Abstract
Purpose of Review
This review provides information on the utility of reference antifungal susceptibility testing methods in the clinical setting.
Recent Findings
Clinical and Laboratory Standards Institute (CLSI)/European Committee for Antimicrobial Susceptibility Testing breakpoints (BPs) as predictors of therapy response (reported as either “cured” or “failure”) and epidemiological cutoff endpoints (ECVs/ECOFFS) of mutants (harboring specific resistance mechanisms) have been established.
Summary
Although ECVs are available for other species and agents and for commercial methods, only reference triazole and echinocandin BPs have been established. Therefore, correlations of in vitro/in vivo results in this review were based on BPs or ECVs for Candida spp. and/or Aspergillus fumigatus. We also included CLSI ECVs for the Cryptococcus neoformans complex and tentative values for Candida auris. Overall, BPs/ECVs appear to be useful, but most available data are for correlations between BPs and minimal inhibitory concentrations (MICs) for susceptible isolates. Although ECVs can discriminate between MICs for WT (wild type) and mutants (non-WT), an MIC overlap could be present.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive candidiasis, including candidemia, is mostly caused by Candida albicans, C. glabrata, C. parapsilosis, C. tropicalis, and C. krusei and the most common severe mold infections by Aspergillus fumigatus, A. flavus, A. niger, and A. terreus. Candida and Aspergillus infections are seen worldwide among immunocompromised as well as non-immunocompromised patients [1•, 2, 3•, 4]. Irrespective of the species, these infections are associated with high mortality and morbidity rates [1•, 2, 3•, 4]. The overall mortality among patients with invasive candidiasis could be ~ 32% and the rate of treatment success ~ 67.4% (including treatment with licensed agents up to 2012) [5]. However, the mortality rates could be higher among neutropenic patients or patients infected with non-Candida albicans infections such as C. krusei and the emerging C. auris [6]. A similar mortality rate has been reported for Aspergillus infections (47%) that is dependent on both the patient population and age [1•, 2, 3•, 4]. Several antifungal agents have been licensed for the systemic treatment of invasive fungal infections caused by Candida, Cryptococcus, and/or Aspergillus (amphotericin B formulations, flucytosine, triazoles, including isavuconazole, and three echinocandins) and others are under investigation [7••, 8••, 9].
The overall utility of antimicrobial susceptibility testing is to aid in selecting the most effective agent for the treatment of microbial infections, which is best achieved by species-specific categorical/interpretive end points, breakpoints (BPs), or epidemiological cutoff values (ECVs). Although both standard and commercial antifungal susceptibility testing methods are available for evaluating the infecting isolates, BPs are only established for a few fungal species and agent combinations. More recently and based solely on MIC (minimal inhibitory concentration) or MEC (minimal effective concentration) distributions, method-specific ECVs or ECOFFs were defined for a variety of yeast and mold species for reference and commercial methods. However, very little information is found in the literature regarding specific correlations of clinical outcome and antifungal susceptibility testing results using BPs or ECVs. One of the reasons is that the infecting agent is not always available due to the lack of reliable methods for the diagnosis of invasive fungal infections. Blood cultures are unreliable markers of candidemia, and in the case of aspergillosis, the Aspergillus PCR assay is substantially more sensitive (77–84%) than blood and respiratory fluids cultures [8••].
Earlier reviews focused on the different available methodologies for antifungal susceptibility testing as well as the expected in vitro results for a variety of fungal species. We present the correlations of MICs with either the clinical outcome to therapy or the presence of genetic resistance mechanisms in the infecting isolate. The literature was first searched for (i) the value of established reference triazole or echinocandin BPs as predictors of clinical response to therapy (reported as either “cured” or “failure”) and (ii) the value of reference ECVs as predictors of mutant isolates when specific resistant mechanism among Candida or Aspergillus isolates were present. Given that ECVs for the Cryptococcus neoformans complex as well as tentative values for C. auris were recently published, those combinations were also included.
Reference Antifungal Susceptibility Methods and Categorical/Interpretive End points
CLSI
The Clinical and Laboratory Standards Institute (CLSI) has developed broth microdilution susceptibility testing methods for Candida spp., the C. neoformans complex, and molds (M27-4th ed. and M38-3rd ed.) documents, respectively) [10, 11]. CLSI BPs were established for most common Candida spp. for MIC categorization of triazoles and echinocandins taking into account (i) the MIC, (ii) resistance mechanisms, (iii) PK/PD (pharmacokinetic/pharmacodynamic) information, and (iv) patient response to therapy from clinical trials (Tables 1 and 4) [12••, 13,14,15,16,17,18,19,20,21]. CLSI method-dependent triazole (isavuconazole included) and echinocandin ECVs also have been defined for species of Candida, Aspergillus, C. neoformans, and other molds [22,23,24,25,26, 27••, 28•, 29], including some species for which BPs have not been established [28•]. The calculation of CLSI ECVs met the criteria postulated by this organization: a minimum of 100 MIC values in the particular pool of data points for ECV definition analysis, modal compatibility among at least three contributing laboratories, and five data points in each distribution/species/agent/laboratory [29]. The ECV calculation should take into account the inherent variability of the test (usually within 1 doubling dilution). The ECVs listed in Table 4 were calculated by the iterative ECOFFinder technique and encompassed 95 to 97.5% of the isolates [30]. Approved CLSI categorical end points are listed in CLSI documents M60 [12••], M59 (approved ECVs) [27••], and elsewhere [28•].
There are some important considerations when using the CLSI M27 method and BPs [12••]. The CLSI BPs for voriconazole and C. krusei are based on the clinical response to voriconazole from 7 of 9 (78%) patients evaluated during voriconazole clinical trials (data not included in Tables 1 and 4). Since C. krusei is innately resistant to fluconazole, testing for this agent/species is not needed. Given that the clinical outcome among patients treated with either fluconazole and especially voriconazole for C. glabrata infections was poor regardless of the MIC endpoint, only the fluconazole susceptible-dose dependent (SDD: ≤ 32 μg/ml) and resistant (≥ 64 μg/ml) endpoints are documented in the CLSI M60 document [12••]. Because of that, this document states that for C. glabrata infections versus fluconazole, higher doses than the standard 6 mg/kg/day may be required for adults.
