Abstract
Purpose of Review
Prior invasive fungal infection (IFI) in children with malignancies was considered a contraindication for hematopoietic stem cell transplant (HSCT). This review summarizes the current evidence in safety of allogeneic HSCT with prior IFI in children.
Recent Findings
In adult population, some studies have shown that pre-transplant IFI should not be considered a contraindication to allogeneic HSCT, but, in the pediatric population, there is limited information about safety of HSCT in children with prior IFI.
Summary
Epidemiological studies in adults with prior IFI show that allogeneic HSCT is safe. There is no sub-analysis in children within these databases. Studies evaluating risk factors for developing IFI in children with allogeneic HSCT have not found that prior IFI is associated with the reactivation of the fungal infection. A proper control of IFI, the correct choice of conditioning regimen, and secondary prophylaxis make allogeneic HSCT feasible in children with prior IFI. There is an urgency of studies in children evaluating other outcomes to establish HSCT safety in children with prior IFI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to the increase in immunosuppressed patients (primary immunodeficiencies, cancer, autoimmune diseases) and the elevation in survival rates for critically ill children, invasive fungal infections (IFI) have increased in recent years [1].
Hematopoietic stem cell transplant (HSCT) is the definitive treatment for patients with primary immunodeficiencies, as well as for some solid and hematological malignancies that do not have adequate response to chemotherapy [2]. Prior to transplantation, conditioning regimens must deplete all the cells of the immune system, leaving the subject at a great risk of opportunistic infections, including viral, bacterial, and fungal infections. On the other hand, it is known that patients who receive an HSCT and had a latent infection can be reactivated. The most frequent example is CMV, where different strategies have been developed to prevent and diagnose a reactivation to start early prophylaxis or treatment [3].
For years, invasive fungal infections were considered a contraindication to HSCT given the fact that they could be reactivated by the immunosuppression caused by HSCT. At the present time, with advances in conditioning regimens, IFI treatment, and primary and secondary prophylaxis, outcomes of prior IFI in HSCT have changed. We aimed to review treatment options and outcomes of HSCT in children with prior IFI.
Invasive Fungal Infection in Children
Invasive fungal infections are a major cause of morbidity and mortality in immunocompromised and critically ill patients, including bone marrow and solid organ transplant recipients, patients with cancer, AIDS, premature infants, elderly, and patients undergoing major surgery [1].
Candida spp. and Aspergillus spp. are the two main IFI agents. In the USA, the annual incidence of invasive candidiasis and invasive aspergillosis is 72–228 and 12–34 infections/million people, respectively [4], Candida spp. being the third cause of hospital acquired bloodstream infections [5]. Candida albicans is the most common species both in the pediatric population and in neonates; however, among Candida non-albicans species, Candida parapsilosis is the most frequently reported (22% in pediatrics and 28% in neonates) [5]. In France, the incidence and mortality of IFI increased by 1.5% and 2.9% per year (p <0.001) over a period of 10 years from 2001 to 2010 [6]. In contrast, in the USA, it is reported that, in the pediatric population, the incidence of invasive candidiasis decreased by 72%, probably secondary to improvements in the prevention of in-hospital infections and the timely initiation of antifungal prophylaxis in the population at risk [7].
The EUROCANDY study group described the epidemiology of candidemia in newborns, children, and adolescents across Europe in a retrospective study from 2005 to 2015; 1395 episodes of candidemia were recorded in 23 centers in 10 countries in northern and southern Europe. A significant difference was reported in the proportion of candidemia caused by C. albicans vs. non-albicans, with a higher percentage of C. albicans infections in northern Europe (58.6% vs. 44%). Likewise, it was observed that the proportion of C. parapsilosis infections was higher in southern Europe (35.7% vs. 16.4%). These differences reveal a possible geographical difference in the niches of Candida sp. [8].
Filamentous fungal infections are most frequently caused by Aspergillus sp., with an incidence of 2.6 to 6.9% (1). In an international prospective study in the pediatric population, it was found that 75% of filamentous fungal infections were caused by Aspergillus sp., 13% mucormycosis, and 17% by other fungi [9].
Regarding the cancer population, the incidence of IFI varies from 3 to 14.4% depending on the chemotherapy regimens, the antifungal prophylaxis used, and the supportive care that can vary between centers, even in the same country [10]. After 1990, when fluconazole prophylaxis started, invasive candidiasis decreased in > 70% of chemotherapy cycles [11, 12]. This decrease was observed by Simms-Waldrip in a retrospective cohort study in pediatric hematopoietic stem cell transplant patients, finding 66% of invasive infections by Candida during the period of 1991–1996, 48% during the period of 1997–2001, and 37% during the period of 2002–2006, when fluconazole prophylaxis became the standard of care in their institution [13].
