Abstract
Purpose
To evaluate interobserver agreement in full-field digital mammography (FFDM) and digital breast tomosynthesis (DBT) in terms of both lesion detection and characterization, and to evaluate the cancer detection rate of standard two-view FFDM compared to various combinations of DBT.
Materials and methods
Thirty-five women (mean age 59.7; range 50–80 years) with 37 breast cancers who underwent both two-view DBT and two-view FFDM were included. DBT images were obtained using an investigational prototype. We performed interobserver agreement analyses using kappa (k) statistics. The cancer detection rate of various combinations of DBT compared to standard two-view FFDM was estimated using a generalized estimation equation.
Results
There was fair to moderate agreement on detectability (k = 0.59–0.62) in both views of FFDM and DBT, while fair to substantial agreement was found for lesion location (k = 0.52–0.84) and fair to moderate agreement for lesion type (k = 0.46–0.70) and BI-RADS final assessment (k = 0.48–0.69). In generalized estimation equations, standard two-view FFDM was inferior to any combination of DBT. The detection rate ratio was significantly higher in the combined four views of DBT and FFDM compared to standard FFDM (p < 0.046).
Conclusion
Our study showed good agreement in lesion detection and characterization between FFDM and DBT images. Our findings also demonstrated that combining DBT and FFDM is superior in detecting cancer compared to standard FFDM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mammography is widely used for breast cancer screening and has been shown to reduce breast cancer mortality rates [1, 2]. However, full-field digital mammography (FFDM) has some limitations, such as a reduced sensitivity by as much as 50 % in dense breast tissue compared to fatty breast tissue resulting from fibroglandular density, which can mask suspicious findings [3, 4], and increased false-positive rates due to superimposition of overlapping tissues, which can obscure masses or other important features of malignancy [5]. As many as 20–30 % of breast cancers can be undetected on FFDM [6].
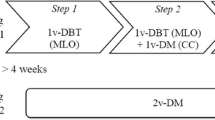
Digital breast tomosynthesis (DBT) is a three-dimensional imaging technique that has demonstrated promise for breast cancer detection. An X-ray tube moves through a limited arc angle and reconstructs the tissue based on thin slices to minimize the influence of overlapping breast structures. DBT is expected to improve mammographic sensitivity for breast cancer detection. Several previous studies have demonstrated the diagnostic performance of DBT compared to that of FFDM and its potential benefits such as reducing recall rates in screening mammography, improving cancer detection in women with dense breast tissue, and improving mammographic specificity by eliminating overlapping tissues, particularly in dense breast tissue, which can reduce false-positive rates and the number of biopsies [7–17]. Studies on DBT published to date have compared one-view DBT (mediolateral oblique (MLO) view) alone [9, 12, 17], two-view DBT (craniocaudal (CC) and MLO view) [18], one-view DBT (MLO view) with one-view FFDM (CC view) [9, 19], or both two-view DBT with two-view FFDM [13–15], to standard two-view FFDM. However, to our knowledge, no studies have compared several different combinations of DBT versus standard two-view FFDM to determine which combination provides the greatest benefit. Understanding the optimal detection method is important because increases in radiation dose can be a concern in clinical practice.
In our current study, interobserver agreement in FFDM and DBT was evaluated in terms of both lesion detection and characterization, and the cancer detection rate of standard two-view FFDM was compared to that of various combinations of DBT. The goal of our analysis was to determine the best technique for clinical application.
Materials and methods
Patients
The study protocol was approved by the institutional review board of our institution, and written informed consent was obtained from all participants. From November 2012 to March 2013, study participation was offered to women who had biopsy-proven breast cancer and were planned to undergo mastectomy. The exclusion criteria were the following: (a) age below 50 years; (b) participants who were planned to undergo neoadjuvant chemotherapy or radiation therapy before surgery; (c) participants who underwent excisional biopsy or mammotome excision for the diagnosis of breast cancer; and (d) mammography limitations due to foreign materials such as implant insertion. We included a final cohort of 37 breast cancers from 35 women (age range 50–80 years; mean age 59.7 years).