More importantly, poor interlaboratory agreement of caspofungin MICs for Candida spp. has been reported for both CLSI and European Committee for Antimicrobial Susceptibility Testing (EUCAST) MICs [31]. However, the CLSI M60 lists BPs for caspofungin and Candida spp. with the recommendation that caspofungin “susceptible MICs” should be confirmed with follow-up anidulafungin and micafungin MICs and/or the presence of mutations in the infecting isolate [12••]. Neither step is practical or feasible in most clinical laboratories as well as being time consuming which will further delay the report. The best approach would be to use either anidulafungin or micafungin as surrogate indicators of echinocandin resistance, since CLSI BPs and ECVs are available for Candida spp. and those two agents. Because of that, Table 4 only provides anidulafungin data as the surrogate indicator.
EUCAST
European Committee for Antimicrobial Susceptibility Testing Broth microdilution methods were also developed by the EUCAST for testing Candida and Aspergillus spp. The EUCAST BPs are based on MIC distributions, PK/PD information, correlation and regression trees (CART) analysis, including Monte Carlo simulations, and to a certain extent clinical data (http://www.eucast.org/ast_fungi/) [32,33,34,35]. Although susceptible EUCAST and CLSI fluconazole and voriconazole BPs are the same for C. albicans, C. parapsilosis, and C. tropicalis (fluconazole BPs < 2 μg/ml and voriconazole BPs < 0.12 μg/ml) (Table 1), there are some substantial differences among other CLSI and EUCAST BPs [35]. In addition to the susceptible and resistant breakpoints, an intermediate BP is available for fluconazole (not usually listed). The intermedia EUCAST BP is “the value between the S and R categories” [34]. EUCAST has developed BPs for the triazoles, including isavuconazole and amphotericin B for A. fumigatus and other Aspergillus spp. and several ECOFFs for Candida/Aspergillus spp., including tentative ECVs for C. auris and most available agents [36] (http://www.eucast.org/documents/consultations/). EUCAST guidelines for setting ECVs are in the “EUCAST discussion document” (under review). But it is not clear yet what are the restrictions or criteria regarding the MIC data used to define EUCAST ECVs, but the listed “combined distributions are from multiple sources and time periods” when ECVs/BPs were established for the particular agent. Overall, EUCAST ECOFFs are set “when the visual and statistical ECOFFs are no more than one 2-fold dilution apart” [36] (http://www.eucast.org/documents/consultations/), (www.eucast.org/clinical_breakpoints). Interlaboratory discrepancies were also evident among caspofungin EUCAST MICs for Candida spp. [31]. The recommendation is to use either anidulafungin or micafungin as surrogate data (www.eucast.org/clinical_breakpoints).
Commercial Etest and SYO Methods
Although it is not the scope of the present review to cover the commercial methods, ECVs have been developed for the widely used Sensititre Yeast One (SYO) and Etest methods [37,38,39,40,41, 42••, 43••]. However, the lack of suitable data has precluded the establishment of BPs for the categorical interpretation of MICs by the commercial methods. Presently, these two methods rely on CLSI interpretive categories as well quality control (QC) data. Also, despite favorable comparisons between MICs by commercial and reference methods to evaluate method equivalence before marketing, substantial method-dependent differences were reported between CLSI, SYO, and Etest ECVs [40, 43••]. Therefore, it is not advisable to use reference BPs/ECVs to categorize MICs that are obtained by either of these two methods. Instead, the physician should be apprised regarding the potential role/usefulness of the ECV as a predictor of antifungal resistance [28•,29]. Recent ECV studies have concluded that, although both SYO and Etest methods are easier to perform and more practical than reference methods, due to interlaboratory discrepancies among the participant laboratories, the SYO method provides more reliable data for Candida spp. and the Etest for Aspergillus spp. [42••, 43••].
Resistance Mechanisms in Fungal Isolates
The impact of azole and echinocandin resistance in MIC data is widely recognized, and various mutational mechanisms of resistance have been elucidated, especially for the most prevalent Candida spp. and A. fumigatus [15, 17, 22, 23, 42••, 43••, 44••, 45,46,47, 48••, 49,50,51,52,53]. The use of triazole therapies has led to in vitro resistance among Candida and other yeasts to fluconazole, voriconazole and posaconazole [15, 17, 22, 44••, 45,46,47, 48••]. The azoles block the pathway of ergosterol biosynthesis by inhibiting the 14-α-lanosterol demethylase enzyme. Various molecular mechanisms are associated with in vitro resistance to the triazoles and Candida spp., such as modifications in the quality or quantity of the target enzyme (ERG11 gene mutations/modifications and/or overexpression) or the MRR1 transcriptional regulator [15, 17, 44••, 45,46,47, 48••]. Also, the active azole efflux from the fungal cell mediated through the activation of multidrug efflux transporters encoded by CDR1, CDR2, or PDR1 genes has been reported [15, 17, 44••, 45,46,47, 48••]. More recently, resistance to the echinocandins has become prevalent especially among C. glabrata and other Candida isolates [49,50,51,52,53]. Echinocandin resistance among Candida isolates is usually associated with mutations in the 1,3 β-d-glucan synthase target enzyme encoded by either the hot FKS1 (Candida species, including C. glabrata) or FKS2 (C. glabrata) gene muations [49,50,51]. Resistance to the triazoles against Aspergillus spp. also has increased in the last decade, especially in Europe. The most frequent resistance mechanisms in A. fumigatus are the mutations in the Cyp51A gene [28•, 42••]. However, although ECVs have been proposed for other agents, very little data are available regarding the resistance mechanisms for other agents and fungal species [28•].
Role of the Categorical/Interpretive Endpoints
BPs and ECVs
As discussed above, the BP is the predictor of clinical outcome guiding the clinician in choosing the best agent for the infecting isolate being evaluated [12••,15, 17, 21]. The ECV, as the new categorical end point, will differentiate the non-WT (strains potentially harboring resistance mechanisms) from the WT isolates (strains without known resistance mechanisms) in the MIC/MEC distribution [22, 23, 28•, 29]. Because ECVs do not take into account the pharmacology of the antifungal agent or the findings from clinical outcome studies, the ECV will not categorize a fungal isolate as susceptible or resistant as BPs do. The ECV is the highest MIC/MEC without phenotypically expressed resistance and is not a predictor of treatment outcome. Due to all those considerations, the ECV only should be used when BPs have not been established for the species/agent being evaluated; they could provide clinical guidance regarding the potential outcome/response to therapy [28•, 29]. Again, regardless of their role, both categorical end points are species/agent dependent as well as method-dependent. ECVs also are particularly useful in tracking the emergence of resistance at an institution. Finally, both categorical end points only are useful in the clinical setting, when the causative fungal isolate is identified to the species level.