In the EUROCANDY study group findings, the population belonging to hemato-oncology services, including bone marrow transplant units, was 16.9%. In this article, a higher frequency of Candida non-albicans infections was reported in patients admitted to hemato-oncological services (60.2%) compared to other services [8].
In the hematopoietic stem cell transplant population, the risk varies according to the type of transplant, being lower in autologous transplant patients (1.2–8.7%), while in allogeneic transplant patients, the incidence of IFI varies from 8 to 24% [11, 12, 14].
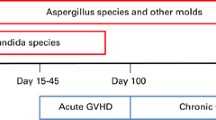
It is important to emphasize that the risk does not only appear during the period of aplasia, as it can occur in a longer period derived from immunosuppression; 89.3% of IFIs appear in the first year after transplantation, most frequently due to Candida sp. and Aspergillus sp. On average, Candida sp. infections occur in the first days after transplantation, while Aspergillus sp. infections occur after 30 days of transplant [13, 15,16,17,18].
The Turkish Pediatric Bone Marrow Transplantation Study Group published the results of a multicenter retrospective study in the pediatric population, estimating a cumulative incidence of probable or proven IFI of 6.5% (95% CI 4.5–9.5%) during the first 180 days after allogeneic transplantation, varying the frequency from 4.5% for the related donor to 10.7% for the unrelated [11]. IFI was diagnosed on average on day +39.5, with lung being the most affected site (46.1%). In Italy, the estimated cumulative incidence of IFI in children with allogeneic transplantation was 4.26% (95% CI 1.99–7.83%) at day 30, 7.45 (95% CI 4.27–11.77) at day 60, 13.29 (95% CI 8.91–18.57) at 120, and 15.96 (95% CI 11.14–21.55) at day 270 [19].
Regarding causal agents, the Turkish group found that the most frequent agents in the pediatric transplant population were Aspergillus 53.8%, Candida 34.6%, Mucorales, and Fusarium 11.6% [11], similar to the Italian group [19] and to that described in adults [15, 20]. Risk factors for IFI in children with HSCT are prolonged neutropenia, receiving high doses of steroids, intense chemotherapy for children with acute myeloid leukemia, and acute and chronic graft-versus-host disease (GVHD) [21].
Outcome of IFI in Children with Hematopoietic Stem Cell Transplantation
The outcome that is generally measured in children with IFI is death rate. Although IFI are rare infections, mortality can reach up to 30% of cases, increasing up to 40% in cases of filamentous fungal infections [11, 13,14,15,16]. Patients with allogeneic HSCT with IFI have a cumulative survival on day +180 lower than those without IFI, 73.1% (95% CI 55.7–90.5) vs. 81.6% (95% CI 77.6–85.6), log rank p = 0.343, respectively [11].
In a study that included 28,542 European subjects with diagnosis of acute leukemia and HSCT, authors reported mortality without relapse to 5 years. Subjects with previous candidemia have mortality of 22.5% (95% CI 17–28) vs. 13.5% (95% CI 13–14) in those without candidemia (p˂0.0001) [14].
In pediatric population with allogeneic HSCT, this phenomenon is not like to adult population; survival rate is lower in subject with IFI (26.9% [95% CI 14.3–50.7] vs. 15.5% [95% CI 12.3–19.6%], p=0.163), but the difference did not reach statistical significance [11]. The analysis of the pediatric patients of the Italian group described as risk factors for mortality, having acute lymphoblastic leukemia, disease not remitted at the time of HSCT, non-myeloablative conditioning regimen, and diagnosis of IFI after day +40 [19].
Changes in the Prophylaxis Regimen to Avoid Invasive Fungal Infection
The risk of IFI is variable and has classically been described in cancer patients, depending on the type of malignancy, type of chemotherapy used, depth and duration of neutropenia, high-dose steroid use, and mucosal damage [22]. In patients receiving HSCT, the risk is based on the type of conditioning regimen, the duration of neutropenia, the presence of GVHD, and the medications used to control GVHD.
Attempts have been made to establish a risk factor model to consider which patients may benefit from the use of antifungal prophylaxis. Usually, an incidence of IFI of greater than 10% is considered as high risk [22]. To establish an institutional prophylaxis policy, local epidemiological data must be considered, and bear in mind that a patient who was not initially considered as high risk can become high risk if, during the post-HSCT follow-up, GVHD is develop and presents a poor response to steroid treatment. An IFI risk classification of HSCT receptors is propose in Table 1.
Prophylaxis Indications
Most groups recommend using antifungal prophylaxis when the incidence of IFI is greater than 10% [22, 23]. Table 2 summarizes the main indications for prophylaxis in HSCT recipients. It is important to consider what is the etiology that is required to prevent; the main objective of prophylaxis could be to avoid Candida spp. infections, which mainly occur in the pre-engraftment period (during neutropenia period), generally associated to the presence of central catheters and mucosal damage secondary to myeloablative conditioning therapy and radiotherapy, or to prevent infections by Aspergillus spp. or other filamentous fungi that appear when patients with HSCT receive greater and more prolonged immunosuppression, generally secondary to treatment of GVHD. Additionally, local epidemiological data on the prevalence of IFI and isolates identified must be considered before choosing prophylaxis, so that the choice of antifungal is adequately supported.
