Abstract
Although the deterioration in pulmonary functions is a well-known important problem due to the treatment of the Hodgkin’s lymphoma patients, the immediate and long term effects of the therapy and its distinctive components were not shown clearly yet. We planned to investigate effects of multiple agent chemotherapy and/or radiotherapy to pulmonary functions immediately and thereafter and the possible effects of the managing this situation. 34 patients were included the study. The patients were evaluated for peak expiratory flow (PEF), forced expiratory volume in 1 s (FEV1), forced expiratory vital capacity (FVC), mean total lung capacity (TLC) values, FEV1/FVC ratio, diffusing capacity for carbonmonoxide (DLco), diffusing capacity for carbonmonoxide corrected for hemoglobin concentration (DLCO) before and at 1, 6 and 12 months after the initiation of the treatment. Demographic characteristics; disease stages; chemotherapy protocols; whether radiotherapy is received; if yes, the region and the dose received were recorded. The tests were finally analysed in two separated groups; group A treated with only chemotherapy and group B; treated with combination therapy, chemotherapy and radiotherapy. In group A, FVC and FEV1 is similar before and after treatment. FEV1/FVC ratio was increased (P = 0.0001) in this group despite increasing in mean TLC values (P = 0.001). No meaningful changes were observed in PEF and DLCO values in group A. In group B, FVC, FEV1 and PEF were decreased after treatment (for FVC P = 0.028, for FEV1 P = 0.04). Despite a decrease in first month of the treatment in FEV1/FVC ratio and DLco these two parameters were recovered at the end of the first year in group B patients. TLC values were increased after treatment in group B as in group A (P = 0.035). We believe that, if these patients are managed well in 1 year; necessary precautions are provided; and patients are well-informed, then there wouldn’t be too much risk and mortality rate for long-term side effects of ABVD and mediastinal RT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hodgkin lymphoma (HL) is a lymphoproliferative disease, which constitutes 1 % of all malignancies. Recently, long-term disease-free survival rate has been achieved approximately at 80 % in all stages of the disease and histological subtypes. The target of modern treatments is to decrease treatment-related toxicities to the minimum level by using the recent improvements in chemotherapy and radiotherapy methods. However, short- and long-term side effects related to the treatments can be encountered [1]. Pulmonary complications, which are encountered related to chemotherapy and radiotherapy treatments in patients with HL are pneumonia, pulmonary fibrosis, obstructive and restrictive changes in respiratory function tests, and pleural effusion [2]. In this present study, it was planned to investigate effects of multiple agent chemotherapy and/or radiotherapy to pulmonary functions in HL patients.
Material and Methods
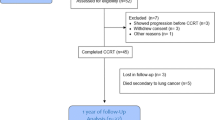
A total of 34 patients with HL, who were diagnosed at the hematology outpatient clinic, and received ABVD treatment, were included into the study, and 12 of them (35.2 %) were female. The study was performed retrospectively by examining the medical records of patients diagnosed with HL.
The study was approved by the local ethics committee of the Istanbul Training and Research Hospital of the Health Ministry. Demographic characteristics; disease stages (according to Ann Arbor Staging System); chemotherapy protocols; whether radiotherapy is received; if yes, the region and the dose received were recorded. Also respiratory function tests of patients were examined before therapy and at the 1st, 6th and 12th months after the treatment. We evaluated the total lung capacity (TLC), forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), FEV1/maximal vital capacity (VCmax) ratio, peak expiratory flow (PEF), carbon monoxide diffusion capacity corrected for haemoglobin concentration (DLCO). Individuals with previously existing pulmonary disease were excluded from the study. Individuals, who required growth factor like filgrastim or lenograstim while receiving ABVD chemotherapy, were excluded from the study, because pulmonary toxicity risk was increased when they were used concomitantly with bleomycin [2]. None of the patients has taken concomitant medicines with pulmonary toxicities. Prognostic factors were defined according to IPI and EORTC [3] criteria. Performance states of patients were defined according to WHO/ECOG [4, 5] criteria. EORTC criteria were used for the early stage patients, and IPS prognostic criteria were used for the advanced stage. During data analysis, comparisons between the groups were analyzed by using Mann–Whitney U test, and Freidman variance analysis was used for the analysis of repetitive measurements. The level of significance was accepted as P < 0.05. Statistical analyses were performed by using Epi Info Version 3.5.1.
