Abstract
Over the past 100 years, Salvia miltiorrhiza f. alba (Lamiaceae) (RSMA) roots have been used to cure thromboangiitis obliterans (TAO) in local clinics. This study aimed to confirm the anti-thrombotic efficacy of 12 phenolic acids obtained from RSMA and to clarify the possible underlying mechanisms. The results of quantitative real-time polymerase chain reaction (qRT-PCR) and enzyme-linked immunosorbent assay (ELISA) experiments demonstrated that most of the phenolic acids markedly inhibited PAI-1 protein and mRNA levels but increased t-PA protein and mRNA levels in TNF-α-induced EA.hy926 cells (P < 0.05 or 0.001), with lithospermic acid displaying the strongest effect. In vitro anticoagulation and antiplatelet aggregation assays showed that lithospermic acid and salvianolic acid B significantly prolonged prothrombin time (PT), activated partial thromboplastin time (APTT), decreased fibrinogen concentration (FIB), and inhibited platelet aggregation induced by adenosine diphosphate (ADP) in rat blood. Both lithospermic acid and salvianolic acid B markedly down-regulated the expression of factor Xa and factor IIa on the external surface of EA.hy926 cells and demonstrated significant anti-factor IIa and anti-factor Xa activity using chromogenic substrates in vitro. Western blot results revealed that both lithospermic acid and salvianolic acid B also significantly inhibited the expression of TF, p-p65, p-p38, and pJNK proteins induced by TNF-α. These results indicated that all of the phenolic acids appeared to have some anti-thrombotic activity, with salvianolic acid B and lithospermic acid markedly decreasing the chance of thrombosis by regulating the NF-κB/JNK/p38 MAPK signaling pathway in response to TNF-α.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thrombosis is the process by which a solid mass of blood forms within living blood vessels or the heart, resulting in a thrombus. Thrombosis has been widely recognized as a common pathological mechanism underlying various thrombotic diseases such as coronary artery syndrome, ischemic stroke, and peripheral vascular diseases (Obermayer et al. 2018; Xue et al. 2018). The incidence and death rate of thrombotic diseases is high and has been increasing, which has obvious and serious potential for adverse effects on human life and health.
Vascular endothelial cells have a role in both anti-coagulation and pro-coagulation. In their normal state, intact endothelial cells exert an anticoagulant effect mainly by synthesizing anti-coagulants such as prostaglandin I2 (PGI2), tissue plasminogen activator (t-PA), and tissue factor pathway inhibitor (TFPI) (Kadri et al. 2019). However, once endothelial cells become dysfunctional or damaged, a variety of factors will be synthesized and released to promote platelet aggregation and thrombosis (Sioulis et al. 2009). Among these, t-PA can activate plasminogen and convert it to plasmin, and its inhibitor PAI is effective in the process of platelet adhesion and aggregation, thrombosis, and fibrinolysis inhibition (Tsantarliotou et al. 2019). The dynamic balance of t-PA and PAI-1 plays a decisive role in regulating fibrinolysis: a reduction in the t-PA/PAI-1 ratio can promote the formation of a thrombus, and any factor that affects the dynamic balance of t-PA and PAI-1 can affect the fibrinolytic process and promote thrombosis (Amiral et al. 2018; Huebner et al. 2018).
Tissue factor (TF) is a key initiator in the physiological coagulation process through activating the exogenous coagulation pathway (Lopes-Bezerra and Filler 2003). TF is mainly present in non-vascular cells. Under normal conditions, the content of TF in the blood is too low to trigger coagulation. However, TF is induced by thrombin, tumour necrosis factor-α (TNF-α), oxidized low-density lipoprotein (ox-LDL), and lipopolysaccharide (LPS), which are highly expressed in smooth muscle cells, monocytes/macrophages, vascular endothelial cells, and atheromatous plaques, respectively, in the pathological state. TF is essential in thrombosis. It produces the factor VIIa (FVIIa)-TF complex with factor VII (FVII) to activate factor X (FX) to factor Xa (FXa) and factor IX (FIX) to factor IXa (FIXa) to initiate coagulation. All of these lead to the production of a thrombus, resulting in thrombosis (Winckers et al. 2013; Edén et al. 2019). Therefore, TF provides a particularly promising target for anti-thrombotic drug therapy.