Image acquisition
Participants underwent FFDM and DBT imaging of both breasts in the CC and MLO positions. Both imaging studies were acquired within 1 month. Standard FFDM images of each breast were obtained using a commercially available system (Senographe DS; General Electric Medical System, Milwaukee, WI, USA). DBT images were obtained using an investigational prototype version of the Korea Electrotechnology Research Institute (KERI, Ansan, Gyeonggido, Korea), which was developed for clinical evaluation. Fifteen low-dose projection images were obtained with a total tomographic angle of 42° (from −21° to +21° in increments of 3°) acquired in a step-and-shoot mode while the breast was compressed in the fixed position. The usual acquisition time for DBT of the breast was 10 s (Table 1). Using this machine, the radiation dose for the FFDM and DBT for each view was approximately the same and the total dose for the combined FFDM and DBT was less than the Mammography Quality Standards Act (MQSA) limit for a single mammography [20]. DBT projection views were reconstructed into 1-mm thick slices using the filtered back projection technique. DBT was performed by one technologist, who had 5 years of experience in FFDM and had participated in 4 weeks of training for DBT.
Image review and statistical analysis
Three board-certified radiologists (H.H.K., H.J.S., and E.Y.C.) with 8–20 years of breast image experience participated in this study. Each had undergone training in the interpretation of DBT images, and all readers had participated in prior reader studies of interpreting tomosynthesis examinations [18]. Image interpretation was performed per breast, not per patient.
The primary aim of this study was to estimate the reproducibility of assessment across multiple readers using FFDM and DBT for diagnostic purposes. Each radiologist first interpreted FFDM images independently, and after finishing their first assigned mode and after a predetermined time period of 6 months, the readers analyzed the randomly mixed DBT images. The readers were aware that patients had a confirmed breast cancer. The assessment included detectability, breast density (almost entirely fatty, scattered areas of fibroglandular density, heterogeneously dense, and extremely dense), lesion location (upper, lower, mid, and subareolar area in MLO view, outer, inner, mid, and subareolar area in CC view), lesion type (mass without calcification, mass with calcification, calcification only, architectural distortion, and asymmetry), and BI-RADS categorization of final assessment [21]. We performed interobserver agreement analyses using kappa (k) statistics [22]. To interpret the kappa coefficients, we used the following definitions: less/equal to 0 indicates poor agreement; 0.01–0.20 slight agreement; 0.21–0.40 fair agreement; 0.41–0.60 moderate agreement; 0.61–0.80 substantial agreement; 0.81–0.99 almost perfect agreement; and 1.00 perfect agreement [23].
The secondary end point of this study was to evaluate the cancer detection rate of various combinations of DBT compared to standard two-view FFDM. We considered detection when the lesions were seen by at least two readers. DBT (CC and MLO view) + FFDM (CC and MLO view), DBT (CC and MLO view), DBT (MLO view) + FFDM (CC view), DBT (MLO view) and DBT (CC view) were compared to standard FFDM (CC and MLO view). Estimation was done using a generalized estimation equation to estimate the detection rate ratio for each of the outcomes [24]. A p value of <0.05 was considered significant. R 3.0.2 was used for analyses (R 3.0.2 for Windows).
Results
The 37 malignant breast lesions in our study were primary breast cancers, and the histological types were invasive ductal carcinoma (n = 30), ductal carcinoma in situ (n = 4), invasive lobular carcinoma (n = 2), and tubular carcinoma (n = 1). The size of the tumors ranged from 0.6 to 7.4 cm, and the mean size was 2.1 cm. Of the 37 potential detections, individual investigators detected between 28 (75.7 %) and 34 (91.9 %) tumors based on FFDM images, and between 33 (89.2 %) and 36 (97.3 %) based on DBT images. A total of 25 (67.6 %) lesions were detected by the three readers in both CC and MLO views of FFDM and 29 (78.4 %) were detected by the three readers in both CC and MLO views of DBT (Fig. 1). There were three missed cancers, which were not detected by any of the three readers by both views of FFDM, all of which were masses without calcification with a tumor size of 0.6, 0.8, and 1.8 cm, respectively (Fig. 2). None of the three cancers were missed by all three readers using both views of DBT.