Antifungal prophylaxis in allogeneic HSCT during the period of neutropenia is routinely recommended; this can be performed with various antifungals: fluconazole (IA), itraconazole or voriconazole (BI), micafungin (CI), and liposomal amphotericin B (C-III) [22]. In HSCT, fluconazole demonstrated its efficacy against placebo in 2 trials carried out more than 20 years ago [24, 25], establishing the indication of prophylaxis in HSCT and ushering in a new era in the prevention of IFI. Due to the extensive experience in pediatrics regarding the safety of fluconazole, this drug continues to be the most widely used for prophylaxis in allogeneic HSCT in the pre-engraftment period.
Currently, due to fluconazole prophylaxis, the main infection-causing fungus in pediatric patients with HSCT is Aspergillus spp. [15, 20, 26], displacing Candida spp. to second place. In addition, an increase in the incidence of other filamentous fungi such as Mucorales, Fusarium spp., and Scedosporium spp. has been reported [11].
After engraftment, the risk of aspergillosis is much higher; this increase in filamentous fungi has arisen as a consequence of the severe immunosuppression received by patients with allogeneic HSCT who develop GVHD that require intensive and prolonged immunosuppression treatment (e,g., prednisone at doses greater than 0.3mg/kg/day or the use of anti-inflammatory antibodies) [19]. Under these conditions, antifungal prophylaxis with coverage against filamentous fungi is indicated. Suggested options are posaconazole in children > 13 years old (B-I), voriconazole in children > 2 years old (B-I), and itraconazole (C-II). Other options could include liposomal amphotericin B and micafungin (no degree of evidence) [22].
In a double-blind clinical trial in patients with HSCT and severe GVHD requiring high doses of steroids, the efficacy of posaconazole against fluconazole in decreasing IFI was compared. Posaconazole prophylaxis was associated with a lower incidence of proven and probable IFI (OR 0.56, 95% CI 0.30–1.07, p=0.07) and a significant reduction in proven and probable aspergillosis (OR 0.31, 95% CI 0.13–0.75, p=0.006). A lower incidence in the development of breakthrough invasive fungal infections was also observed in this study (2.4% vs. 7.6%, p=0.004), notably invasive aspergillosis (1.0% vs. 5.9%, p=0.046) [27].
There is published experience on the prophylaxis of IFI in HSCT with micafungin and caspofungin; both require intravenous administration, which limits their use in outpatients. Micafungin is indicated for antifungal prophylaxis in HSCT after a multicenter, randomized trial in which greater overall efficacy of micafungin (80% vs. 73.5%, p = 0.03) was demonstrated compared to fluconazole, to decrease the incidence of IFI during the neutropenic phase (pre-engraftment period) of HSCT [28]. Nevertheless, the representation of the pediatric population in this study (<16 years of age) was small, just 9.5% (84) of the 882 randomized subjects.
In 2007, a meta-analysis of adult patients with cancer and myelosuppressive chemotherapy and HSCT was reported to compare the efficacy of antifungal prophylaxis (fluconazole, itraconazole, posaconazole) with a control group (placebo or without intervention, or with a non-systemic antifungal such as clotrimazole). It was observed that in patients with allogeneic HSCT and antifungal prophylaxis, the incidence of documented IFI could be reduced (RR 0.33, 95% CI 0.18–0.63, p<0.05), as well as all-cause mortality (RR 0.62, 95% CI 0.45–0.85, p<0.05) and mortality related to fungal infection (RR 0.52, 95% CI 0.27–0.99, p<0.05). In autologous HSCT patients, patients who received low-dose amphotericin B (0.2 mg/kg once daily) had an estimated effect similar to that of allogeneic HSCT, but because of few studies, it failed to observe statistical significance [29].
Subsequently, in 2012 another meta-analysis in HSCT and hematological malignancies compared antifungal prophylaxis with an agent with activity against filamentous fungi against prophylaxis with fluconazole. It was observed that prophylaxis with activity against filamentous fungi reduced the number of proven and probable IFI (RR 0.71, 95% CI 0.52–0.98, p=0.03), the risk of invasive aspergillosis (RR 0.53, 95% CI 0.37–0.75, p=0.0004), and the risk of mortality secondary to IFI (RR 0.67, 95% CI 0.47–0.96, p=0.03), but not all-cause mortality (RR 1.0, 95% CI 0.88–1.33, p=0.96). In this study, no specific conclusions could be drawn in pediatric patients since only 1 study included children [30].