FXa is the intersection of the endogenous and exogenous coagulation pathways and is a vital component of the blood coagulation cascade. FXa can catalyse the conversion of factor II (FII) into factor IIa (FIIa). Recently, there has been a gradual increase in the use of FXa inhibitors as a target for the cure and prevention of thrombotic disorders (Hanslik et al. 2017). Three coagulation function indexes—prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombin time (TT)—can reflect the state of the body’s coagulation system to a certain extent. Among these, APTT and TT can reflect the functional state of endogenous coagulation, while PT is an indicator of the exogenous coagulation pathway (Ku et al. 2016). Platelet activation and aggregation play an important role in thrombus formation. Activated platelets undergo morphological changes, which induces their adhesion and aggregation through intracellular and extracellular signals and eventually leads to the formation of a blood clot (Koupenova et al. 2018).
The root of Salvia miltiorrhiza Bunge f. alba C.Y.Wu & H.W.Li (Lamiaceae) (RSMA), has been used as a Chinese herbal medicine for activating blood and removing stasis. For over 100 years it has been used at local clinics to treat patients with thrombotic diseases including thromboangiitis obliterans (TAO) (Liu et al. 2018).
Phenolic acids have been found to possess diverse pharmacological activities. Salvianolic acid A, or danshensu, has significant anti-platelet and anti-thrombotic effects by increasing cyclic adenosine monophosphate (cAMP) to inhibit platelet aggregation, inhibiting phosphoinositide 3-kinase (PI3K) to suppress platelet activation, and affecting the G protein-coupled receptor (GPCR) signaling pathway (Fan et al. 2010). Salvianolic acid B can be used to inhibit platelet aggregation as a phosphodiesterase (PDE) inhibitor and P2Y12 antagonist, and danshensu inhibits platelet activity, possibly through the inhibition of calcium influx (Fei et al. 2017).
In our previous study, we reported that phenolic acids had anti-inflammation properties through the TLR4/NF-κB signaling pathway in LPS-induced THP-1 cells (Liu et al. 2018). It has also been found that a total phenolic acid extract from RMSA—a mixture of danshensu, salvianolic acid A, salvianolic acid B, rosmarinic acid, lithospermic acid, and salvianolic acid E (Zhu et al. 2012)—and SalB (purity > 96%) (Zhang et al. 2020) had effective anti-thrombotic effects in rats with TAO induced by sodium laurate injection.
In the present study, the anti-thrombotic effects of 12 phenolic acids on TNF-α-induced EA.hy926 cells were determined, along with their potential mechanisms. The structures of the 12 phenolic acids obtained from RSMA are shown in Fig. 1: salvianolic acid A (1), isosalvianolic acid A (2), rosmarinic acid-3-O-glucoside (3), methyl 3,4-dihydroxyphenyl lactate (4), salvianolic acid C (5), rosmarinic acid (6), pro-lithospermic acid (7), danshensu (8), salvianolic acid B (9), lithospermic acid (10), 3,4-dihydroxybenzaldehyde (11), and 2,3-O-diisoferacyl tartaric acid (12) (Zhang et al. 2017; Liu et al. 2018).
Materials and methods
Cell culture
Human EA.hy926 cells were purchased from the National Infrastructure of Cell Line Resource and cultivated in DMEM (Gibco, Carlsbad, CA, USA). The cell culture was then supplemented with penicillin (100 U/mL), 10% fetal bovine serum (FBS) (Gibco), and streptomycin (100 µg/mL) under standard culture conditions (5% CO2 and 37 °C), with a medium change every 2–3 days.
CCK-8 cell viability test
The CCK-8 assay (Beyotime, Shanghai, China) was used to examine the growth inhibition of EA.hy926 cells treated with the 12 phenolic acids. Cells in the logarithmic growth phase were seeded in 96-well plates (1 × 104 cells/cm2) and then incubated with different concentrations of phenolic acid (1, 5, 25, or 50 μM) for 24 h. CCK-8 solution (5 μL) was then added to each well and the incubation was prolonged for 2–4 h. The absorbance at 450 nm was then determined using a microplate reader (Bio-Rad, Hercules, CA, USA).