Factors That Obscure In Vitro Versus In Vivo Correlations Using BPs or ECVs
Other factors, beside the MIC for the infecting isolate and therapy with the licensed antifungal agents, can obscure the correlations of in vitro versus in vivo results as follows: (i) the extrapolation of method versus categorical end point, (ii) the PK/PD status, (iii) the host immune status, (iv) the site of infection, and (v) the infecting isolate species [54]. In 2012, based on data from several clinical trials for invasive Candida infections, the following factors were identified as predictors of patient mortality [5]: (i) increasing age, (ii) the Acute Physiology and Chronic Health Evaluations, (iii) the use of immunosuppressive therapy, and (iv) infections caused by C. tropicalis and more recently, among candidemia patients, by the fluconazole resistant C. auris (~ 70% mortality) [6]. However, removal of the central venous catheter and/or treatment with an echinocandin instead of amphotericin B or a triazole has been associated with decreased mortality [5, 55]. Tables 2 and 3 depict the impact of the immune status and/or of the infecting isolate species on the clinical response to therapy during earlier clinical trials [56]. Some echinocandin PK/PD factors are discussed in more detail below.
The echinocandin PD target for 11 C. glabrata mutants (fks mutations, MICs 0.06–4 μg/ml) and 8 WT (MICs 0.03–0.25 μg/ml) was evaluated using an in vivo invasive candidiasis/echinocandin model [57]. The mean free anidulafungin 24-h AUCf/MIC ratio associated with stasis for the WT group was 13.2 and 3.43 for the mutants. In patients, the PD target was achieved when the anidulafungin MICs for the infecting isolates was 0.25 μg/ml (C. glabrata infections). The conclusion was that the MIC could be a better predictor of the outcome of therapy than the identification of genetic mutations [57]. Regarding the PK/PD status in patients treated for invasive candidiasis with micafungin (100 mg daily), there was a relationship between a patient’s weight and drug exposure which indicated that patients weighing > 100 kg could have insufficient drug exposure and thus potentially inadequate antifungal treatment [58•]; the median micafungin MIC for the infecting isolates was 0.016 μg/ml (susceptible). Therefore, it is possible that patients infected with Candida isolates with higher MICs also could have insufficient drug exposure.
In Vitro Versus In Vivo Correlations: the Triazoles Versus Candida spp., C. neoformans VNI, and A. fumigatus
Because reports of response to therapy and their correlation with MICs are scarce, the data from earlier fluconazole and voriconazole and Candida spp. clinical trials are included in Table 4 [15, 17]. However, more data were available regarding the presence of mutations and their effect on the MIC end point. The CLSI triazole MIC data for Candida spp. and A. fumigatus Cyp51A mutants were pooled from the multicenter studies that defined CLSI ECVs and other reports [42••, 44••, 45,46,47, 48••, 59,60,61,62,63,64,65,66]. MIC data for mutants validated ECVs as predictors of triazole resistance [24, 28•, 29].
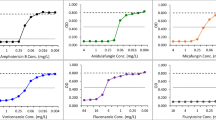
Candida spp. Versus the Triazoles
The clinical response to therapy and the presence of specific mutations for the infecting isolate are depicted in Table 4; the overall clinical response according to CLSI (fluconazole and voriconazole) and EUCAST (fluconazole) BPs C. albicans, by categories are summarized in Table 1. Clinical trials to assess the efficacy of fluconazole and voriconazole prior to licensing yielded very little data for resistant or other non-C. albicans isolates [15, 17, 32]. The most probable reasons were that patients were not infected with non-C. albicans isolates as C. albicans was and continues being the most prevalent species; also, perhaps it was too early for resistance development. The treatment response data for each species and BP was summarized when the current CLSI BPs were proposed (between 2010 and 2011; Table 4) [12••, 15, 17]. The correlation between fluconazole MICs ≤ 2 μg/ml for C. albicans (susceptible BP) and successful clinical response to therapy (patients considered cured) was 94% and 70% for C. tropicalis (smaller number of treated patients with the latter species (20 versus 339) (Table 4). Regarding the fluconazole SDD value for C. glabrata of ≤ 32 μg/ml, 40 of 64 (63%) patients responded to therapy. Correlations between voriconazole MICs and clinical outcome for C. albicans, C. parapsilosis and C. tropicalis were similar (72–82%) [17] (total number of patients infected with each of these three species was below 100) (Table 4). Further information about the role of PK/PD and MICs on the clinical outcome of patients treated with triazoles can be found in a recent review [67].
MICs from multiple laboratories enabled the definition of CLSI triazole ECVs for the five Candida spp. listed in Table 4, as well as for C. guilliermondii, C. lusitaniae, and C. krusei [22, 27••, 28•]. ECVs for those three species were not listed, because genetic information is not available, but those ECVs can be found elsewhere [22, 28•]. The performance of fluconazole and voriconazole ECVs in recognizing Candida spp. mutants was excellent for most of the species/agent combinations listed in Table 4 (92 to 100%) [22, 44••, 45,46,47]. The same applied among the WT isolates evaluated (MICs equal to or below the ECV). Although CLSI has not defined isavuconazole ECVs for Candida spp., the available CLSI data for C. albicans and C. glabrata mutants are listed in Table 4 [44••]. Insufficient data precluded a proper evaluation of posaconazole ECVs for Candida spp. However, with the exception of fluconazole, some “overlap” was observed with the other triazoles. The overlap indicated that MICs for confirmed mutants were below the ECV (false WT) or that MICs for WT isolates (without known mechanism of resistance; false non-WT) were above the ECV. This phenomenon can be observed in most published studies, where data for confirmed mutant and WT isolates have been reported.
