Abstract
Introduction
Neoadjuvant treatment has been widely used for patients with advanced breast cancer, and pathological complete response (pCR) has been proposed as a surrogate marker. However, more than 50% of patients will not achieve pCR and an appropriate, practical prognostic marker is required for these patients.
Materials and methods
A retrospective analysis of patients treated with neoadjuvant treatment for stage I–III disease was performed. Clinicopathological data including the neutrophil-to-lymphocyte ratio (NLR) were collected. NLRs were collected serially according to the treatment schedule. Changes in NLRs were calculated, of which the performance capacity as a prognostic factor was evaluated, and a Kaplan–Meier plot was developed and compared with the log rank test
Results
Changes in NLRs of each time points of 148 patients were used to assess performance capacity as a prognostic factor for invasive disease-free survival (IDFS), overall survival (OS) and distant disease-free survival (DDFS), and that of shortly prior to the third cycle treatment showed statistical significance. With a cut off value of 0.1258, patients could be divided into high- and low-risk of invasive disease recurrence. Kaplan–Meier curves were developed and the log rank test showed that patients in high-risk group after 2 cycles of neoadjuvant treatment were significantly correlated with worse survival outcomes than those in low-risk group.
Conclusion
Changes in NLRs after neoadjuvant treatment showed statistically significant correlation with patient survival and could categorize patients into high- and low-risk groups. Larger, prospectively designed clinical trials are required to substantiate findings of this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant systemic treatment in breast cancer was initially introduced to improve surgical outcomes in patients with locally advanced disease. Since then, its application has expanded and it now enables the direct assessment of treatment response by pathological analysis of resected tissue, and is a strong prognostic factor, like with pathological complete response (pCR) [1,2,3,4].
pCR, one of the parameters indicating a response to treatment, is a strong, individualized prognostic marker for patients with neoadjuvant treatment [1,2,3, 5]. However, not all patients can achieve pCR and more than half of them will have residual disease after neoadjuvant treatment [6,7,8]. pCR is also dependent on breast cancer subtype. Patients with triple negative breast cancer (TNBC) and human epidermal growth factor receptor-2 (HER-2) positive disease have higher chance of to achieving pCR than patients with estrogen receptor(ER) positive breast cancer, and their pCR rate still ranges from 30 to 50% [6,7,8]. Failure to achieve pCR does not always mean disease recurrence, especially in slowly proliferating disease such as ER positive, luminal A cancer, suggesting that prediction of survival with pCR is dependent on tumor biology [5, 9].Taken together, complicating features of non-pCR disease need a careful approach since only an appropriate selection and careful escalation of treatment can improve patient outcomes. Therefore, appropriate biological markers are required to indicate the prognosis in terms of survival [3, 10, 11].
Elevated neutrophil to lymphocyte ratio (NLR) is known correlated with poor prognosis in many solid cancers, including breast cancer [12,13,14]. In breast cancer, subsequent NLR after treatment, such as NLR at 5 years after primary treatment showed statistically significant prognostic power for late recurrence, suggesting that NLR can reflect treatment response as it may change according to the host–tumor interaction during the treatment [15].
The aim of this study was to assess whether changes in NLRs after preoperative systemic treatment correlate with survival benefit such as invasive disease-free survival, overall survival and recurrence-free survival.
Materials and methods
Study cohort
A retrospective cohort was developed with female patients who were triaged into neoadjuvant systemic treatment for stage I–III primary breast cancer diagnosed between 2000 and 2014 and completed all phases of treatment at Wonju Severance Hospital, Yonsei University Wonju College of Medicine. The Institutional review board approved this study (CR318108) and waived off the need for an informed consent due to the retrospective nature of this study. All records were coded under the IRB data monitoring body and kept by a neutral person who was blinded from this study’s analysis (IC). Survival analysis was based on two databases, one from Wonju Severance Hospital and the other from the Korean National Cancer Registry.
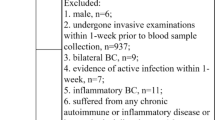
Inclusion and exclusion criteria
Patients were eligible if they had stage I–III breast cancer and completed planned systemic and local treatment at Wonju Severance Hospital,Yonsei University Wonju College of Medicine. Patients with stage IV disease were excluded. Patients who refused surgical treatment after neoadjuvant treatment were also excluded. Neoadjuvant treatment was not recommended for patients with connective tissue diseases, such as systemic lupus erythematosus, unless the patient had inoperable or metastatic disease. This is because radiation treatment following breast conserving surgery was not recommended for this group of patients during the study period according to the institutional policy.