Results
A total of 34 HL patients were included in the study; 12 of them were female (35.2 %) and the remaining (64.8 %) was male. Male/female ratio was calculated as 1.83. When patients were evaluated according to Eastern Cooperative Oncology Group (ECOG) performance status, 29 patients (85.3 %) had ECOG 0; and 5 patient (14.7 %) had ECOG 1. Mean follow up duration for patients was 12 months. Median age was 39.2 (min = 16 and max = 65) years.
When histopathological distribution of patients with HL diagnosis was examined, 3 patients (8.8 %) had nodular lymphocyte predominant type; 10 patients (29.4 %) had mixed cellular; 21 patients (61.8 %) had nodular sclerosing type. Nodal involvement was present in mediastinal area in 8 patients (23.5 %), and extramediastinal nodal involvement was present in 26 patients (76.5 %). Moreover, extranodal involvement was present in 2 patients (5.8 %). Three patients (8.8 %) had bulky mass. Of patients, 5 (14.7 %) had spleen and 4 (11.7 %) had bone marrow involvements. Presence of B symptoms was detected in anamnesis of 22 patients (64.7 %). According to Ann Arbor staging system at the time of diagnosis, 7 patients (20.6 %) were in Stage I; 8 (23.5 %) were in Stage II; 12 (35.3 %) were in Stage III; and 7 (20.6 %) were in Stage IV (Table 1).
ABVD chemotherapy, doxorubicin (adriamycin) 25 mg/m2, bleomycin 10 mg/m2, vincristine 1.4 mg/m2 (maximum 2 mg), dacarbazine (DTIC) 375 mg/m2, was applied as the first choice treatment in every 15 days. Four patients (11.7 %) received 2 courses; 6 patients (17.6 %) had 4 courses; 5 patients (14.7 %) had 6 courses; and 19 patients (66 %) had 8 courses of ABVD.
Eighteen patients (52.9 %) received radiotherapy, which was directed to the involved area. Of patients, 11 (61.1 %) received cervical, and 7 (38.9 %) received mediastinal radiotherapy (Table 2). Mean dose of mediastinal radiotherapy was 3574.3 cGy (min: 3420; max: 3600 Gy).
After the treatment, 31 patients (91.2 %) had complete remission, whereas 3 patients (8.8 %) were evaluated as primary refractory. The distribution of the treatment protocols of patients with Hodgkin’s lymphoma according to stage, B symptom and bulky states showed in Table 3.
In group A, when mean TLC values before and at 1, 6 and 12 months after the treatment were compared, statistically significant decreases were observed (Table 4). Statistical significance was also detected in FEV1/FVC ratio; first it was decreased and then increased. FEV1/FVC ratios at months 0, 1, 6, and 12 in only CT-receivers were 80.63, 85.13, 83.31 and 92.19, respectively (P = 0.001) and TLCO ratios during the same timelines were 104.31, 96.06, 97.88 and 118.25, respectively (P = 0.0001; Table 4). Mean TLC values 1 month after the treatment were significantly lower than those of the pretreatment in group B (P = 0.035). While statistically significant decrease was detected in DLCO values in months 1 and 6 when compared with the baseline values, increase was detected in year 1 when compared with the baseline (P = 0.009). There were statistical decreases in PEF, FEV1 and FVC values when compared with the baseline values. There were statistically significant increases in FEV1/FVC and TLC values in year 1 when compared with the baseline values (P = 0.014 and P = 0.035, respectively; Table 5). None of patients developed pulmonary symptoms in 12-months follow up and there was no death according to pulmonary toxicity.
Mean bleomycin dose was 187 mg (min = 60 and max: 240). Mean dose of mediastinal radiotherapy was 3574.3 cGy, and radiotherapy dose was between 3420 and 3600 cGy.