Invasive ductal carcinoma in 57-year-old woman. Full-field digital mammgoraphy with craniocaudal (CC) (a) and mediolateral oblique (MLO) view (b) of right breast reveals hyperdense mass with pleomorphic microcalcification (arrow) in upper outer portion. Digital breast tomosynthesis with CC (c) and MLO view (d) in same patient that all three readers detected with good interobserver agreement
Invasive ductal carcinoma in 51-year-old woman. Full-field digital mammgoraphy (FFDM) with craniocaudal (CC) (a) and mediolateral oblique (MLO) view (b) of left breast reveals suspicious isodense mass (arrow) in upper inner portion. Digital breast tomosynthesis with CC (c) and MLO view (d) in same patient that shows improved visibility of cancer and cancer margins (arrow) compared with FFDM. Three readers missed this lesion in FFDM
Among the 111 interpretations by the three readers, more than 61 % of breasts were interpreted as dense breast (Table 2). The most common lesion type was mass without calcification and it showed 55.3 % (57/103) in CC view of DBT, 57.1 % (60/105) in MLO view of DBT, 45.6 % (41/90) in CC view of FFDM and 42.4 % (39/92) in MLO view of FFDM, respectively.
Interobserver agreement was assessed between the three readers (Table 3). There was fair to moderate agreement on detectability (k = 0.59–0.62) in both views of FFDM and DBT. Fair to substantial agreement was found for lesion location (k = 0.52–0.84) and fair to moderate agreement for lesion type (k = 0.46–0.70) and BI-RADS final assessment (k = 0.48–0.69).
In generalized estimation equations, we found standard two-view FFDM was inferior to any combination of DBT (Table 4). The detection rate ratio compared to standard FFDM was 0.946 (95 % CI 0.865–1.000) for DBT (CC and MLO view) + FFDM (CC and MLO view), 0.919 (95 % CI 0.836–1.000) for DBT (CC and MLO view), 0.919 (95 % CI 0.836–1.000) for DBT (MLO view) + FFDM (CC view), 0.892 (95 % CI 0.865–0.973) for DBT (MLO view), and 0.865 (95 % CI 0.738–0.973) for DBT (CC view). The detection rate ratio was significantly higher in the combined four views of DBT and FFDM than in standard FFDM (p < 0.046).
Discussion
In our present study, we found that the interobserver agreement for detectability, lesion location, lesion type, and BI-RADS final assessment was good based on either FFDM or DBT images. Our findings showed that standard two-view FFDM showed the lowest detection rate ratio compared to other combinations of DBT. These results indicate that the use of investigational prototype DBT of the KERI showed similar reliability and better detection than FFDM.
The efficacy of combining digital mammography with tomosynthesis in breast cancer screening has been demonstrated in several studies. Skanne et al. [13] reported increased detection of invasive cancer by 40 %, and another study by Rafferty et al. [16] showed a consistent and statistically significant gain in diagnostic accuracy with combined screening modalities. The recall rate was therefore reduced by 15–37 % [11, 13–16]. This can be expected because adding another modality can provide more information to the radiologist, which could improve the observer performance. Our results showed that combined screening modality with four views of FFDM and DBT was significantly superior to standard FFDM in detecting cancer.
In our present analyses, although the differences were not statistically significant, there was a tendency toward greater cancer detection in four views of FFDM and DBT, two views of DBT or MLO view of DBT with CC view of FFDM, one view of DBT (MLO view), and two views of FFDM. In addition, there were no cancers detected by FFDM which were not seen on DBT. This may be because overlapping tissues, especially in dense breast tissue, are removed during tomosynthesis, and the distribution of fibroglandular tissue is less of a concern, resulting in better characterization of the tissue. These results are in agreement with those of previous studies that showed better cancer detection in single-view tomosynthesis [8] or combination of MLO view of tomosynthesis and CC view of digital mammography [19] compared to standard digital mammography.