Detection of PAI-1 and t-PA protein levels by ELISA
EA.hy926 cells within the logarithmic growth phase were seeded in 96-well plates (1 × 104 cells/cm2) and incubated with different concentrations of phenolic acid (1, 5, or 25 μM) for 1 h. They were then separately co-incubated with TNF-α (10 ng/mL) or without TNF-α for 24 h. ELISA kits (Abcam, Cambridge, UK) were used to determine the levels of PAI-1 and t-PA proteins according to the manufacturer’s instructions and the absorbance at 450 nm was determined using a microplate reader (Bio-Rad).
Detection of PAI-1 and t-PA RNA levels by qRT-PCR
EA.hy926 cells in the logarithmic growth phase were seeded in 6-well plates (5 × 104 cells/cm2). Cells were pre-treated with phenolic acid (1, 5, or 25 μM) for 1 h and then co-incubated with TNF-α (10 ng/mL) or without TNF-α for 24 h. TRIzol reagent (Invitrogen, Carlsbad, CA, USA) was used to extract the total RNA from EA.hy926 cells according to the standard procedure, after which M-MLV Reverse Transcriptase (Invitrogen) was used to reverse-transcribe the RNA (5 μg) into cDNA. For the reverse transcription, a mixture of 2 × SuperReal PreMix Plus (5 μL; Tiangen, Beijing, China), cDNA template (2 μL, 1:3) and primers (3 μL; refer to Table 1) was used. The produced samples were run three times with the QPCR thermocycler (Eppendorf, Hamburg, Germany) according to the following procedure: 95 °C for 3 min, followed by 40 cycles of 95 °C for 15 s, 60 °C for 20 s and 72 °C for 30 s. The final result was used to compute the relative expression level by 2−ΔΔCt.
Anticoagulation and antiplatelet aggregation assays of phenolic acids in vitro
Wistar rats (230–250 g) were purchased from the Experimental Animal Center of Shandong University (Jinan, Shandong, China). After fasting for 8 h and anesthetization with pentobarbital, blood was collected from the abdominal aorta of the rats and anticoagulant agent sodium citrate (3.8%, 1:9 v/v) was added. The collected blood was centrifuged at 3000 rpm for 10 min at room temperature to obtain the upper plasma. The upper plasma (50 μL) and different concentrations of phenolic acid solution (10 μL) were mixed in a test cup and incubated at 37 °C. The PT, APTT, and TT were determined by routine laboratory assays using a semi-automated coagulation analysis instrument (RT-2204C, Rayto, Shenzhen, China). Fibrinogen (FIB) concentration was determined using the Clauss method.
Platelet-rich plasma (PRP) was obtained by centrifuging the above-collected blood at 1000 rpm for 6 min at room temperature. The remaining blood samples were centrifuged at 3000 rpm for another 15 min to afford platelet-poor plasma (PPP). PRP (0.3 mL), with the platelet count adjusted to 4 × 108/mL, was placed in a cuvette and stirred by rotor at 37 °C for 5 min, following which adenosine diphosphate (ADP; 6 μM) was added. Aggregation was measured with a platelet aggregometer (Chrono-log 700, Havertown, PA, US). Data are expressed as the percentage of maximal aggregation.
Production of FXa on the surface of EA.hy926 cells
EA.hy926 cells in the logarithmic growth phase were seeded in 96-well plates (1 × 104 cells/cm2). The cells were then incubated with or without salvianolic acid B (9) or lithospermic acid (10) (1, 5 or 25 μM) for 1 h, after which TNF-α (10 ng/mL) was added and the cells incubated for a further 6 h. In the presence or absence of anti-TF IgG (25 μg/mL), FVIIa (10 nm; Aglyco, Beijing, China) was added and the cells were incubated for 5 min at 37 °C. Finally, FX (175 nm; Aglyco) was added to 100 μL of solution and the mixture incubated for 15 min at 37 °C. FXa production was determined by adding S-2765 (3 mmol/mL, 60 μL; Aglyco) and measuring the absorbance at 405 nm with a microplate reader (Bio-Rad).