Tentative EUCAST/CLSI ECVs for C. auris were defined for various agents [36], including fluconazole and voriconazole; data for 42 mutants and 36 WT isolates were recently reported (most common mutations, EGR11 Y132F and K143R, also found among C. tropicalis and C. parapsilosis mutants) [48••]. CLSI fluconazole MICs for the mutants were 4– > 128 μg/ml (mode, ≥ 16 μg/ml) and for the WT 2–64 μg/ml (mode, 2 μg/ml), so there was an MIC overlap among WT and mutants. Similar overlap was observed with the voriconazole ECV (8 μg/ml; Table 4) as well as discrepant modes for both agents [36, 48••]. Redefinition of these ECVs should be considered to evaluate interlaboratory modal agreement.
C. neoformans VNI Versus Fluconazole
In addition to ECVs for Candida and the triazoles, the CLSI has approved ECVs for various Cryptococcus spp., including C. neoformans VNI, the triazoles, amphotericin B, flucytosine, and isavuconazole [25, 27••, 28•]. The CLSI ECV for C. neoformans VNI and isavuconazole is 8 μg/ml (WT values); isavuconazole MICs of ≤ 8 μg/ml (WT values) for eight isolates were reported from patients treated with this agent for cryptococcal meningitis; six of eight patients had a successful outcome to therapy (Table 4) [68]. It is interesting that fluconazole MICs were 0.25 to 8 μg/ml (presumptively WT isolates) for isolates from patients reported as cured, while five therapeutic failures correlated with MICs of ≥ 16 mg/ml [69] (fluconazole data not listed in Table 4); these latter MICs were obtained using the yeast nitrogen base instead of the CLSI RPMI broth [10].
Aspergillus spp. Versus the Triazoles
The CLSI has not developed BPs for molds due to lack of suitable clinical data, but ECVs have been approved for amphotericin B and the triazoles, including isavuconazole for A. fumigatus and other molds [24, 26, 27••, 28•, 42••]. Table 4 provides a summary of the performance of the available triazole ECVs in identifying potential A. fumigatus non-WT isolates (data pooled from various published studies) [42••, 59,60,61,62,63,64,65,66]. The CLSI itraconazole ECV of 1 μg/ml (97%) is superior to the posaconazole ECV of 0.25 μg/ml (77%) and both voriconazole and isavuconazole ECVs of 1 μg/m (83/84%, respectively) in identifying the Cyp51A mutants. However, certain mutations do not affect posaconazole and voriconazole MICs as they do itraconazole values. It also has been suggested that some mutations must be silent polymorphisms [42••]. A recent clinical report correlated CLSI/EUCAST voriconazole MICs > 8 μg/ml with a patient’s treatment failure to this agent; data for pretreatment isolate(s) was not provided [70].
EUCAST ECVs have been established for Aspergillus spp. and the triazoles. EUCAST posaconazole MICs were pooled for 52 A. fumigatus mutants in a recent collaborative study [42••]; itraconazole and voriconazole data were reported elsewhere [71] (not shown in Table 4). The EUCAST posaconazole ECV of 0.25 μg/ml would have identified as non-WT, 40 of the 52 isolates harboring confirmed mutational changes [42••]. EUCAST triazole ECVs for A. fumigatus were first defined in an earlier study, where 32 A. fumigatus mutants with itraconazole MICs ≥ 8 μg/ml were evaluated [72]. Posaconazole MICs for those mutants were 0.12– > 8 μg/ml, which indicated a similar overlap between MICs for WT and mutant isolates, but not among itraconazole MICs [71, 72]. Similar mutations were observed in both studies (G54, M220 or TR34), but the latter evaluations included TR46 [42••, 71].
However, it was recently reported that there was no relationship between patient outcome to therapy versus isavuconazole and voriconazole MICs for infecting Aspergillus isolates [73]. Their summary was as follows: of 49 patients treated with isavuconazole, 6 patients died (MICs, > 2 μg/ml for 1/6 of the infecting isolates); 43/49 patients responded (alive at the end of therapy) and MICs were ≤ 2 μg/ml for 38/43 (88%) of the infecting isolates (data not listed in Table 4). Although the isavuconazole EUCAST ECV is ≤ 2 μg/ml for A. fumigatus, the proposed BP is ≤ 1 μg/ml [34]. In the case of voriconazole, both EUCAST BP and ECV are ≤ 1 μg/ml for A. fumigatus, so the overlap between “susceptible” and “resistant” MICs was also evident with this agent. ECVs and BPs are species specific [12••, 28•, 29], but the infecting isolates were reported as “Aspergillus,” so the proportion of A. fumigatus in the set is not clear. However, it appears that the isavuconazole EUCAST BP needs to be adjusted for this species, as more data from clinical trials becomes available. It is interesting that based on an in vitro dynamic model of invasive pulmonary aspergillosis with simulation of human-like voriconazole PK and galactomannan as a biomarker, the trough concentration that achieved suppression of galactomannan was the EUCAST voriconazole MIC of 1.68 μg/ml [63]. The authors suggested that for voriconazole and A. fumigatus, the BPs could be ≤ 1 μg/ml and > 2 μg/ml, as susceptible and resistant BPs, respectively.
Candida spp. and the Echinocandins
Elevated echinocandin MICs for Candida spp. have been associated with amino acid substitutions in the FKS1 and FKS2 genes, therapeutic failure, and/or breakthrough infections. However, resistance mechanisms are not as clearly elucidated for Aspergillus spp. There is also the interlaboratory variability issue among reference caspofungin MICs for Candida spp. [31]. Due to those concerns, Table 4 only depicts the correlation of CLSI anidulafungin MICs with treatment outcome from clinical trials and other report [21, 53]. The correlation of CLSI anidulafungin ECVs and MICs for Candida mutants was also provided in Table 4, including the data summarized during the calculation of echinocandin ECVs and from other studies [23, 49,50,51,52,53]. The clinical data for patients treated with micafungin, including data for mutants, is summarized below [52]. Those two echinocandins have been recommended as surrogate agents. Some of these studies were published before ECVs were defined according to the current criteria, so the correlations were based on BPs instead of ECVs for the mutants [51,52,53]. However, those data were re-evaluated according to current CLSI ECVs [23, 27••, 28•].