Systemic treatment
Standard regimens which Health Insurance Review & Assessment service (HIRA) provided reimbursement plan, a review body for government-run health insurance system, were used. Six cycles of 500 mg/m2 fluorouracil, 50 mg/m2 doxorubicin, and 500 mg/m2 cyclophosphamide intravenously administered once every 3 weeks (FAC) for node negative patients. For patients with pathologically proven nodal metastasis, Taxen-based regimen was introduced; A total 4 cycles of Doxorubicin 50 mg/m2 IV, with cyclophosphamide 500 mg/m2 IV(AC) were repeat every 3 weeks and subsequent 4 cycles Paclitaxel 80 mg/m2 IV(T) every 3 weeks (AC followed by T): T was given either after surgery or in a consecutive manner before surgery. For patients with HER2-positive disease proven by immunohistochemical staining or any in-situ hybridization, trastuzsumab was recommended after surgery only if there was residual disease until HIRA provided reimbursement plan for trastuzumab as one of the regimens for neoadjuvant treatment in 2010. Hormonal treatment for patients with ER-positive disease was given according to the HIRA reimbursement plan; 5-year tamoxifen for premenopausal women or aromatase inhibitor for postmenopausal women.
Collection of data: clinicopathological, laboratory and survival data
Pathologic tumor size and nodal status were determined from the surgical specimen. pCR was defined as ypT0/ypN0, absence of invasive and in-situ cancer cells in the breast and axillary nodes. Complete blood counts (CBC) were collected serially, before any systemic treatment and immediate prior to the 3rd cycle and just prior to the last cycle of systemic treatment. NLR was calculated as the serum absolute neutrophil count divided by the serum absolute lymphocyte count, and changes in NLRs were calculated as NRLs at each time points subtracted by NLRs at baseline.
Statistical analysis
Patients’ baseline characteristics were summarized using descriptive statistics. For a comparison of two groups, the Chi squared test or Fisher’s exact test was used for applicable categorical value, and the independent t-test was used for continuous value. Receiver operating curves (ROC) were generated and the area under the curves (AUC) was calculated to assess what extent changes in NLRs were capable of distinguishing higher and lower risk groups of invasive disease free-survival (IDFS), distant disease free- survival(DDFS) and overall survival(OS). The definition of these categories are summarized in supplementary Table 1. Youden’s index was utilized to find the appropriate cut-off value for changes in NLRs. Kaplan–Meier curves were generated to estimate IDFS, OS and DDFS, and the log rank test was used to compare survival of each group. The Cox proportional hazard model was used to estimate hazard ration (HR) with 95% confidence intervals (CI). All statistical analyses were done with SPSS 25 (IBM Corporation, Somers, NY, USA). All p- values were two sided and those less than 0.05 were deemed significant.
Results
Study cohort
148 patients with age distribution of 47.29 ± 8.06 (30–71) completed the planned neoadjuvant systemic treatment and underwent surgery; further adjuvant treatment such as chemotherapy, hormonal treatment or anti HER2 treatment, where applicable, for locally advanced breast cancer. Of 148 patients, 119 were included in this analysis after excluding 29 patients due to stage IV disease. The patients’ clinicopathological characteristics are described in Table 1. Neoadjuvant treatment regimens were decided after clinical assessment, mainly nodal involvement of the disease. The number of patients assigned each regimen is in listed in Table 2. Taxane was introduced in almost half of all patients and hormonal treatment was addressed in 80 patients. Anti HER2 treatment was allowed only as adjuvant treatment for the patients who had residual disease before 2010, and four patients were treated with trastuzumab during neoadjuvant treatment in the study period.
Changes in NLR after 2 cycles of neoadjuvant treatment as prognostic factor
First, ROC curves were generated to measure the performance of changes in two NLRs, baseline and each NLRs according to the treatment schedule, as a predictive factor for IDFS, OS and DDFS, as shown in Fig. 1 and supplementary Fig. 1. The changes between NLRs prior to the third cycle and the baseline NLRs showed strongest performance capacity with statistical significance. The AUC values of each end point of interest are 0.852, 0.716, and 0.764, for IDFS, OS and DDFS, respectively.