FIIa production on the surface of EA.hy926 cells
EA.hy926 cells in the logarithmic growth phase were seeded in 96-well plates (1 × 104 cells/cm2) and then incubated with or without compound 9 or 10 (1, 5 or 25 μM) for 1 h. FXa and FVa (175 nm; Aglyco) were added into the solution and the cells were incubated for 10 min, then pro-thrombin (1 μM; Aglyco) was added and the production of FIIa was determined by adding S-2238 (3 mmol/mL, 60 μL; Aglyco) and measuring the absorbance at 405 nm with a microplate reader (Bio-Rad).
Anti-FIIa and anti-FXa activity in vitro
The in vitro anti-FIIa and anti-FXa activity of compounds 9 and 10 was confirmed using the chromogenic substrate method. Different concentrations of compounds 9, 10, aspirin, or heparin (National Institutes for Food and Drug Control, Beijing, China) (50 μL) were mixed with antithrombin (AT; 0.25 IU/mL, 30 μL; Aglyco) in 96-well plates at 37 °C for 2 min. FXa (1 IU/mL, 60 μL; Aglyco) or FIIa (1 IU/mL, 60 μL; Aglyco) was then added for 1 min. Finally, S-2765 (3 mmol/mL, 60 μL; Aglyco) or S-2238 (3 mmol/mL, 60 μL; Aglyco) was added to evaluate the activity of FXa or FIIa. The absorbance at 405 nm was measured with a microplate reader (Bio-Rad).
Western blot analysis
EA.hy926 cells in the logarithmic growth phase were seeded in 6-well plates (5 × 104 cells/m2). The cells were then incubated with compound 9 or 10 (1, 5 or 25 μM) for 1 h, and then with TNF-α (10 ng/mL) for 4 h. The cells were washed twice with cold PBS and then RIPA buffer containing protease and phosphatase inhibitors (Beyotime, Shanghai, China) was used for pyrolysis. The protein concentration was determined using an enhanced BCA protein assay kit (Beyotime) according to the manufacturer’s instructions.
Equal amounts of protein samples were separated on SDS-PAGE gels and then moved onto a 0.45 um PVDF membrane. The membranes were sealed in 5% skimmed milk for 1–2 h at room temperature and were then incubated with primary antibodies (Proteintech, Chicago, IL, USA) against TF (1:6000), p65 (1:1000), p-p65 (1:1000), p38 (1:1000), p-p38 (1:1000), pJNK (1:1000), JNK (1:1000), and β-actin (1:1000) at 4 °C with gentle shaking overnight. The PVDF membranes were rinsed three times with TBST and then incubated with Peroxidase-conjugated AffiniPure Goat Anti-Mouse or Anti-Rabbit secondary antibodies (at a ratio of 1:3000, Proteintech) for 1 h at ambient temperature. Finally, enhanced chemiluminescence reagents (Millipore, Billerica, MA, USA) were used to visualize the proteins.
Statistical analysis
All data were obtained from at least three independent experiments and are expressed in the format of mean ± standard error of the mean (SEM). GraphPad Prism software version 8.0 was used to determine differences between groups by one-way analysis of variance (ANOVA). The statistical significance was set as P < 0.05.
Results
Influence of phenolic acids on the viability of EA.hy926 cells
After incubation of EA.hy926 cells with various concentrations of phenolic acids 1–12 (1, 5, 25 or 50 μM) for 24 h, the phenolic acid cytotoxicity was determined using CCK-8 analysis. The cell survival rate was above 95% in the 1, 5 and 25 μM groups and no toxicity was observed (Table S1).