Discussion
Because high cure rates were achieved by the treatments in HL, the attention was mainly focused on treatment toxicities. Concomitant use of radiotherapy and chemotherapeutics had increased the survival, but these combined treatments could cause lung and cardiac toxicities [6–8]. Inflammation associated with bleomycin is one of the leading causes of death in the Hodgkin’s disease treated with ABVD standard chemotherapy. Toxic effect of treatment significantly affects the quality of life of patients with cancer. We aimed to define pulmonary toxicities, which developed in 12 months duration in patients.
Santoro et al. [9] investigated toxicity differences of different regimens like ABVD and MOPP (nitrogen mustard 6 mg/m2, vincristine 1.4 mg/m2, procarbazine 100 mg/m2, prednisone 40 mg/m2). In mediastinal radiotherapy receiving patients, gonadal dysfunction and acute leukemia incidences in MOPP regimen receivers were increased when compared with ABVD regimen in 7-years follow up, but there was no difference in cardiopulmonary functions between them.
It was shown in some studies that more caution should be paid on toxicities in patients with the massive mediastinal mass in concomitant use of particularly adriamycin and bleomycin with the addition of radiotherapy [10]. In our study, decrease in pulmonary function, which was parallel to this, was detected and this condition was reversible. Pulmonary function was increased 1 year after the treatment, and it was statistically significant. There was no relationship between the RT of the head and neck region and pulmonary toxicity.
Pulmonary toxicity due to one of the most frequently used chemotherapy agents, bleomycin, is important. The risk is increased particularly in subjects, who received mediastinal radiotherapy before or during bleomycin; total bleomycin dose over 300–400 U; were aged over 70 years; and high dose oxygen treatment after it. In our study total bleomycine dose was average 250 U. Radiotherapy was given after bleomisin chemotherapy. Additionally toxicity can be observed at all dose levels and ages. Our patients median age was 39.2 (min = 16 and max = 65) years. Bleomycin related toxicity caused mortality observed 6 courses of ABVD was estimated at 1–3 % [11].
In the study of Evens et al. [12], bleomycin related pulmonary toxicity was up to 32 %, mortality rates were reported as 25 %.
Pulmonary function tests of 119 patients, who received only mediastinal radiotherapy; bleomycin in addition to mediastinal radiotherapy; and bleomycin-only, were examined in a study conducted at the Stanford University. Respiratory function tests were performed before and 15 and 36 months after the treatment. During the follow up, 15 months after the treatment was completed, decreases in forced vital capacity (FVC) and carbon monoxide diffusion capacity (DLCO) values were observed, and then the recovery was observed at the month 36. This decrease was prominent especially in patients receiving mediastinal radiotherapy, and the recovery was limited. No severe pulmonary problem requiring hospitalization was observed [13].
In our study, recovery in the pulmonary functions was observed earlier than observed in the study of Horning et al. (at the 12th month rather than 36th). In another study conducted about toxicity of bleomycin and involved region radiotherapy on early stage (IA–IIA) HL patients, impaired respiratory function with cough and dyspnea were detected in 14 out of 30 patients. And it was concluded that the applied treatment was related to pulmonary toxicity [14]. In the study performed by Hirsch et al., patients received 6 courses of ABVD chemotherapy and mantle or mediastinal radiotherapy was applied additionally in 30 patients.
Respiratory function tests were performed before treatment, after chemotherapy and after radiotherapy. When FVC and DLCO values 6 months after the treatment were compared with the values before the treatment in ABVD-only receivers and patients, who received involved area or mediastinal radiotherapy after ABVD, statistically significant decrease was observed. Investigators reported that bleomycin dose modification might be required in acute pulmonary toxicity related to ABVD chemotherapy, and radiotherapy caused an additional decrease in FVC. However, they reported that normal daily activities of none of patients were affected [15]. Although pulmonary functions of our patients were affected, pulmonary functions recovered at the 12th month and there was no relationship with head and neck RT. In a study, no cardiopulmonary symptom was observed in HL patients, who received <30 Gy low dose (mean 2340 cGy) involved area radiotherapy in addition to MOPP/ABVD (mean adriamycin dose was 233 mg/m2, bleomycin dose was 92 IU/m2) chemotherapy after 6.3 years of follow up. While there was no significant difference in FVC value, FEV1/FVC value was decreased by 3 % (P = 0.05) [16].