Although the number of detected lesion types including calcification did not show big difference between DBT and FFDM, mass without calcification was much better detected and less number of lesions was assessed as asymmetry on DBT. This may be due to the fact that the DBT helps removing the overlapping tissue in dense breast which may obscure the mass lesion and leads to better detection.
Currently, four DBT systems—Selenia Dimensions (Hologic, Bedford, MA, USA); Senographe essential (GE Healthcare, Waukesha, WI, USA); Giotto Image (IMS, Bologna, Italy); and Mammomat Inspiration (Siemens Healthcare, Erlange, Germany)—are commercially available and follow different protocols by their respective manufacturer. In Korea, the KERI has developed prototype breast tomosynthesis units for clinical evaluation. In this study, we described our experience with the use of the investigational prototype version of the KERI.
Radiation dose should also be considered when determining optimal screening modality [25, 26]. In early studies, the radiation dose of tomosynthesis was equal or higher compared to that of digital mammography [26]; however, recent improved tomosynthesis has a similar radiation dose to digital mammography. Our DBT system showed approximately the same radiation dose as digital mammography. Therefore, one-view DBT or other combinations of DBT may show better performance without increasing the radiation dose. In addition, synthesized 2D images (C-view; Hologic, Bedford, MA, USA Volume preview; GE Healthcare, BUC, France), which are approved by the Food and Drug Administration, requires no additional radiation and shows comparable performance to FFDM [27, 28]. Although synthesized 2D images were not available with the systems used in the present study, later versions of the prototype may produce reconstruction of synthesized 2D images, which may show equal radiation dose to FFDM while providing significant diagnostic performance.
Our study had several limitations. First, as we included only patients who underwent mastectomy for malignancy and who volunteered for this study, some degree of selection bias cannot be excluded. Second, we included a relatively small number of patients. Further studies with a larger number of patients are needed. Third, although this was the first study to evaluate interobserver agreement of DBT, we did not evaluate all the findings according to the BI-RADS lexicon. Finally, this was a preliminary single-vendor study in a single institution. Our results need to be validated by other studies.
In conclusion, our study findings showed good agreement in lesion detection and characterization between both FFDM and DBT images. We further found that the combined technique of DBT and FFDM was superior for cancer detection compared to standard FFDM.
References
Tabar L, Vitak B, Chen HH, Yen MF, Duffy SW, Smith RA. Beyond randomized controlled trials: organized mammographic screening substantially reduces breast carcinoma mortality. Cancer. 2001;91:1724–31.
Tabar L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, et al. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology. 2011;260:658–63.
Berg WA. Beyond standard mammographic screening: mammography at age extremes, ultrasound, and MR imaging. Radiol Clin North Am. 2007;45:895–906.
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356:227–36.
Harvey JA, Bovbjerg VE. Quantitative assessment of mammographic breast density: relationship with breast cancer risk. Radiology. 2004;230:29–41.
Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK, Acharyya S, et al. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005;353:1773–83.
Niklason LT, Christian BT, Niklason LE, Kopans DB, Castleberry DE, Opsahl-Ong BH, et al. Digital tomosynthesis in breast imaging. Radiology. 1997;205:399–406.
Andersson I, Ikeda DM, Zackrisson S, Ruschin M, Svahn T, Timberg P, et al. Breast tomosynthesis and digital mammography: a comparison of breast cancer visibility and BIRADS classification in a population of cancers with subtle mammographic findings. Eur Radiol. 2008;18:2817–25.
Gennaro G, Toledano A, di Maggio C, Baldan E, Bezzon E, La Grassa M, et al. Digital breast tomosynthesis versus digital mammography: a clinical performance study. Eur Radiol. 2010;20:1545–53.