The correlation of CLSI MICs for C. albicans, C. glabrata, and C. parapsilosis and clinical response to anidulafungin therapy was excellent for the susceptible isolates (91–93%) [21, 53]; lower percentages were observed for the other two species, but the number of patients treated was small (Table 4) [21]. Clinical trials did not include much anidulafungin data for resistant or intermediate isolates; in a recent study, anidulafungin MICs > 0.12 μg/ml for C. glabrata only predicted 5/22 treatment failures [53]. In a micafungin study [52], 6/16 patients responded to therapy (MICs 0.03–1 μg/ml); however, the micafungin MIC range was 0.12 to 4 μg/ml (only two intermediate values, 0.12 μg/ml) for the 10 treatment failure isolates [52]. Results were similar with either agent in both studies. So, more data are needed to clarify these discrepant results.
Concerning the pooled echinocandin data for mutants and ECVs [23], the predictor value of the anidulafungin CLSI ECVs in detecting mutants ranged from 88% (C. glabrata) to > 90% for the other Candida species (Table 4). The amount of data was small for some of these species/anidulafungin combinations.
Using the EUCAST method, MIC data for 20 Candida spp. (8 C. albicans, 2 C. krusei, and 10 C. glabrata) harboring FKS1 or FKS2 mutations indicated that anidulafungin MICs for these three species were above the EUCAST ECVs (0.03 μg/ml, 0.06 μg/ml, and 0.06 μg/ml) [74]. These isolates were recovered from patients with bloodstream infections treated with caspofungin. Echinocandin MICs for the initial isolates were low (WT by FKS sequence), but they increased following therapy [74] (data not shown in Table 4).
IDSA Recommendations for Antifungal Susceptibility Testing
For Candida Infections
Due to recent trends, the IDSA recommends the determination of azoles and echinocandin MICs for: (i) C. glabrata isolates, (ii) isolates from blood/sterile sites, and (iii) isolates recovered from treatment failures, breakthrough infection, or limited therapeutic options (e.g., adverse events, allergies, or previous exposures) [7••].
For Aspergillus Infections
Again, the recommendation is to test Aspergillus isolates from patients failing therapy or for epidemiological purposes [8••]. Ideally, isolates recovered prior to and during therapeutic failure should be tested together.
For Non-Candida and Non-Aspergillus Species
In addition to isolates from sterile/deep sites, the recommendation is to test isolates from patients previously exposed to an antifungal agent, rare/emerging, or species known to be less susceptible to antifungal agents.
Conclusions
Available standardized antifungal susceptibility testing methods are internationally used. CLSI/EUCAST triazole and echinocandin BPs and ECVs/ECOFFS have been established for some Candida spp. and Aspergillus spp. Reference BPs or ECVs could be useful MIC cutoffs as predictors of failure/success to therapy (BPs) or to identify mutant/non-WT isolates (ECVs). However, other factors can influence therapeutic outcome in addition to microbiological clearance, because this relationship is dependent on the combination of the MIC and the factors discussed above. Current knowledge of genetic resistance mechanisms among Candida (triazoles and echinocandins) and Aspergillus spp. (triazoles) is valuable since antifungal resistance continues to spread, including multidrug resistance. However, resistance mechanisms have not been elucidated and BPs are not available for other antifungal agents/species (e.g., less common or emerging species or new agents).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Bongomin F, Gago S, Oladele RO, Denning DW. Global and multinational prevalence of fungal diseases-estimate precision. J Fungi (Basel). 2017;3:E57. https://doi.org/10.3390/jof3040057 A paper interrogating the accuracy of the serious fungal infection burden estimates in 43 papers published within the Leading International Fungal Education (LIFE) initiative.
Bassetti M, Righi E, Montravers P, Cornely OA. What has changed in the treatment of invasive candidiasis? A look at the past 10 years and ahead. J Antimicrob Chemother. 2018;73:i14–25. https://doi.org/10.1093/jac/dkx445.
• Kontoyiannis DP. Antifungal resistance: an emerging reality and a global challenge. J Infect Dis. 2017;216:S431–5. https://doi.org/10.1093/infdis/jix179 An overview on different aspects of a complex area dealing with the emerging and global problem of the antifungal resistance in pathogenic fungi.
Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax. 2015;70:270–7. https://doi.org/10.1136/thoraxjnl-2014-206291.
Andes DR, Safdar N, Baddley JW, Playford G, Reboli AC, Rex JH, et al. Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis. 2012;54:1110–22.
Clancy CJ, Nguyen MH. Emergence of Candida auris: an international call to arms. Clin Infect Dis. 2017;64(2):141–3.
•• Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner, et al. Clinical practice guidelines for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62:1–50. https://doi.org/10.1093/cid/civ747 An advice to physicians for applying the current IDSA guidelines for the management of candidiasis in the light of each patient’s individual circumstances.
•• Patterson TF, Thompson GR III, Denning DW, Fishman JA, Hadley S, Herbrecht R, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;63:e1–e60. https://doi.org/10.1093/cid/ciw326 An advice to physicians for applying the current IDSA guidelines for the management of aspergillosis in the light of each patient’s individual circumstances.
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR Jr, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–322.
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts. In: CLSI standard M27. 4th ed. Wayne: Clinical and Laboratory Standards Institute; 2017.
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. In: CLSI standard M38. 3rd ed. Wayne: Clinical and Laboratory Standards Institute; 2017.
•• Clinical and Laboratory Standards Institute. Performance standards for antifungal susceptibility testing of yeasts. In: CLSI standard M60. 1st. ed. Wayne: Clinical and Laboratory Standards Institute; 2017. An update on the CLSI clinical breakpoints (BPs) and QC data for the broth microdilution reference M27 method.
Rex JH, Bennett JE, Sugar AM, Pappas PG, van der Horst CM, Edwards JE, et al. A randomized trial comparing fluconazole and amphotericin B for the treatment of candidemia in patients without neutropenia. N Engl J Med. 1994;331:1325–30.
Clancy CJ, Yu VL, Morris AJ, Snydman DR, Nguyen MH. Fluconazole MIC and the fluconazole dose/MIC ratio correlate with therapeutic response among patients with candidemia. Antimicrob Agents Chemother. 2005;49:3171–7.
Pfaller MA, Andes D, Diekema DJ, Espinel-Ingroff A, Sheehan D, The CLSI Subcommittee for Antifungal Testing. Wild-type MIC distributions, epidemiological cutoff values and species-specific clinical break-points for fluconazole and Candida: time for harmonization of CLSI and EUCAST broth microdilution methods. Drug Resist Updat. 2010;13:180–95.