When deciding to start prophylaxis with an azole, it must be considered that this group of antifungals is metabolized by the cytochrome P450 system (CYP450) and there is a potential interaction with other drugs metabolized by the same system. The potential for interaction with other drugs is greater with itraconazole and voriconazole than with posaconazole and to a lesser extent with fluconazole.
If posaconazole prophylaxis is started, it should be kept in mind that there are two presentations for oral administration: suspension and delayed-release tablets. The suspension has limited bioavailability, which has been improved with the delayed-release tablets, including patients with HSCT> 13 years of age. Posaconazole tablets have a predictable absorption that improves blood levels [31]; this makes the weight dose of posaconazole in the suspension presentation different from the dose of the delayed-release tablets, and therefore, they are not interchangeable.
Allogenic Hematopoietic Stem Cells Transplantation and Invasive Fungal Infection
Allogeneic HSCT has very precise indications as curative therapy in malignant diseases and has recently been used for curative treatment of primary immunodeficiencies and metabolic diseases [2].
One of the greatest challenges is patients who develop IFI prior to transplantation due to the limited experience to manage this condition in pediatric patients. Various factors must be considered, especially in the case of allogeneic HSCT with prior IFI because they generally received immunosuppression therapy to prevent or to treat graft versus host disease and it potentially could increases the risk of reactivate a latent fungal infection.
The conditioning regimen administrated before the hematopoietic cell infusion is an essential component of HSCT. It is a protocol for applying chemotherapy and/or radiotherapy (even monoclonal antibodies can also be applied), to achieve three goals: (1) create a space in the bone marrow for the graft; (2) create immunosuppression to prevent graft rejection; and (3) eliminate residual tumor.
The conditioning regimens for hematopoietic cell transplantation are classified into myeloablative, nonmyeloablative, and reduced intensity [32].
Myeloablative conditioning (MAC): Medullary hematopoiesis is eradicated and induces deep pancytopenia 1 to 3 weeks after application [32].
Non-myeloablative conditioning (NMA): This regimen seeks to reduce myelosuppressive toxicity, both in deep pancytopenia and in its duration if it occurs [32].
Reduced intensity conditioning (RIC): Conditioning regimen that is not classified as MAC or NMA. RIC regimens result in almost entirely reversible myelosuppression [32].
The drug combinations used in this type of conditioning are summarized in Table 3 [32].
After a related, compatible allogeneic HSCT and without any other factor that delays immune reconstitution, it is known that it can take months or years after transplantation for the recovery of B and T lymphocytes. It is important to remember that both neutrophils and T cells are important for the control of IFIs. The association between T lymphocytes and neutrophils is essential to avoid or to maintain control of IFIs after transplantation. As the immune reconstitution is variable in each patient, it is important to periodically evaluate the lymphocytes populations in order to consider what patient can be candidate for antifungal prophylaxis [33].
Generally, the reconstitution of NK cells and T lymphocytes begins around day +28, the NKs reach their normality around day +100, while may take about a year for T cells to normalize. B cells begin their reconstitution towards day +100 and become normalized around day +180. The source of the hematopoietic progenitor cells impacts the speed of the engraftment (umbilical cord cells take up to 1 month, whereas those of bone marrow take up to 21 days); however, it does not appear to impact restoration of NK cells and T lymphocytes [33].
Among IFI that may be perceived as contraindications for allogeneic HSCT because of the potential high risk of recurrent IFI and transplant-related mortality (TRM), invasive aspergillosis (IA) can have an impact on the incidence and severity of GVHD and on relapse rates of leukemia. A common strategy to avoid this is to reduce pharmacological immunosuppression (e.g., with calcineurin inhibitors), in patients with IA early after HSCT [34].
In a retrospective study of HSCT subjects with prior history of IA, a lower overall survival (56% versus 77%; p = .0001) and higher TRM (38% versus 21%; p = <.001) 100 days after HSCT was associated with prior IA. They also observed that subjects with prior IA who received total body irradiation had higher TRM compared with those subjects who received nonmyeloablative and non-total body irradiation-based regimens (p = 0.024). Finally, in subjects who received less than 1 month of antifungal therapy before HSCT, they observed a major occurrence of post-HSCT invasive aspergillosis [34].
The potential risk of recurrence of an IFI may raise the consideration that allogeneic HSCT is contraindicated. The use of nonmyeloablative regimens (2 Gy of total body irradiation alone) or reduce-intensity conditioning regimens (fludarabine, busulfan, and antithymocyte globulin; melphalan), surgical resection of lung lesions prior HSCT, aggressive antifungal prophylaxis after transplantation, and prophylactic use of granulocyte transfusions have been propose as strategies to reduce the incidence of IA after HSCT [34].