In the study performed on 39 patients, who received 4 courses of ABVD and mediastinal RT in the range of 30–41 Gy by Villani et al. [17], respiratory function tests were performed at the end, and 1 year after the treatment. Decreases in FEV1, TLC, VC and DLCO values were observed at the end of treatment, and this decrease continued 1 year after the treatment, which was different from our study result.
In our study; in gorup A, statistically significant decreases were observed in mean TLC values, which started at the first month after the treatment, when these values at 1, 6, and 12 months after the treatment were compared with the mean values before the treatment, which is a different finding from the literature. Statistically significance was detected in FEV1/FVC ratio; firstly the decrease and then the increase were detected. There were no significant changes in PEF, FEV1, FVC and DLCO values in group A.
In group B, mean TLC values at the 1st month were statistically significantly lower than the ones at the 12th month after the treatment. While there were statistically significant decreases in DLCO values at months 1 and 6 when compared with the baseline, there was an increase in the first year when compared with the baseline (P = 0.09). There were also statistically significant decreases in PEF, FEV1 and FVC at the first year when compared with the baseline (P = 0.017, P = 0.04, and P = 0.028, respectively). There were statistically significant increases in FEV1/FVC and TLC values at the first year when compared with the baseline (P = 0.014, and P = 0.035, respectively).
Although respiratory function impairment was detected in HL patients receiving multiple chemotherapeutics, especially bleomycin and mediastinal radiotherapy, it was decided that these treatments should be used with consideration of possible side effects because of the successful outcomes of these treatments [18].
According to a new review which focuses on bleomycin and its toxicity; new guidelines were suggested. For example, carefully assessment for symptoms or signs suggestive of pulmonary toxicity, performing DLCO/FVC tests, restriction of the total dose of bleomycin to less than 400 IU, ceasing smoking, limiting as much as possible the inhaled oxygen concentration (<30 %) are some of these suggestions [19].
In our study, although pulmonary functions were affected by ABVD regimen and radiation treatment used in Hodgkin lymphoma, the recovery was observed in 12 months. Patients were advised to be more careful, and not to miss their annual influenza vaccinations. If a patient has anatomic or functional asplenia (due to splenectomy or splenic irradiation), we recommend immunization with the polyvalent S. pneumoniae, conjugate quadrivalent meningococcal polysaccharide, and conjugate H. influenzae type b vaccines for every 6 years. So immunization is particularly important for patients with compromised immune systems.
In conclusion, because pulmonary symptoms were absent, and pulmonary functions of patients were recovered at the 12th month in our patient group, we believe that, if these patients are managed well in 1 year; necessary precautions are provided; and patients are well-informed, mortality risk can be lowered; then there wouldn’t be too much risk for long term side effects of ABVD and mediastinal RT. Finally these findings must now be tested in larger clinical trials but can be used to guide the design of future trials.