Receiver operating characteristics (ROC) curves to define optimal cut-off values for Invasive disease- free survival(IDFS) (a), overall survival (OS) (b) and distant disease free survival(DDFS) (c). IDFS showed the heist performance capacity with AUC 0.852, while AUCs for OS and DDFS were 0.716, and 0.764, respectively. Coordinates of the ROC curves for Youden’s index for OS and IDFS are available from supplementary Table 3 and 4
Date of data cut-off for this analysis, before the 3rd cycle of chemotherapy, allowed about 6 weeks’ exposure to the systemic treatment. Neutrophil and lymphocyte count and NLR values at baseline and prior to the third treatment are summarized in supplementary Table 2. Changes in NLRs between two time points are shown in Fig. 2. In summary, NLR decreased in 57 cases and increased in 61 case. One case showed no difference between the two-time point. The cut-off value was determined at 0.1258 with ROC curves and Youden’s index (Supplementary Table 3 & 4), and patients were categorized into either a high-risk group with increased NLR over 0.1258, or a low-risk group with decreased NLRs less than 0.1258. Median follow-up was 70 ± 43 month (2–202 months) and Kaplan–Meier survival plots were obtained for IDFS, OS and DDFS (Fig. 3).The high-risk group categorized by changes in NLRs showed statistically significant worse survival rates with p value < 0.00. In subgroup analysis, changes in NLRs larger than 0. 1258 also showed tendency of poor prognosis in each subgroup, ER positive, HER2 overexpressed and triple negative breast cancer (supplementary Fig.2–4).
Individual changes in NLRs after 2 cycles of neoadjuvant chemotherapy. Bar length indicates the amount of changes in NLRs. Red and blue color indicate patients with invasive disease recurrence (red) or free from recurrence (blue). Arrow head indicate cases achieved pathological complete response (pCR). Of 11 patients with pathologic complete response (pCR), 2 patients experienced invasive disease recurrence
Association between changes in NLRs and IDFS (a), OS (b), and DDFS (c). Kaplan Meier curves of two groups, high-risk group with change in NLR > 0.1258(blue line), and low-risk group with change in NLR < 0.1258 (red line) were generated and compared with the log rank test. High-risk group showed significantly worse prognosis in all of the IDFS (a), OS (b), and DDFS (c)
Comparison between groups having NLR differences either larger or smaller than 0.1258
Clinicopathological characteristics of each group dichotomized by NLR differences were summarized in Table 3. Two groups with different value of changes in NLRs, either larger or smaller than 0.1258, were not different in terms of previously known prognostic factors such as age, ER, PR, HER2, size of residual disease (as continuous value), pCR, nodal stage, subtype, except number of positive LN (as continuous value). Multivariate analysis with the Cox regression hazard test found nodal involvement and changes in NLRs as independent risk factors for IDFS (Table 4). While changes in NLRs and nodal disease showed statistically significant performance as risk factor, both showed different level of hazard according to whether they were included as continuous value or categorical value (Table 4).
Discussion
This study was designed to find the prognostic factors after neoadjuvant treatment regarding survival, paying particular attention to patients with non-pCR. Patients with non-pCR disease would need escalated treatment, which is in itself risky, while little is known about which recurrent disease could afflict which patient [3, 4, 11]. This study showed that changes in NLRs after neoadjuvant systemic treatment could categorize patients into higher and lower risk groups with statistical significance and patients with decreased NLR after neoadjuvant treatment showed better survival than those without.
We focused on the changes in NLR after neoadjuvant treatment as a parameter reflecting treatment response in terms of survival. Higher NLRs, a potential marker of systemic inflammation is known to be related with poor survival [12, 14, 16]. NLRs are also known to be related to pCR rates, and patients with lower NLRs before any systemic treatment showed better survival rates. Previous studies related to changes in circulating tumor cells (CTCs) after neoadjuvant treatment showed that patients with decreased CTCs after preoperative chemotherapy showed better survival than those without [17, 18]. This led to the question whether decreased NLRs after neoadjuvant treatment, which might reflect the complicated interaction between the innate and adaptive immune response [15, 16], could serve as a prognostic factor in patients with non-pCR, and our findings indicate that this indeed is true.
As the first step, we investigated which NLRs can reflect the changes predicting patients’ survival, and NLRs prior to the third cycle showed the strongest performance capacity to predict patients’ survival. Neither initial NLRs nor last NLRs during the treatment was a prognostic factor in this study. For initial NLRs, unlike other studies which included every eligible patients regardless of preoperative chemotherapy history and showed reliability of their capacity as prognostic factor, this cohort consisted of patients with neoadjuvant treatment, which is usually recommended for the patients with advanced disease. Given that patients who were included in this study could tend to have advanced disease, it is not unexpected that comparison within this group could not yield significant data. Regarding NLRs beyond third cycle of treatment, chemotherapy-induced neutropenia and pancytopenia may interfere exact reflecting hosts and their tumor interaction in terms of immune response.