Kuhlberg BJ, Sobel JD, Ruhnke M, Pappas PG, Viscoli C, Rex JD, et al. Voriconazole versus a regimen of amphotericin B followed by fluconazole for candidemia in nonneutropenic patients: a randomized non-inferiority trial. Lancet. 2005;366:1435–42.
Pfaller MA, Andes D, Arendrup MC, Diekema DJ, Espinel-Ingroff A, Alexander BD, et al. Clinical breakpoints for voriconazole and Candida spp. revisited: review of microbiologic, molecular, pharmacodynamic, and clinical data as they pertain to the development of species-specific interpretive criteria. Diagn Microbiol Infect Dis. 2011;70:330–43.
Kuse ERP, Chutchotisakd CA, da Cunha RM, Barrios C, Raghunadharao D, Sekhon JS, et al. Micafungin versus liposomal amphotericin B for candidemia and invasive candidiasis: a phase III randomized double-blind trial. Lancet. 2007;369:1519–27.
Pappas PG, Rotstein CMF, Betts RF, Nucci M, Talwar D, De Waele JJ, et al. Micafungin versus caspofungin for treatment of candidemia and other forms of invasive candidiasis. Clin Infect Dis. 2007;45:883–93.
Reboli AC, Rotstein C, Pappas PG, Chapman SW, Kett DH, Kumar D, et al. Anidulafungin versus fluconazole for invasive candidiasis. N Engl J Med. 2007;356:2472–82.
Pfaller MA, Diekema DJ, Andes, D, Arendrup MC, Rodriguez-Tudela J-T, the CLSI Subcommittee for Antifungal Testing. Clinical breakpoints for the echinocandins and Candida revisited: Integration of molecular, clinical, and microbiological data to arrive at species-specific interpretive criteria. Drugs Resist Updates 2011:14:164-176.
Espinel-Ingroff A, Pfaller MA, Bustamante B, Canton E, Fothergill A, Fuller J, et al. Multilaboratory study of epidemiological cutoff values for detection of resistance in eight Candida species to fluconazole, posaconazole, and voriconazole. Antimicrob Agents Chemother. 2014;58:2006–12. https://doi.org/10.1128/AAC.02615-13.
Pfaller MA, Espinel-Ingroff A, Bustamante B, Canton E, Diekema DJ, Fothergill A, et al. Multicenter study of anidulafungin and micafungin MIC distributions and epidemiological cutoff values for eight Candida species and the CLSI M27-A3 broth microdilution method. Antimicrob Agents Chemother. 2014;58:916–22. https://doi.org/10.1128/AAC.02020-13.
Espinel-Ingroff A, Diekema DJ, Fothergill A, Johnson E, Pelaez T, Pfaller MA, et al. Wild-type MIC distributions and epidemiological cutoff values for the triazoles and six Aspergillus spp. for the CLSI broth microdilution method (M38-A2 document). J Clin Microbiol. 2010;48:3251–7. https://doi.org/10.1128/JCM.00536-10.
Espinel-Ingroff A, Chowdhary A, Gonzalez GM, Guinea J, Hagen F, Meis JF, et al. Multicenter study of isavuconazole MIC distributions and epidemiological cutoff values for the Cryptococcus neoformans–Cryptococcus gattii species complex using the microdilution method. Antimicrob Agents Chemother. 2015;59:666–8.
Espinel-Ingroff A, Chowdhary A, Gonzalez GM, Lass-Flörl C, Martin-Mazuelos E, Meis J, et al. Multicenter study of isavuconazole MIC distributions and epidemiological cutoff values for Aspergillus spp. for the CLSI M38-A2 broth microdilution method. Antimicrob Agents Chemother. 2013;57:3823–8.
•• Clinical and Laboratory Standards Institute. Epidemiological cutoff values for antifungal susceptibility testing. In: CLSI supplement M59. 2nd ed. Wayne: Clinical and Laboratory Standards Institute; 2018. An updated document by the CLSI that summarizes the approved epidemiological cutoff values for antifungal susceptibility testing
• Espinel-Ingroff A, Turnidge J. The role of epidemiological cutoff values (ECVs/ECOFFs) in antifungal susceptibility testing and interpretation for uncommon yeasts and moulds. Rev Iberoam Micol. 2016;33:63–75 This review summarizes the ECVs that are not listed in the M59 document, as well as detailed information about ECV calculation.
Clinical and Laboratory Standards Institute. Principles and procedures for the development of epidemiological cutoff values for antifungal susceptibility testing. In: CLSI M57 document. 1st ed. Wayne: Clinical and Laboratory Standards Institute; 2016.
Turnidge J, Kahmeter G, Kronvall G. Statistical characterization of bacterial wild-type MIC value distributions and the determination of epidemiological cut-off values. Clin Microbiol Infect. 2006;12:418–25.
Espinel-Ingroff A, Arendrup MC, Pfaller MA, Bonfietti LX, Bustamante B, Canton, et al. Interlaboratory variability of caspofungin MICs for Candida spp. using CLSI and EUCAST methods: should the clinical laboratory be testing this agent? Antimicrob Agents Chemother. 2013. https://doi.org/10.1128/AAC.01519-13.
Rodriguez-Tudela JL, Almirante B, Rodriguez-Pardo D, Laguna F, Donnelly JP, Mouton JW, et al. Correlation of the MIC and dose/MIC ratio of fluconazole to the therapeutic response of patients with mucosal candidiasis and candidemia. Antimicrob Agents Chemother. 2007;51:3599–604.
Rodriguez-Tudela JL, Donnelly JP, Pfaller MA, Chryssantou E, Warn P, Denning DW, et al. Statistical analyses of correlation between fluconazole MICs for Candida spp. assessed by standard methods set forth by the European Committee on Antimicrobial Susceptibility Testing (E.Dis. 7.1) and CLSI (M27-A2). J Clin Microbiol. 2007;45:109–11.
Arendrup MC, Meletiadis J, Mouton JW, Guinea J, Cuenca-Estrella M, Lagrou K, et al. EUCAST technical note on isavuconazole breakpoints for Aspergillus, itraconazole breakpoints for Candida and updates for the antifungal susceptibility testing method documents. Clin Microbiol Infect. 2016;22:571.e1–4.