Effects of phenolic acids on the protein and mRNA levels of PAI-1 and t-PA in TNF-α–induced EA.hy926 cells
The balance between t-PA and its inhibitor PAI-1 is known to be integral to the thrombosis process. The influence of phenolic acids 1–12 on the protein (Table 2) and mRNA (Fig. 2) levels of PAI-1 and t-PA in EA.hy926 cells was investigated using ELISA and qRT-PCR, respectively. The results showed that compounds 1, 2, 9, 10, and aspirin significantly suppressed PAI-1 expression at the mRNA and protein levels with a dose-dependent relationship (P < 0.001). In particular, PAI-1 protein inhibition by compound 10 (lithospermic acid) was 34.5% at a concentration of 25 μM, which was close to that of aspirin (38.9%). Additionally, compounds 1, 9, 10, and aspirin showed potent up-regulation of the mRNA and protein expression of t-PA in EA.hy926 cells with a dose-dependent relationship (P < 0.001). Compound 10 promoted a 55.9% increase in t-PA protein levels at a concentration of 25 μM, which was just weaker than that obtained using aspirin (60.8%). The ratio of t-PA/PAI-1 was significantly increased by all compounds except for 6, 7, and 8, which displayed a tendency for equivalence, and compound 10 significantly increased the ratio of t-PA/PAI-1 at concentrations of 5 and 25 µM (P < 0.01). These results indicated compound 10 to be a potential anti-thrombotic drug through up-regulation of t-PA expression and maintenance of an appropriate balance of t-PA and PAI-1. Also, because compound 9 (salvianolic acid B) was the most abundant salvianolic acid in RMSA, it was selected for further studies along with compound 10.
Effects of lithospermic acid and salvianolic acid B on TNF-α–induced FXa and FIIa production in EA.hy926 cells
Following on from the above findings, the inhibitory effect of salvianolic acid B (9) and lithospermic acid (10) on the production of FXa and FIIa in EA.hy926 cells was explored by chromogenic substrate assay. It is known that FVIIa can complex with TF to activate FX to FXa and that TF can be induced by the TNF-α present in EA.hy926 cells (Edén et al. 2019). This was consistent with the result obtained in the present study (Fig. 3a), where TNF-α significantly induced the production of FXa in EA.hy926 cells compared to the untreated group. It is also known that anti-TF IgG can inhibit the expression of FXa by binding to TF with high affinity and specificity (Lee et al. 2016). Compounds 9 and 10 significantly decreased FXa production in a concentration-dependent way, with compound 10 showing stronger anti-FXa activity than that of 9. As shown in Fig. 3b, both 9 and 10 also markedly decreased the expression of FIIa, with a similar effect to that of aspirin.
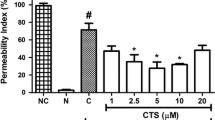
Inhibition by compounds 9 and 10 of (A) FXa and (B) FIIa production in EA.hy926 cells; (C) anti-FXa and (D) anti-FIIa activity of compounds 9 and 10 in vitro as determined by chromogenic substrate assay, and (E) effects of phenolic acids on platelet aggregation induced by ADP in vitro. All results were determined from three independent tests. Data are expressed as mean ± SEM. ###P < 0.001 vs. the control group. *P < 0.05, **P < 0.01, ***P < 0.001 vs. the prothrombin (FII) group
Anti-FIIa and anti-FXa activity of salvianolic acid B and lithospermic acid in vitro
To further investigate the effects of salvianolic acid B (9) and lithospermic acid (10) on the activity of FXa and FIIa, thrombin was treated with 9 or 10 in vitro and FXa and FIIa activity were determined using the chromogenic substrate assay. Heparin can induce a configuration change in AT by binding to it, which increases the ability of AT to bind to and inactivate clotting factors. The main targets of the AT and heparin complex are FXa and FIIa, so heparin and aspirin were used as positive controls. The concentrations of compounds and aspirin were 0.0001–100 μM and heparin was 0.0001–100 μg/mL. At a concentration of 100 µM, the relative FXa activity in the presence of 9, 10, and aspirin was 41.2%, 29.3%, and 52.0%, respectively (Fig. 3c), while the relative FIIa activity in the presence of 9 (54.6%) and 10 (54.8%) was similar to that of the aspirin group (55.3%) at a concentration of 100 µM (Fig. 3d; Table S4). These results indicated that lithospermic acid had the strongest anti-FXa activity and that all three compounds had similar anti-FIIa activity in vitro.