Factors indicating response to neoadjuvant treatment, such as pCR, biological aspects of residual tumor and CTCs after neoadjuvant treatment, were thoroughly investigated [4, 7, 9, 17, 18].National surgical adjuvant breast and bowel project-18 and European organization for research and treatment reported that pCR was a strong prognostic factor for individual patients while neoadjuvant treatment did not improve or worsen survival, suggesting that treatment response could correlate with patients’ survival [1, 2]. pCR is a strong prognostic factor for individual patients but less than 50% of patients will reach pCR, which will leave unmet clinical needs for more than 50% of patients with non-pCR status. The specific recurrent disease that would affect each non-pCR patients needs additional biological markers other than pathological responses, CTCs, and residual tumor burden because these were investigated with limited success. First, changes of CTCs after systemic treatment statistically strongly stratified patients into higher or lower risk groups [17,18,19] However, CTCs are not widely applicable methods and their clinical utilities remain doubtful [19]. Residual tumor burdens have had limited success with current treatment options [3].
We showed that a change in NLRs was an independent prognostic factor from pCR. Predicting pCR does not always result in better prognosis in terms of survival [7, 9]. For example, tumor infiltrating lymphocytes (TILs), a strong predicting factor of pCR and one of the outcomes of interest after neoadjuvant treatment, is not always correlated with better survival, especially in non-pCR patients [9]. Patients with higher TILs showed better survival regardless of tumor subtype, provided that pCR was achieved. However, patients with non-pCR disease showed no difference in survival even with higher TILs when they had TNBC or HER2 overexpressed disease and interestingly, if patients had ER positive non-pCR disease, higher TILs was related to worse prognosis [9]. Given that patients with ER positive breast cancer usually achieve pCR only in 10–20% of patients [10, 20, 21], TILs cannot be used as a reliable prognostic factor for survival in around 80% of patients with non-pCR disease in this subgroup and cannot be utilized without caution in around 50% of patients with TNBC and HER2 positive non-pCR disease.
NLRs have limitations despite the promising aspect as a prognostic marker, such as easy accessibility, cost-effectiveness and utilizing popular standard test. First, changes in NLR after treatment can be affected by treatment from bone marrow suppression, which will eventually result in major bias in NLRs and can be highly challenging when utilized in clinics. In this study, we used data acquired before the 3rd cycle of the planned treatment, allowing sufficient exposure of the tumor to the treatment, while including all data regardless of GM-CSF use, thereby minimizing bias. Regarding GM-CSF use and patients’ survival, because studies have reported mixed results with better or worse prognosis, analyzing the effect of GM-CSF needs a more sophisticated approach [22, 23]. Considering that there are not enough data to determine the role of GM-CSF and cancer biology, it would be reasonable not to exclude data from patients with history of GM-CSF treatment. Another thing to be mentioned is that while there are many studies suggesting NLRs’ role as a prognostic factor, evidence regarding the mechanism underlying the association between high NLR and poor outcome in cancer patients is limited [15, 24]. Thus this area should be actively investigated to elucidate and take advantage of immune-related therapy during neoadjuvant treatment, especially when it is strongly related with neutropenic events [15, 22, 23].
Limitations of this study were the relatively small number of patients in the TNBC and HER2 positive subgroup, lower pCR rate (which might come from the nature of this study) and the retrospective nature of the study with small population from a single institution. We showed that changes in NLRs can predict patient survival in each subgroup (supplementary Fig. 2–4) but because of the small number of patients in each subgroup, we could not fully address the effect of change in NLRs in each subgroup, which urges larger clinical trials with a high enough number of patients in each subgroup. Another limitation is insufficient data regarding HER2-targeted agents mainly due to regulatory restriction, which markedly affected pCR rate in the relevant patients. Recently positive relationship between increased NLRs and response rate in patient with HER2 overexpressed breast cancer was reported from the clinical trial, “Combination therapy with docetaxel for first-line treatment of HER2-positive metastatic breast cancer in the clinical evaluation of Pertuzumab and Trastuzumab (CLEOPATRA) trial”, suggesting more elaborate data regarding patients’ prognosis is expected in future [24].
In conclusion, changes in NLRs after neoadjuvant treatment showed statistically significant correlation with patients’ survival and could dichotomize patients into two groups; high and low risk of disease recurrence. Because NLRs are numerical values, it can be integrated with existing factors as continuous parameter like Oncotype DX® [25] or as categorical parameter, which is more useful in a clinical setting. Larger, prospectively derived clinical trials are required to substantiate findings from this study.
References
van der Hage JA, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001;19(22):4224–377.
Wolmark N, Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;30:96–102.
Patel SA, DeMichele A. Adding adjuvant systemic treatment after neoadjuvant therapy in breast cancer: review of the data. Curr Oncol Rep. 2017;19(8):56.