Good WF, Abrams GS, Catullo VJ, Chough DM, Ganott MA, Hakim CM, et al. Digital breast tomosynthesis: a pilot observer study. AJR Am J Roentgenol. 2008;190:865–9.
Gur D, Abrams GS, Chough DM, Ganott MA, Hakim CM, Perrin RL, et al. Digital breast tomosynthesis: observer performance study. AJR Am J Roentgenol. 2009;193:586–91.
Wallis MG, Moa E, Zanca F, Leifland K, Danielsson M. Two-view and single-view tomosynthesis versus full-field digital mammography: high-resolution X-ray imaging observer study. Radiology. 2012;262:788–96.
Skaane P, Bandos AI, Gullien R, Eben EB, Ekseth U, Haakenaasen U, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267:47–56.
Haas BM, Kalra V, Geisel J, Raghu M, Durand M, Philpotts LE. Comparison of tomosynthesis plus digital mammography and digital mammography alone for breast cancer screening. Radiology. 2013;269:694–700.
Rose SL, Tidwell AL, Bujnoch LJ, Kushwaha AC, Nordmann AS, Sexton R Jr. Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol. 2013;200:1401–8.
Rafferty EA, Park JM, Philpotts LE, Poplack SP, Sumkin JH, Halpern EF, et al. Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology. 2013;266:104–13.
Svahn TM, Chakraborty DP, Ikeda D, Zackrisson S, Do Y, Mattsson S, et al. Breast tomosynthesis and digital mammography: a comparison of diagnostic accuracy. Br J Radiol. 2012;85:e1074–82.
Mun HS, Kim HH, Shin HJ, Cha JH, Ruppel PL, Oh HY, et al. Assessment of extent of breast cancer: comparison between digital breast tomosynthesis and full-field digital mammography. Clin Radiol. 2013;68:1254–9.
Gennaro G, Hendrick RE, Ruppel P, Chersevani R, di Maggio C, La Grassa M, et al. Performance comparison of single-view digital breast tomosynthesis plus single-view digital mammography with two-view digital mammography. Eur Radiol. 2013;23:664–72.
US Food and Drug Administration. Radiation-emitting products: Mammography quality standards act regulations. http://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/Regulations/default.htm. Accessed 2 Jul 2013.
American college of radiology. ACR BI-RADS® Mammography. ACR BI-RADS atlas, breast imaging reporting and data system. 5th. Reston, VA: American college of radiology; 2013.
Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33:613–9.
Seigel DG, Podgor MJ, Remaley NA. Acceptable values of kappa for comparison of two groups. Am J Epidemiol. 1992;135:571–8.
Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30.
Feng SS, Sechopoulos I. Clinical digital breast tomosynthesis system: dosimetric characterization. Radiology. 2012;263:35–42.
Baker JA, Lo JY. Breast tomosynthesis: state-of-the-art and review of the literature. Acad Radiol. 2011;18:1298–310.
Skaane P, Bandos AI, Eben EB, Jebsen IN, Krager M, Haakenaasen U, et al. Two-view digital breast tomosynthesis screening with synthetically reconstructed projection images: comparison with digital breast tomosynthesis with full-field digital mammographic images. Radiology. 2014;271:655–63.
Zuley ML, Guo B, Catullo VJ, Chough DM, Kelly AE, Lu AH, et al. Comparison of two-dimensional synthesized mammograms versus original digital mammograms alone and in combination with tomosynthesis images. Radiology. 2014;271:664–71.
Acknowledgments
We would like to acknowledge the financial support from the R&D Convergence Program of NST (National Research Council of Science and Technology) of Republic of Korea (Grant CAP-13-3-KERI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
About this article
Cite this article
Choi, W.J., Kim, H.H., Lee, S.Y. et al. A comparison between digital breast tomosynthesis and full-field digital mammography for the detection of breast cancers. Breast Cancer 23, 886–892 (2016). https://doi.org/10.1007/s12282-015-0656-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-015-0656-1