Alastruey-Izquierdo A, Melhem MSC, Bonfieti LX, Rodriguez-Tudela JL. Susceptibility test for fungi: clinical and laboratorial correlations in medical mycology Revista do Instituto de Medicina Tropical de São Paulo. 2015 https://doi.org/10.1590/S0036-46652015000700011
Arendrup MC, Prakash A, Meletiadis J, Sharmav C, Chowdhary A. Candida auris: comparison of the EUCAST and CLSI reference microdilution MICs for eight antifungal compounds and associated tentative ECOFFs. Antimicrob Agents Chemother. 2017;61:e00485–17. https://doi.org/10.1128/AAC.00485-17.
Trek Diagnostic Systems. Sensititre Yeast One: Yeast One susceptibility, v1.8. 2012: Trek Diagnostic Systems, Cleveland
bioMérieux SA. Etest antifungal susceptibility testing package insert. Chemin: bioMérieux SA; 2013.
bioMérieux SA. Etest performance, interpretive criteria and quality control ranges table. Chemin: bioMérieux SA; 2013.
Espinel-Ingroff A, Alvarez-Fernandez M, Cantón E, Carver PL, Chen SC-A, et al. A multi-center study of epidemiological cutoff values and detection of resistance in Candida spp. to anidulafungin, caspofungin and micafungin using the Sensititre Yeast One colorimetric method. Antimicrob Agents Chemother. 2015;59:6725–32. https://doi.org/10.1128/AAC.01250-15.
Espinel-Ingroff A, Arendrup M, Cantón E, Cordoba S, Dannaoui E, García-Rodríguez J, et al. Multicenter study of method-dependent epidemiological cutoff value for detection of resistance in Candida spp. and Aspergillus spp. to amphotericin B and echinocandins for the Etest agar diffusion method. Antimicrob Agents Chemother. 2017;61:e01792–16. https://doi.org/10.1128/AAC.01792-16.
•• Espinel-Ingroff A, Turnidge J, Alastruey-Izquierdo A, Dannaoui E, Garcia-Effron G, Guinea J, et al. Posaconazole MIC distributions for Aspergillus fumigatus species complex by four methods: impact of cyp51A mutations on estimation of epidemiological cutoff values. Antimicrob Agents Chemother. 2018;62:e01916–7. https://doi.org/10.1128/AAC.01916-17 This paper provides the impact of mutations in A. fumigatus MICs by four methods with a large number of mutant isolates.
•• Espinel-Ingroff A, Turnidge J, Alastruey-Izquierdo F, Botterel F, Canton E, Castro C, et al. Method-dependent epidemiological cutoff values (ECVs) for detection of triazole resistance in Candida, other yeast and Aspergillus species for the SYO colorimetric broth and Etest agar diffusion methods. Antimicrob Agents Chemother. 2019;63:e01651–18. https://doi.org/10.1128/AAC.01651-18. This paper provides triazole ECVs for commercial methods and provides MICs by these methods for a substantial number of mutants.
•• Sanglard D, Coste AT. Activity of isavuconazole and other azoles against Candida clinical isolates and yeast model systems with known azole resistance mechanisms. Antimicrob Agents Chemother. 2016;60:229–38. https://doi.org/10.1128/AAC.02157-15 An in-depth investigation on the molecular mechanisms of resistance to isavuconazole in Candida clinical isolates using the Saccharomyces cerevisiae model.
Grossman NT, Pham CD, Cleveland AA, Lockhart SR. Molecular mechanisms of fluconazole resistance in Candida parapsilosis isolates from a U.S. surveillance system. Antimicrob Agents Chemother. 2015;59:1030–7. https://doi.org/10.1128/AAC.04613-14.
Souza ACR, Fuchs BB, Pinhati HMS, Siqueira RA, Hagen F, Meis JF, et al. Candida parapsilosis resistance to fluconazole: molecular mechanisms and in vivo impact in infected Galleria mellonella larvae. Antimicrob Agents Chemother. 2015;59:6581–7. https://doi.org/10.1128/AAC.01177-15.
Berkow EL, Manigaba K, Parker JE, Barker KS, Kelly SL, Rogers PD. Multidrug transporters and alterations in sterol biosynthesis contribute to azole antifungal resistance in Candida parapsilosis. Antimicrob Agents Chemother. 2015;59:5942–50. https://doi.org/10.1128/AAC.01358-15.
•• Healey KR, Kordalewska M, Jiménez Ortigosa C, Singh A, Berrío I, Chowdhary A, et al. Limited ERG11 mutations identified in isolates of Candida auris directly contribute to reduced azole susceptibility. Antimicrob Agents Chemother. 2018;62:e01427–18. https://doi.org/10.1128/AAC.01427-18 An interesting paper showing for the first time that specific ERG11 mutations directly contributes to reduced azole susceptibility in Candida auris.
Garcia-Effron G, Kontoyiannis DP, Lewis RE, Perlin DS. Caspofungin-resistant Candida tropicalis strains causing breakthrough fungemia in patients at high risk for hematologic malignancies. Antimicrob Agents Chemother. 2008;52:4181–3.
Garcia-Effron G, Lee S, Park S, Cleary JD, Perlin DS. Effect of Candida glabrata FKS1 and FKS2 mutations on echinocandin sensitivity and kinetics of 1,3-D-glucan synthase: implication for the existing susceptibility breakpoint. Antimicrob Agents Chemother. 2009;53:3690–9.
Pfeiffer CD, Garcia-Effron G, Zaas AK, Perfect JR, Perlin DS, Alexander A. Breakthrough invasive candidiasis in patients on micafungin. J Clin Microbiol. 2010;53:2373–80.
Alexander BD, Johnson MD, Pfeiffer CD, Jimenez-Ortigosa C, Catania J, Booker R, et al. Increasing echinocandin resistance in Candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis. 2013;56:1724–32.
Shields RK, Hong Nguyen M, Press EG, Updike CL, Clancy CJ. Anidulafungin and micafungin MIC breakpoints are superior to that of caspofungin for identifying FKS mutant Candida glabrata strains and echinocandin resistance. Antimicrob Agents Chemother. 2013;57:6361–5.
Ostrosky-Zeichner L, Andes D. The role of in vitro susceptibility testing in the management of Candida and Aspergillus. J Infect Dis. 2017;216(S3):S452–7.
Lausch KR, Søgaard M, Rosenvinge FS, Johansen HK, Boysen T, Roder BL, et al. Treatment of candidemia in a nationwide setting: increased survival with primary echinocandin treatment. Infect Drug Resist. 2018;11:2449–59.