Effects of phenolic acids on the coagulation parameters and platelet aggregation induced by ADP in vitro
The effect of phenolic acids including compounds 1, 8, 9, and 10 on the coagulation parameters was determined by routine laboratory assays using rat blood. As shown in Table 3, compared with the control group, several phenolic acids had a significant effect on the PT, APTT, TT, and FIB at concentrations higher than 75 μM. Specifically, compound 10 significantly prolonged PT and decreased the FIB at 300 μM (P < 0.001), and compounds 1, 9, and 10 markedly prolonged APTT (P < 0.001) at 150 or 300 μM.
Furthermore, the platelet aggregation induced by ADP was significantly inhibited by compounds 1, 8, 9, and 10 at concentrations of 100 and 200 μM (P < 0.05 or P < 0.001), as shown in Fig. 3e. Among these, the greatest inhibitory effect was with compounds 9 and 10 at concentrations of 100 and 200 μM, respectively. These results revealed that these phenolic acids 9 and 10 have anti-thrombosis effects in vitro.
Effects of lithospermic acid and salvianolic acid B on TF expression in TNF-α-induced EA.hy926 cells
TNF-α is a strong TF inducer, which can enhance the expression and increase the concentration of TF in vascular endothelial cells (Winckers et al. 2013). As shown in Fig. 4a and b, TNF-α significantly induced TF expression in EA.hy926 cells (P < 0.001). Additionally, treatment of cells with increasing concentrations of salvianolic acid B (9) or lithospermic acid (10) led to decreased TNF-α–induced TF protein expression, indicating that 9 and 10 could inhibit the TF protein expression that was stimulated by TNF-α in EA.hy926 cells.
Effects of compounds 9 and 10 on the expression of (A and B) TF, (C and D) p-p38 and p38, (E and F) p-p65 and p65 and (E and G) pJNK and JNK in TNF-α‒stimulated EA.hy926 cells. All results were determined from three independent tests. Data are expressed as mean ± SEM. ###P < 0.001 vs. the control group. *P < 0.05, **P < 0.01, ***P < 0.001 vs. TNF-α group
Effects of lithospermic acid and salvianolic acid B on p-p65, p65, p-p38, p38, pJNK, and JNK expression in TNF-α-induced EA.hy926 cells
TNF-α can mediate the inhibition of t-PA expression through the p38 MAPK/NF-κB pathway in vascular endothelial cells (Ulfhammer et al. 2006) and induce TF expression through the NF-κB and MAPK pathways in endothelial cells (Breitenstein et al. 2009). In this study, after incubation of EA.hy926 cells with TNF-α, the p-NF-κB p65, p-p38, MAPK, and pJNK protein levels were significantly increased compared with those of TNF-α-untreated control cells (Fig. 4c–g). Following treatment with salvianolic acid B (9) or lithospermic acid (10), the expression of p-NF-κB p65, p-p38 MAPK, and pJNK proteins was significantly decreased compared with TNF-α-stimulated cells. These results revealed that compounds 9 and 10 could block thrombosis by regulating the p38 MAPK/JNK/NF-κB signaling pathway in EA.hy926 cells.
Discussion
Inflammation is an important contributor to thrombosis and is closely correlated with coagulation and fibrinolysis systems. Inflammatory mediators such as TNF-α and IL-6 can accumulate in the related thrombosis and coagulation pathways. Mounting evidence has indicated that the over-expression of TNF-α can increase the risk of thrombosis development: it can induce thrombosis by stimulating PAI-1 and TF secretion by vascular cells (Esmon 2004). TNF-α can also induce changes in endothelial cell permeability, leading to local inflammation and edema formation. As a strong stimulating factor, TNF-α can activate the coagulation system, which can manifest as the down-regulation of physiological anticoagulant mechanisms and inhibition of fibrinolysis (Prabhakara and Smyth 2013). Additionally, t-PA can dissolve blood clots because it has a high affinity for fibrin (De Pergola et al. 1997).