Changes in Opinion About Allogeneic Transplantation in Children with Previous IFI
Several years, it was considered that previous IFI contraindicated a HSCT; however, given the advances in IFI treatment and prophylaxis in the last 15 years, the impact of a prior IFI on HSCT began to be evaluated. The first study was carried out by Vaidya et al. [35] who carried out an evaluation of the impact of IFI by microorganisms other than Candida spp. in all subjects who underwent HSCT in a center in Spain and another in the UK [36] between 1989 and 2001. Twenty-seven subjects were reported with IFI before transplantation, only 3 ˂18 years old; all subjects received some type of secondary prophylaxis (amphotericin b, fluconazole, itraconazole, voriconazole), three (11%) patients had IFI reactivation, all by Aspergillus spp., and one had co-infection with Scedosporium prolificans. For this historical moment, IFI rate was like that reported with patients without prior IFI.
Later El-Cheikh et al. [36] retrospectively evaluated the impact of prior IA on allogeneic transplantation using a reduced intensity conditioning regimen. All IA cases between 2000 and 2008 in France were retrospectively evaluated. The prior IA group received secondary prophylaxis with an anti-mold drug (mostly voriconazole, liposomal amphotericin B, itraconazole, and posaconazole). In patients without prior IA, fluconazole was routinely used as primary prophylaxis. Among 360 subjects who received allogeneic HSCT, 28 subjects with prior IA were identified, proven IA was diagnosed in 3 patients (11%), probable IA in 13 patients (46%), and possible IA in 12 patients (43%). All patients received a fludarabine-based conditioning regimen, and 20 patients received anti-thymocyte globulin. At the time of conditioning, IA was in complete remission in 17 patients (60%), stable or partial remission in 10 (35%), and was refractory in 1 patient. In the post-transplant period, only three patients (11%) had reactivation of the disease, one of them was the patient who had been refractory at the time of the conditioning regimen, another had remission but did not receive appropriate secondary prophylaxis, and only one had been in complete remission at the time of conditioning and received appropriate secondary prophylaxis with voriconazole. Overall survival at 24 months was 64%. This study and the one published by Vaidya et al. [35] were the first two which shown low risk of post-HSCT reactivation of a previous IFI, since previously IFI reactivation rates were reported between 22 and 33%. The authors considered that prior history of IA was not a contraindication if the infection has been controlled, a reduced intensity conditioning was used, and adequate secondary prophylaxis was given.
This phenomenon was repeated in the study by Penack et al. [37] where they retrospectively evaluated the impact of previous IA on several important outcomes of allogeneic HSCT. This study was a collaboration between Infectious Diseases and Acute Leukemia Working Parties of the European Society for Blood and Marrow Transplantation (EBMT); 1150 subjects with a diagnosis of leukemia and allogeneic HSCT (461 without prior IA and 689 with prior IA) were evaluated from 2005 to 2010. The outcomes of interest were mortality, non-relapse mortality, GVHD, and chronic GVHD. Children and adults were included, but there was no sub-analysis for children. The group with previous IA received more frequently a reduced intensity conditioning (40.3% vs. 32.8%). There were no differences in any of the outcomes measured; the authors considered that history of IA generally should not be a contraindication for performing allogeneic HSCT.
One of the most recent studies seeking to answer the question regarding this review is that of Maziarz et al. [38] where they retrospectively studied 11,072 subjects who received a HSCT, from 1995 to 2009, 825 of them with previous IFI (176 under 20 years old), and 10,247 without previous IFI (2,352 under 20 years old). Subjects with IFI had more frequently AML and received a reduced intensity conditioning regimen and antifungal prophylaxis with anti-mold activity. In the analysis, the group with prior IFI had a higher probability of unrelated mortality, global mortality, and relapse; the risk of acute GVHD was not modified, and the probability of chronic GVHD decreased. However, when subjects who received allogeneic HSCT and myeloablative conditioning with history of prior IFI were divided by time periods according to the type of prophylaxis used (1995–2000 without anti-mold prophylaxis and 2001–2009 with anti-mold prophylaxis), a lower probability of unrelated mortality, global mortality, relapse, and IFI was observed in the first year after HSCT in the group with anti-mold prophylaxis. Non-relapse mortality was associated with more advanced disease. This study highlights the advances in the past decade for treatment and prophylaxis of IFI; nowadays, drugs are more effective against resistant molds and yeast, so allogeneic HSCT can be considered in subjects with prior IFI, trying to achieve balance between IFI treatment and prophylaxis, an HSCT in a not so advanced stage of the neoplastic disease, the conditioning regimen, and the GVHD prophylaxis.
Although a sub-analysis in children has not been performed, there are evaluations of risk factors for IFI in children with HSCT. Hol et al. [39] retrospectively evaluated 209 children with allogeneic HSCT to identify predictors of post-HSCT IFI. In the univariate analysis, the scale of risk of treatment-related mortality ˃20%, age 10 years, and history of prior IFI were identified as possible predictors; however, in the multivariate analysis, only the scale of risk of treatment-related mortality ˃ 20% was identified as a predictor for the development of post-HSCT IFI.