Pelizzari G, Gerratana L, Basile D, Fanotto V, Bartoletti M, Liguori A, et al. Post-neoadjuvant strategies in breast cancer: from risk assessment to treatment escalation. Cancer Treat Rev. 2019;72:7–14.
Cain H, Macpherson IR, Beresford M, Pinder SE, Pong J, Dixon JM. Neoadjuvant therapy in early breast cancer: treatment considerations and common debates in practice. Clin Oncol (R Coll Radiol). 2017;29(10):642–52.
von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–804.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384(9938):164–72.
Berruti A, Amoroso V, Gallo F, Bertaglia V, Simoncini E, Pedersini R, et al. Pathologic complete response as a potential surrogate for the clinical outcome in patients with breast cancer after neoadjuvant therapy: a meta-regression of 29 randomized prospective studies. J Clin Oncol. 2014;32(34):3883–911.
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19(1):40–50.
Ellis MJ, Suman VJ, Hoog J, Goncalves R, Sanati S, Creighton CJ, et al. Ki67 proliferation index as a tool for chemotherapy decisions during and after neoadjuvant aromatase inhibitor treatment of breast cancer: results from the American College of Surgeons Oncology Group Z1031 trial (Alliance). J Clin Oncol. 2017;35(10):1061–9.
Masuda N, Lee SJ, Ohtani S, Im YH, Lee ES, Yokota I, et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med. 2017;376(22):2147–59.
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):124.
Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res. 2017;19(1):2.
Noh H, Eomm M, Han A. Usefulness of pretreatment neutrophil to lymphocyte ratio in predicting disease-specific survival in breast cancer patients. J Breast Cancer. 2013;16(1):55–9.
Moon G, Noh H, Cho IJ, Lee JI, Han A. Prediction of late recurrence in patients with breast cancer: elevated neutrophil to lymphocyte ratio (NLR) at 5 years after diagnosis and late recurrence. Breast Cancer. 2019. https://doi.org/10.1007/2Fs12282-019-00994-z.
Patel DA, Xi J, Luo J, Hassan B, Thomas S, Ma CX, et al. Neutrophil-to-lymphocyte ratio as a predictor of survival in patients with triple-negative breast cancer. Breast Cancer Res Treat. 2019;174(2):443–52.
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med. 2004;351(8):781–91.
Paoletti C, Miao J, Dolce EM, Darga EP, Repollet MI, Doyle GV, et al. Circulating tumor cell clusters in patients with metastatic breast cancer: a SWOG S0500 translational medicine study. Clin Cancer Res Epub. 2019. https://doi.org/10.1158/1078-0432.CCR-19-0208.
Alimirzaie S, Bagherzadeh M, Akbari MR. Liquid biopsy in breast cancer: a comprehensive review. Clin Genet. 2019;95(6):643–60.
Ellis MJ, Ma C. Letrozole in the neoadjuvant setting: the P024 trial. Breast Cancer Res Treat. 2007;105(Suppl 1):33–43.
Dowsett M, Ebbs SR, Dixon JM, Skene A, Griffith C, Boeddinghaus I, et al. Biomarker changes during neoadjuvant anastrozole, tamoxifen, or the combination: influence of hormonal status and HER-2 in breast cancer—a study from the IMPACT trialists. J Clin Oncol. 2005;23(11):2477–92.
Reggiani F, Bertolini F. GM-CSF promotes a supportive adipose and lung microenvironment in metastatic breast cancer. Oncoscience. 2017;4(9–10):126–7.
Eubank TD, Roberts RD, Khan M, Curry JM, Nuovo GJ, Kuppusamy P, et al. Granulocyte macrophage colony-stimulating factor inhibits breast cancer growth and metastasis by invoking an anti-angiogenic program in tumor-educated macrophages. Cancer Res. 2009;69(5):2133–40.
Shin H, Kim J, Kim HJ. Neutrophil lymphocyte ratio (NLR) change after systemic treatment as a predictive factor of cancer specific survival in stage IV breast cancer. J Clin Oncol. 2015;33(suppl28):29.
Paik SM, Shak S, Tang G, Kim C, Baker J, Cronin M, et al. A multigene assay to predict recurrence of Tamoxifen treated, node negative breast cancer. N Eng J Med. 2004;351:2817–26.
Acknowledgements
All patients who showed brave courage against breast cancer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards and for this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Choi, H., Noh, H., Cho, IJ. et al. Changes in neutrophil to lymphocyte ratio (NLR) during neoadjuvant treatment correlated with patients’ survival. Breast Cancer 27, 871–879 (2020). https://doi.org/10.1007/s12282-020-01083-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-020-01083-2