In this study, the levels of PAI-1 and TF secretion in TNF-α-induced EA.hy926 cells were decreased and the t-PA level was increased in the presence of salvianolic acid B or lithospermic acid, with a concentration-dependent relationship. The result for salvianolic acid B suppression of TNF-α–induced PAI-1 was consistent with the findings of a previous study using human umbilical vein endothelial cells (HUVECs) at lower salvianolic acid B concentrations of 0.05 and 0.15 µM (Zhou et al. 2005).
The formation of a thrombus is related to the aggregation, adhesion, and release of platelets. Clotting time and PT can reflect the functional status of internal and external coagulation (Ku et al. 2014). FXa is the center of the coagulation cascade (Nar et al. 2001) and is recognized as an ideal target for anticoagulant therapy. FXa inhibitors have also become a research hotspot for anticoagulant drugs. FIIa can activate platelets and catalyze the cleavage of fibrinogen into fibrin by cutting off the N-terminal of protease-activated receptors (PARs), and the cross-linking of platelets and fibrin can eventually lead to the formation of blood clots (Bettina et al. 2013). The results of this study demonstrated that lithospermic acid and salvianolic acid B could significantly prolong PT at 300 μM (P < 0.001) and inhibit platelet aggregation at 100 and 200 μM concentrations (P < 0.001). Both compounds also markedly suppressed the production of FXa and FIIa in EA.hy926 cells. Furthermore, lithospermic acid had similar anti-FIIa activity to that of salvianolic acid B and aspirin and displayed a stronger in vitro inhibitory effect on FXa than both salvianolic acid B and aspirin.
The activation of many signaling pathways in the development of a thrombus can not only activate multiple transcription factors including NF-κB and active protein-1 (AP-1), but also enhance the expression of many clotting factors such as TF, FXII, FX, and FIIa (Rauch et al. 2001). NF-κB mediates the interaction between endothelial cells, platelets, and inflammatory factors, resulting in a coagulation and fibrinolysis imbalance that eventually causes thrombosis (Ward et al. 2017). The up-regulation of NF-κB and AP-1 occurs as a response to the activation of multiple upstream pathways, with extensive involvement of the JNK and p38 MAPK pathways (Hsu et al. 2000). The p38 MAPK signaling pathway can be activated by TNF-α, and subsequently activate the downstream transcription factor JNK and activating transcription factor 2 (ATF-2), which promote the formation of clots by inducing increased PAI-1 (Fanjul-Fernández et al. 2010). TNF-α also can suppress t-PA expression in vascular endothelial cells through the p38 MAPK and NF-κB pathways (Ulfhammer et al. 2006). In this study, the results revealed lithospermic acid and salvianolic acid B to play key anti-thrombotic roles via regulation of the NF-κB/JNK/p38 MAPK signaling pathway.
Generally, this research demonstrated that the majority of the 12 phenolic acids extracted from RSMA roots had anti-thrombotic activity and could simultaneously decrease PAI-1 expression and increase t-PA secretion in TNF-α-induced EA.hy926 cells. In particular, lithospermic acid and salvianolic acid B displayed significant inhibitory effects on PAI-1 and TF expression and promoted t-PA expression via the NF-κB/JNK/p38 MAPK signaling pathway. Furthermore, lithospermic acid showed excellent FIIa and FXa resistance activity by significantly prolonging the PT and APTT and inhibiting the platelet aggregation caused by ADP. The potential anti-thrombosis pathway of compounds 9 and 10 in TNF-α–induced EA.hy926 cells is shown in Fig. 5. All the experimental results indicated the potential for use of the 12 phenolic acids from RMSA, especially salvianolic acid B and lithospermic acid, in curing blood stasis diseases. Therefore, this study provides a theoretical foundation to underpin the clinical application of RMSA as a traditional herb in curing thrombotic diseases such as TAO.
Process by which compounds 9 and 10 mediated thrombosis signaling in TNF-α–induced EA.hy926 cells. Compounds 9 and 10 could inhibit thrombus formation by reducing PAI-1, FXa, FIIa, and TF expression and promoting t-PA expression in TNF-α–induced EA.hy926 cells via the NF-κB/JNK/p38 MAPK signaling pathway
In conclusion, this study showed that—of the twelve phenolic acids extracted from Salvia miltiorrhiza f. alba (RSMA) root—lithospermic acid had the strongest anti-thrombotic activity, followed by salvianolic acid B. Lithospermic acid could inhibit the formation of a thrombus via the NF-κB/JNK/p38 MAPK signaling pathway. These findings indicated that lithospermic acid has great potential value for anti-thrombotic drug exploration.