In Italy, Castagnola [19] carried out a similar study to evaluate the predictors of IFI and death in children with allogeneic HSCT. Pre-HSCT IFI did not influence the development of previous IFI or mortality. Predictors for IFI were unrelated donor HSCT HR 2.6 (95% CI 1.1–5.9), graft-versus-host disease HR 7.1 (95% CI 2.3–22.2), and CMV infection/reactivation HR 2.3 (95% CI 1.1–5.1).
Conclusions
During the last 2 decades, there have been important advances in antifungal treatment and prophylaxis for IFI, which has allowed to improve the outcomes of allogeneic HSCT. Although there are no formal analyses to assess the safety of allogeneic HSCT in children with prior IFI, indirect analyses of risk factors for IFI suggest that performing an allogeneic HSCT in children with prior IFI may be a feasible alternative, as long as there is a multi-disciplinary approach among the infectious diseases preventionist team and the stem cell transplant team. When an allogeneic HSCT is going to be performed in a child with prior IFI, it is essential to seek the best balance between IFI treatment and prophylaxis and choose the best conditioning regimen as well as prophylaxis for GVHD. It is important that the international community attending patients receiving HSCT formally evaluate the pediatric population to establish outcomes in children with prior IFI.
References
Nucci M, Queiroz-Telles F, Tobón AM, Restrepo A, Colombo AL. Epidemiology of opportunistic fungal infections in Latin America. Clin Infect Dis. 2010;51:561–70. https://doi.org/10.1086/655683.
Kanate AS, Majhail NS, Savani BN, Bredeson C, Champlin RE, Crawford S, et al. Indications for hematopoietic cell transplantation and immune effector cell therapy: guidelines from the American Society for Transplantation and Cellular Therapy. Biol Blood Marrow Transplant. 2020;26:1247–56. https://doi.org/10.1016/j.bbmt.2020.03.002.
al Yazidi LS, Mitchell R, Palasanthiran P, et al. Management and prevention of cytomegalovirus infection in paediatric hematopoietic stem cell transplant (HSCT) recipients: a binational survey. Pediatr Transplant. 2019;23. https://doi.org/10.1111/petr.13458
Richardson M, Lass-Flörl C. Changing epidemiology of systemic fungal infections. Clin Microbiol Infect. 2008;14:5–24. https://doi.org/10.1111/j.1469-0691.2008.01978.x.
Steinbach WJ, Roilides E, Berman D, Hoffman JA, Groll AH, Bin-Hussain I, et al. Results from a prospective, international, epidemiologic study of invasive candidiasis in children and neonates. Pediatr Infect Dis J. 2012;31:1252–7. https://doi.org/10.1097/INF.0b013e3182737427.
Bitar D, Lortholary O, le Strat Y, Nicolau J, Coignard B, Tattevin P, et al. Population-based analysis of invasive fungal infections, France, 2001–2010. Emerg Infect Dis. 2014;20:1163–9. https://doi.org/10.3201/eid2007.140087.
Fisher BT, Ross RK, Localio AR, Prasad PA, Zaoutis TE. Decreasing rates of invasive candidiasis in pediatric hospitals across the United States. Clin Infect Dis. 2014;58:74–7. https://doi.org/10.1093/cid/cit679.
Warris A, Pana Z-D, Oletto A, Lundin R, Castagnola E, Lehrnbecher T, et al. Etiology and outcome of candidemia in neonates and children in Europe. Pediatr Infect Dis J. 2020;39:114–20. https://doi.org/10.1097/INF.0000000000002530.
Wattier RL, Dvorak CC, Hoffman JA, Brozovich AA, Bin-Hussain I, Groll AH, et al. A prospective, international cohort study of invasive mold infections in children. J Pediatr Infect Dis Soc. 2015;4:313–22. https://doi.org/10.1093/jpids/piu074.
Pana ZD, Roilides E, Warris A, Groll AH, Zaoutis T. Epidemiology of invasive fungal disease in children. J Pediatr Infect Dis Soc. 2017;6:S3–S11. https://doi.org/10.1093/jpids/pix046.
Hazar V, Karasu GT, Uygun V, Öztürk G, Kılıç SÇ, Küpesiz A, et al. Risks and outcomes of invasive fungal infections in pediatric allogeneic hematopoietic stem cell transplant recipients receiving fluconazole prophylaxis: a multicenter cohort study by the Turkish Pediatric Bone Marrow Transplantation Study Group. Med Mycol. 2019;57:161–70. https://doi.org/10.1093/mmy/myy015.
Linke C, Tragiannidis A, Ahlmann M, Fröhlich B, Wältermann M, Burkhardt B, et al. Epidemiology and management burden of invasive fungal infections after autologous hematopoietic stem cell transplantation: 10-year experience at a European Pediatric Cancer Center. Mycoses. 2019;62:954–60. https://doi.org/10.1111/myc.12968.