References
Klimm B, Engert A, Diehl V (2006) First-line treatment of Hodgkin’s lymphoma. Curr Hematol Malig Rep 1(1):51–59
Lanzkowsky P (2005) Manuel of pediatric hematology and oncology, 4th edn. Elsevier Inc., Amsterdam, pp 453–490
Josting A, Franklin J, May M, Koch P, Beykirch MK, Heinz J, Rudolph C, Diehl V, Engert A (2002) New prognostic score based on treatment outcome of patients with relapsed Hodgkin’s lymphoma registered in the database of the German Hodgkin’s Lymphoma Study Group. J Clin Oncol 20:221–230
Zubrod CG, Ipsen J, Frei E, Lasagna LC, Lipsett MB, Gehan E, Escher GC (1960) Newer techniques and some problems in cooperative group studies. Natl Cancer Inst Monogr 3:277–292
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Cosset JM, Henry-Amar M, Meerwaldt JH (1991) Long-term toxicity of early stages of Hodgkin’s disease therapy: the EORTC experience. EORTC Lymphoma Cooperative Group. Ann Oncol 2(Suppl 2):77–82
Straus DJ (1995) High-risk Hodgkin’s disease prognostic factors. Leuk Lymphoma 15(Suppl 1):41–42
Hagberg H, Killander A, Simonsson B (1983) Serum β-2 microglobulin in malignant lymphoma. Cancer 51(12):2220–2225
Santoro A, Bonadonna G, Valagussa P, Zucali R, Viviani S, Villani F, Pagnoni AM, Bonfante V, Musumeci R, Crippa F (1987) Long-term results of combined chemotherapy-radiotherapy approach in Hodgkin’s disease: superiority of ABVD plus radiotherapy versus MOPP plus radiotherapy. J Clin Oncol 5(1):27–37
Lagrange JL, Thyss A, Caldani C, Héry M, Schneider M, Bensadoun JR (1988) Toxicity of a combination of ABVD chemotherapy and mediastinal irradiation for Hodgkin’s disease patients with massive initial mediastinal involvement. Bull Cancer 75(8):801–806
Jules-Elysee K, White DA (1990) Bleomycin-induced pulmonary toxicity. Clin Chest Med 11(1):1–20
Evens AM, Helenowski I, Ramsdale E, Nabhan C, Karmali R, Hanson B, Parsons B, Smith S, Larsen A, McKoy JM, Jovanovic B, Gregory S, Gordon LI, Smith SM (2012) A retrospective multicenter analysis of elderly Hodgkin lymphoma: outcomes and prognostic factors in the modern era. Blood 119(3):692–695
Horning SJ, Adhikari A, Rizk N, Hoppe RT, Olshen RA (1994) Effect of treatment for Hodgkin’s disease on pulmonary function: results of a prospective study. J Clin Oncol 12(2):297–305
Bates NP, Williams MV, Bessell EM, Hudson GV, Hudson BV (1994) Efficacy and toxicity of vinblastine, bleomycin, and methotrexate with involved-field radiotherapy in clinical stage IA and IIA Hodgkin’s disease: a British National Lymphoma Investigation pilot study. J Clin Oncol 12(2):288–296
Hirsch A, Vander Els N, Straus DJ, Gomez EG, Leung D, Portlock CS, Yahalom J (1996) Effect of ABVD chemotherapy with and without mantle or mediastinal irradiation on pulmonary function and symptoms in early-stage Hodgkin’s disease. J Clin Oncol 14(4):1297–1305
Salloum E, Tanoue LT, Wackers FJ, Zelterman D, Hu GL, Cooper DL (1999) Assessment of cardiac and pulmonary function in adult patients with Hodgkin’s disease treated with ABVD or MOPP/ABVD plus adjuvant low-dose mediastinal irradiation. Cancer Invest 17(3):171–180
Villani F, Fede Catania A, Laffranchi A, Maffioli L, Viviani S, Bonfante V (2003) Effect of an intensive chemotherapy followed by mediastinal irradiation on pulmonary and cardiac function in advanced Hodgkin’s disease. Cancer Invest 21(2):185–192
Ho P, Sherman P, Grigg A (2012) Intermittent granulocyte colony-stimulating factor maintains dose intensity after ABVD therapy complicated by neutropenia. Eur J Haematol 88(5):416–421
Villani F, De Maria P, Bonfante V, Viviani S, Laffranchi A, Dell’oca I, Dirusso A, Zanini M (1997) Late pulmonary toxicity after treatment for Hodgkin’s disease. Anticancer Res 17(6D):4739–4742
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guner, S.I., Yanmaz, M.T., Selvi, A. et al. Chemotherapy and Radiation Induced Pulmonary Dysfunction in Hodgkin Lymphoma Patients. Indian J Hematol Blood Transfus 32, 431–436 (2016). https://doi.org/10.1007/s12288-015-0619-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-015-0619-x