Mora-Duarte J, Betts R, Rotstein C, Lopes-Colombo A, Thompson-Moya L, Smietana J, et al. Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med. 2002;547:2020–9.
Lepak A, Castanheira M, Daniel Diekema D, Pfaller M, Andes D. Optimizing echinocandin dosing and susceptibility breakpoint determination via in vivo pharmacodynamic evaluation against Candida glabrata with and without fks mutations. Antimicrob Agents Chemother. 2012;52:5875–82.
• Boonstra JM, van der Elst KC, Veringa A, Jongedijk EM, Brüggemann RJ, Koster RA, et al. Pharmacokinetic properties of micafungin in critically ill patients diagnosed with invasive candidiasis. Antimicrob Agents Chemother. 2017;61:e01398–17. https://doi.org/10.1128/AAC.01398-17 An interesting paper highlighting the risk for inappropriate micafungin exposure and potentially inadequate antifungal treatment in critically ill patients diagnosed with invasive candidiasis.
Garcia-Effron G, Dilger A, Alcazar-Fuoli L, Park S, Mellado E, Perlin DS. Rapid detection of triazole antifungal resistance in Aspergillus fumigatus. J Clin Microbiol. 2008;46:1200–6. https://doi.org/10.1128/JCM.02330-07.
Mavridou E, Bruggemann RJM, Melchers WJG, Mouton JW, Verweij PE. Efficacy of posaconazole against three clinical Aspergillus fumigatus isolates with mutations in the cyp51A gene. Antimicrob Agents Chemother. 2010;54:860–5.
Meletiadis J, Mavridou E, Melchers WJG, Mouton JW, Verweij PE. Epidemiological cutoff values for azoles and Aspergillus fumigatus based on a novel mathematical approach incorporating cyp51A sequence analysis. Antimicrob Agents Chemother. 2012;56:2524–9.
Burgel P-R, Baixench M-T, Amsellem M, Audureau E, Chapron J, Kanaan R, et al. High prevalence of azole-resistant Aspergillus fumigatus in adults with cystic fibrosis exposed to itraconazole. Antimicrob Agents Chemother. 2012;56:869–74. https://doi.org/10.1128/AAC.05077-11.
Jeans AR, Howard SJ, Al-Nakeeb Z, Goodwin J, Gregson L, Majithiya JB, et al. Pharmacodynamics of voriconazole in a dynamic in vitro model of invasive pulmonary apergillosis: implications for in vitro susceptibility breakpoints. J Infect Dis. 2012;206:442–52.
Gregson L, Goodwin J, Johnson A, McEntee L, Moore CB, Richardson M, et al. In vitro susceptibility of Aspergillus fumigatus to isavuconazole: correlation with itraconazole, voriconazole, and posaconazole. Antimicrob Agents Chemother. 2013;57:5778–6578.
Lepak AJ, Marchillo K, VanHecker J, Andes DR. Posaconazole pharmacodynamic target determination against wild type and Cyp51 mutant isolates of Aspergillus fumigatus in an in vivo model of invasive pulmonary aspergillosis. Antimicrob Agents Chemother. 2013;57:579–85.
Lepak AJ, Marchillo K, VanHecker J, Andes DR. Isavuconazole (BAL4815) pharmacodynamic target determination in an in vivo murine model of invasive pulmonary aspergillosis against wild-type and cyp51 mutant isolates of Aspergillus fumigatus. Antimicrob Agents Chemother. 2013;57:6284–9.
Patel TS, Carver PL, Eschenauer GA. Are in vitro susceptibilities to azole antifungals predictive of clinical outcome in the treatment of candidemia? J Clin Microbiol. 2018;56:e01072–18. https://doi.org/10.1128/JCM.
Thompson GR III, Rendon A, dos Santos RR, Queiroz-Telles F, Ostrosky-Zeichner L, Azie N, et al. Isavuconazole treatment of cryptococcosis and dimorphic mycoses. Clin Infect Dis. 2016;63:356–62.
Aller AI, Martin-Mazuelos E, Lozano F, Gomez-Mateos J, Steele-Moore L, Espinel-Ingroff A, et al. Correlation of fluconazole MICs with clinical outcome in cryptococcal infection. Antimicrob Agents Chemother. 2000;44:1544–8.
Isla G, Leonardelli F, Tiraboschi IN, Refojo N, Hevia A, Vivot W, et al. First clinical isolation of an azole-resistant 2 Aspergillus fumigatus harboring a TR46/Y121F/T289A mutation in South America. Antimicrob Agents Chemother. 2018;62. https://doi.org/10.1128/AAC.00872-18.
Zhang M, Feng C-L, Chen F, He Q, Su X, Shi Y. Triazole resistance in Aspergillus fumigatus clinical isolates obtained in Nanjing, China. Chin Med J (Engl). 2017;20:130. https://doi.org/10.4103/0366-6999.201609.
Rodriguez-Tudela L, Alcazar-Fuoli L, Mellado E, Alastruey-Izquierdo A, Monzon A, Cuenca-Estrella M. Epidemiological endpoints to azole drugs in Aspergillus fumigatus. Antimicrob Agents Chemother. 2008;52:2468–72.
Andes DR, Ghannoum MA, Mukherjee PK, Kovanda LL, Lu Q, Jones ME, et al. Outcomes by minimum inhibitory concentrations for patients treated with isavuconazole or voriconazole for invasive aspergillosis in the phase 3 SECURE and VITAL trials. Antimicrobial Agents and Chemotherapy 2019;63:e01634–18. https://doi.org/10.1128/AAC.01634-18.
Dannaoui E, Desnos-Ollivier M, Garcia-Hermoso D, Grenouillet F, Cassaing S, Baixench M-T, et al. Candida spp. with acquired echinocandin resistance, France, 2004–2010. Emerg Infect Dis. 2012. https://doi.org/10.3201/eid1801.110556.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Clinical Mycology Lab Issues
Rights and permissions
About this article
Cite this article
Espinel-Ingroff, A., Sanguinetti, M. & Posteraro, B. Usefulness of Antifungal Reference In Vitro Susceptibility Tests as a Guide in Therapeutic Management. Curr Fungal Infect Rep 13, 33–43 (2019). https://doi.org/10.1007/s12281-019-0336-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-019-0336-2