Simms-Waldrip T, Rosen G, Nielsen-Saines K, Ikeda A, Brown B, Moore T. Invasive fungal infections in pediatric hematopoietic stem cell transplant patients. Infect Dis Ther. 2015;47:218–24. https://doi.org/10.3109/00365548.2014.985709.
Cesaro S, Tridello G, Blijlevens N, Ljungman P, Craddock C, Michallet M, et al. Incidence, risk factors, and long-term outcome of acute leukemia patients with early candidemia after allogeneic stem cell transplantation: a study by the Acute Leukemia and Infectious Diseases Working Parties of European Society for Blood and Marrow Transplantation. Clin Infect Dis. 2018;67:564–72. https://doi.org/10.1093/cid/ciy150.
Harrison N, Mitterbauer M, Tobudic S, Kalhs P, Rabitsch W, Greinix H, et al. Incidence and characteristics of invasive fungal diseases in allogeneic hematopoietic stem cell transplant recipients: a retrospective cohort study. BMC Infect Dis. 2015;15:584. https://doi.org/10.1186/s12879-015-1329-6.
Fracchiolla NS, Sciumè M, Orofino N, Guidotti F, Grancini A, Cavalca F, et al. Epidemiology and treatment approaches in management of invasive fungal infections in hematological malignancies: Results from a single-centre study. PLoS One. 2019;14:e0216715. https://doi.org/10.1371/journal.pone.0216715.
Hale KA, Shaw PJ, Dalla-Pozza L, MacIntyre CR, Isaacs D, Sorrell TC. Epidemiology of paediatric invasive fungal infections and a case-control study of risk factors in acute leukaemia or post stem cell transplant. Br J Haematol. 2010;149:263–72. https://doi.org/10.1111/j.1365-2141.2009.08072.x.
Dvorak CC, Steinbach WJ, Brown JMY, Agarwal R. Risks and outcomes of invasive fungal infections in pediatric patients undergoing allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2005;36:621–9. https://doi.org/10.1038/sj.bmt.1705113.
Castagnola E, Bagnasco F, Menoni S, Muraca M, Prete A, Belotti T, et al. Risk factors associated with development and mortality by invasive fungal diseases in pediatric allogeneic stem cell transplantation. A pediatric subgroup analysis of data from a prospective study of the Gruppo Italiano Trapianto di Midollo Osseo (GITMO). Bone Marrow Transplant. 2018;53:1193–7. https://doi.org/10.1038/s41409-018-0160-2.
Montesinos P, Rodríguez-Veiga R, Boluda B, Martínez-Cuadrón D, Cano I, Lancharro A, et al. Incidence and risk factors of post-engraftment invasive fungal disease in adult allogeneic hematopoietic stem cell transplant recipients receiving oral azoles prophylaxis. Bone Marrow Transplant. 2015;50:1465–72. https://doi.org/10.1038/bmt.2015.181.
Fisher BT, Robinson PD, Lehrnbecher T, Steinbach WJ, Zaoutis TE, Phillips B, et al. Risk Factors for invasive fungal disease in pediatric cancer and hematopoietic stem cell transplantation: a systematic review. J Pediatr Infect Dis Soc. 2018;7:191–8. https://doi.org/10.1093/jpids/pix030.
Groll AH, Castagnola E, Cesaro S, Dalle JH, Engelhard D, Hope W, et al. Fourth European Conference on Infections in Leukaemia (ECIL-4): guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or allogeneic haemopoietic stem-cell transplantation. Lancet Oncol. 2014;15:e327–40. https://doi.org/10.1016/S1470-2045(14)70017-8.
Hope WW, Castagnola E, Groll AH, Roilides E, Akova M, Arendrup MC, et al. ESCMID European Society for Clinical Microbiology and Infectious Diseases. Guideline for the diagnosis and management of Candida diseases 2012: prevention and management of invasive infections in neonates and children caused by Candida spp. Clin Microbiol Infect. 2012;18:38–52. https://doi.org/10.1111/1469-0691.12040.
Goodman JL, Winston DJ, Greenfield RA, Chandrasekar PH, Fox B, Kaizer H, et al. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med. 1992;326:845–51. https://doi.org/10.1056/NEJM199203263261301.
Slavin MA, Osborne B, Adams R, Levenstein MJ, Schoch HG, Feldman AR, et al. Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation--a prospective, randomized, double-blind study. J Infect Dis. 1995;171:1545–52. https://doi.org/10.1093/infdis/171.6.1545.
Lehrnbecher T, Schöning S, Poyer F, Georg J, Becker A, Gordon K, et al. Incidence and outcome of invasive fungal diseases in children with hematological malignancies and/or allogeneic hematopoietic stem cell transplantation: results of a prospective multicenter study. Front Microbiol. 2019;10. https://doi.org/10.3389/fmicb.2019.00681.
Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356:335–47. https://doi.org/10.1056/NEJMoa061098.
van Burik J-AH, Ratanatharathorn V, Stepan DE, Miller CB, Lipton JH, Vesole DH, et al. Micafungin versus fluconazole for prophylaxis against invasive fungal infections during neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin Infect Dis. 2004;39:1407–16. https://doi.org/10.1086/422312.
Robenshtok E, Gafter-Gvili A, Goldberg E, Weinberger M, Yeshurun M, Leibovici L, et al. Antifungal prophylaxis in cancer patients after chemotherapy or hematopoietic stem-cell transplantation: systematic review and meta-analysis. J Clin Oncol. 2007;25:5471–89. https://doi.org/10.1200/JCO.2007.12.3851.
Ethier MC, Science M, Beyene J, Briel M, Lehrnbecher T, Sung L. Mould-active compared with fluconazole prophylaxis to prevent invasive fungal diseases in cancer patients receiving chemotherapy or haematopoietic stem-cell transplantation: a systematic review and meta-analysis of randomised controlled trials. Br J Cancer. 2012;106:1626–37. https://doi.org/10.1038/bjc.2012.147.
Cornely OA, Duarte RF, Haider S, Chandrasekar P, Helfgott D, Jiménez JL, et al. Phase 3 pharmacokinetics and safety study of a posaconazole tablet formulation in patients at risk for invasive fungal disease. J Antimicrob Chemother. 2016;71:1747. https://doi.org/10.1093/jac/dkw079.
Brown V (2018) Preparing the patient for HSCT: Conditioning regimens and their scientific rationale. In: Hematopoietic Stem Cell Transplantation for the Pediatric Hematologist/ Oncologist., 1st Edition. Switzerland: Springer International, pp 139–174
Brown V (2018) Immune reconstitution after hematopoietic stem cell transplantation. In: Hematopoietic Stem Cell Transplantation for the Pediatric Hematologist/ Oncologist., 1st Edition. Switzerland: Springer International, pp 371–383
Fukuda T, Boeckh M, Guthrie KA, Mattson DK, Owens S, Wald A, et al. Invasive aspergillosis before allogeneic hematopoietic stem cell transplantation: 10-year experience at a single transplant center. Biol Blood Marrow Transplant. 2004;10:494–503. https://doi.org/10.1016/j.bbmt.2004.02.006.
Vaidya SJ, Ortín M, López-Duarte M, Sirohi B, Powles R, Treleaven J, et al. Haemopoietic progenitor cell transplantation in patients with previous history of invasive fungal infection. Leuk Lymphoma. 2005;46:1143–50. https://doi.org/10.1080/10428190500097052.
El-Cheikh J, Castagna L, Wang L, et al. Impact of prior invasive aspergillosis on outcome in patients receiving reduced-intensity conditioning allogeneic hematopoietic stem cell transplant. Leuk Lymphoma. 2010;51:1–6. https://doi.org/10.3109/10428194.2010.500433.
Penack O, Tridello G, Hoek J, Socié G, Blaise D, Passweg J, et al. Influence of pre-existing invasive aspergillosis on allo-HSCT outcome: a retrospective EBMT analysis by the Infectious Diseases and Acute Leukemia Working Parties. Bone Marrow Transplant. 2016;51:418–23. https://doi.org/10.1038/bmt.2015.237.
Maziarz RT, Brazauskas R, Chen M, McLeod AA, Martino R, Wingard JR, et al. Pre-existing invasive fungal infection is not a contraindication for allogeneic HSCT for patients with hematologic malignancies: a CIBMTR study. Bone Marrow Transplant. 2017;52:270–8. https://doi.org/10.1038/bmt.2016.259.
Hol JA, Wolfs TFW, Bierings MB, Lindemans CA, Versluys ABJ, Wildt de A, et al. Predictors of invasive fungal infection in pediatric allogeneic hematopoietic SCT recipients. Bone Marrow Transplant. 2014;49:95–101. https://doi.org/10.1038/bmt.2013.136.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Martha Aviles-Robles reports personal fees from Merk Sharp & Dohme outside the submitted work. Jose Felix Gaytan Morales, Karla Ojeda-Diezbarroso, Ivan Castorena Villa, and Rodolfo Norberto Jimenez-Juarez declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Infections
Rights and permissions
About this article
Cite this article
Avilés-Robles, M., Gaytan, F., Ojeda-Diesbarroso, K. et al. Allogeneic Hematopoietic Stem Cell Transplant in a Pediatric Patient with Invasive Fungal Infections: Challenges and Indications. Curr Fungal Infect Rep 15, 8–16 (2021). https://doi.org/10.1007/s12281-021-00411-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-021-00411-z