73(5):362–365. doi:10.1212/WNL.0b013e3181ae2361
Adams RJ, McKie VC, Hsu L, Files B, Vichinsky E, Pegelow C, Abboud M, Gallagher D, Kutlar A, Nichols FT, Bonds DR, Brambilla D (1998) Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med 339(1):5–11. doi:10.1056/nejm199807023390102
Adewoyin AS (2015) Management of sickle cell disease: a review for physician education in Nigeria (sub-saharan Africa). Anemia 2015:791498. doi:10.1155/2015/791498
Lagunju I, Sodeinde O, Telfer P (2012) Prevalence of transcranial Doppler abnormalities in Nigerian children with sickle cell disease. Am J Hematol 87(5):544–547. doi:10.1002/ajh.23152
Segal JB, Strouse JJ, Beach MC, Haywood C, Witkop C, Park H, Wilson RF, Bass EB, Lanzkron S (2008) Hydroxyurea for the treatment of sickle cell disease. Evid Rep Technol Assess 165:1–95
Fasola FA, Odaibo GN, Aken’Ova YA, Olaleye OD (2003) Hepatitis B and C viral markers in patients with sickle cell disease in Ibadan, Nigeria. Afr J Med Med Sci 32(3):293–295
Ware RE, Davis BR, Schultz WH, Brown RC, Aygun B, Sarnaik S, Odame I, Fuh B, George A, Owen W, Luchtman-Jones L, Rogers ZR, Hilliard L, Gauger C, Piccone C, Lee MT, Kwiatkowski JL, Jackson S, Miller ST, Roberts C, Heeney MM, Kalfa TA, Nelson S, Imran H, Nottage K, Alvarez O, Rhodes M, Thompson AA, Rothman JA, Helton KJ, Roberts D, Coleman J, Bonner MJ, Kutlar A, Patel N, Wood J, Piller L, Wei P, Luden J, Mortier NA, Stuber SE, Luban NL, Cohen AR, Pressel S, Adams RJ (2016) Hydroxycarbamide versus chronic transfusion for maintenance of transcranial doppler flow velocities in children with sickle cell anemia-TCD with transfusions changing to hydroxyurea (TWiTCH): a multicentre, open-label, phase 3, non-inferiority trial. Lancet 387(10019):661–670. doi:10.1016/s0140-6736(15)01041-7
Italia K, Jain D, Gattani S, Jijina F, Nadkarni A, Sawant P, Nair S, Mohanty D, Ghosh K, Colah R (2009) Hydroxyurea in sickle cell disease—a study of clinico-pharmacological efficacy in the Indian haplotype. Blood Cells Mol Dis 42(1):25–31. doi:10.1016/j.bcmd.2008.08.003
Voskaridou E, Christoulas D, Bilalis A, Plata E, Varvagiannis K, Stamatopoulos G, Sinopoulou K, Balassopoulou A, Loukopoulos D, Terpos E (2010) The effect of prolonged administration of hydroxyurea on morbidity and mortality in adult patients with sickle cell syndromes: results of a 17-year, single-center trial (LaSHS). Blood 115(12):2354–2363. doi:10.1182/blood-2009-05-221333
Lobo CL, Pinto JF, Nascimento EM, Moura PG, Cardoso GP, Hankins JS (2013) The effect of hydroxcarbamide therapy on survival of children with sickle cell disease. Br J Haematol 161(6):852–860. doi:10.1111/bjh.12323
Iughetti L, Bigi E, Venturelli D (2016) Novel insights in the management of sickle cell disease in childhood. World J Clin Pediatr 5(1):25–34. doi:10.5409/wjcp.v5.i1.25
Thornburg CD, Files BA, Luo Z, Miller ST, Kalpatthi R, Iyer R, Seaman P, Lebensburger J, Alvarez O, Thompson B, Ware RE, Wang WC (2012) Impact of hydroxyurea on clinical events in the BABY HUG trial. Blood 120(22):4304–4310; quiz 4448. doi:10.1182/blood-2012-03-419879
Kratovil T, Bulas D, Driscoll MC, Speller-Brown B, McCarter R, Minniti CP (2006) Hydroxyurea therapy lowers TCD velocities in children with sickle cell disease. Pediatr Blood Cancer 47(7):894–900. doi:10.1002/pbc.20819
Gulbis B, Haberman D, Dufour D, Christophe C, Vermylen C, Kagambega F, Corazza F, Devalck C, Dresse MF, Hunninck K, Klein A, Le PQ, Loop M, Maes P, Philippet P, Sariban E, Van Geet C, Ferster A (2005) Hydroxyurea for sickle cell disease in children and for prevention of cerebrovascular events: the Belgian experience. Blood 105(7):2685–2690. doi:10.1182/blood-2004-07-2704
Lagunju I, Brown BJ, Sodeinde O (2015) Hydroxyurea lowers transcranial Doppler flow velocities in children with sickle cell anemia in a Nigerian cohort. Pediatr Blood Cancer 62(9):1587–1591. doi:10.1002/pbc.25529
Bernaudin F, Verlhac S, Arnaud C, Kamdem A, Chevret S, Hau I, Coic L, Leveille E, Lemarchand E, Lesprit E, Abadie I, Medejel N, Madhi F, Lemerle S, Biscardi S, Bardakdjian J, Galacteros F, Torres M, Kuentz M, Ferry C, Socie G, Reinert P, Delacourt C (2011) Impact of early transcranial Doppler screening and intensive therapy on cerebral vasculopathy outcome in a newborn sickle cell anemia cohort. Blood 117(4):1130–1140; quiz 1436. doi:10.1182/blood-2010-06-293514
Brass LM, Pavlakis SG, DeVivo D, Piomelli S, Mohr JP (1988) Transcranial Doppler measurements of the middle cerebral artery. Effect of hematocrit. Stroke 19(12):1466–1469
Hokazono M, Silva GS, Silva EM, Braga JA (2011) Results from transcranial Doppler examination on children and adolescents with sickle cell disease and correlation between the time-averaged maximum mean velocity and hematological characteristics: a cross-sectional analytical study. Sao Paulo Med J 129(3):134–138
Author information
Authors and Affiliations
Contributions
SMM and AFT designed the study, analyzed the data and wrote the manuscript. HAH and SMM collected data, AFT revised the paper and approved the final version. MAS and SMM helped design the study, drafted and revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests.
Ethical Approval
Patients were invited to participate in the study after getting informed consent and the steps and aim of the research were explained to participants The authors assert that all procedures performed in this study were in accordance with the ethical standards of the institutional committee of medical ethics and with the 1964 Helsinki declaration.
Informed Consent
Informed consent was obtained from all individual participants included in the study. Research involving human participants.
Rights and permissions
About this article
Cite this article
Moeen, S.M., Thabet, A.F., Hasan, H.A. et al. Lower Transcranial Doppler Flow Velocities in Sickle Cell Anemia Patients on Hydroxyurea: Myth or Fact. Indian J Hematol Blood Transfus 34, 97–103 (2018). https://doi.org/10.1007/s12288-017-0814-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-017-0814-z