References
Amiral J, Laroche M, Seghatchian J (2018) A new assay for global fibrinolysis capacity (GFC): investigating a critical system regulating hemostasis and thrombosis and other extravascular functions. Transfus Apher Sci 57(1):118–126. https://doi.org/10.1016/j.transci.2018.02.020
Breitenstein A, Camici GG, Tanner FC (2009) Tissue factor: beyond coagulation in the cardiovascular system. Clin Sci 118(3–4):159–172. https://doi.org/10.1042/CS20080622
Edén D, Panagiotou G, Mokhtari D, Eriksson JW, Åberg M, Siegbahn A (2019) Adipocytes express tissue factor and FVII and are procoagulant in a TF/FVIIa-dependent manner. Ups J Med Sci 124(3):158–167. https://doi.org/10.1080/03009734.2019.1645248
Esmon CT (2004) Crosstalk between inflammation and thrombosis. Maturitas 61(1–2):122–131
Fan HY, Fu FH, Yang MY, Xu H, Zhang AH, Liu K (2010) Antiplatelet and antithrombotic activities of salvianolic acid A. Thromb Res 126(1):E17–E22. https://doi.org/10.1016/j.thromres.2010.04.006
Fanjul-Fernández M, Folgueras AR, Cabrera S, López-Otín C (2010) Matrix metalloproteinases: evolution, gene regulation and functional analysis in mouse models. Biochim Biophys Acta 1803(1):3–19. https://doi.org/10.1016/j.bbamcr.2009.07.004
Fei YX, Wang SQ, Yang LJ, Qiu YY, Li YZ, Liu WY, Xi T, Fang WR, Li YM (2017) Salvia miltiorrhiza Bunge (Danshen) extract attenuates permanent cerebral ischemia through inhibiting platelet activation in rats. J Ethnopharmacol 207:57–66. https://doi.org/10.1016/j.jep.2017.06.023
Hanslik A, Kitzmüller EE, Tran US, Thom K, Karapetian H, Prutsch N, Voitl J, Michel-Behnke I, Newall F, Male C (2017) Anti-activated factor II assay for monitoring unfractionated heparin in children: results of the HEARTCAT study. J Thromb Haemost 15(1):38–46. https://doi.org/10.1111/jth.13539
Hsu T, Young MR, Cmarik J, Colburn NH (2000) Activator protein 1 (AP-1) and nuclear factor κB (NF-κB)–dependent transcriptional events in carcinogenesis. Free Radic Biol Med 28(9):1338–1348. https://doi.org/10.1016/S0891-5849(00)00220-3
Huebner BR, Moore EE, Moore HB, Stettler GR, Nunns GR, Lawson P, Sauaia A, Kelher M, Banerjee A, Silliman CC (2018) Thrombin provokes degranulation of platelet α-granules leading to the release of active plasminogen activator inhibitor-1 (PAI-1). Shock 50(6):671–676. https://doi.org/10.1097/SHK.0000000000001089
Kadri OE, Surblyte M, Chandran VD, Voronov RS (2019) Is the endothelial cell responsible for the thrombus core and shell architecture? Med Hypotheses 129:109–244. https://doi.org/10.1016/j.mehy.2019.109244
Koupenova M, Clancy L, Corkrey HA, Freedman JE (2018) Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ Res 122(2):337–351. https://doi.org/10.1161/CIRCRESAHA.117.310795
Kovács B, Bereczky Z, Oláh Z, Gindele R, Kerényi A, Selmeczi A, Boda Z, Muszbek L (2013) The superiority of anti-FXa assay over anti-FIIa assay in detecting heparin-binding site antithrombin deficiency. Am J Clin Pathol 140(5):675–679. https://doi.org/10.1309/AJCPVY4Z9XZMFOTH
Ku SK, Yoon EK, Lee W, Kwon S, Lee T, Bae JS (2016) Antithrombotic and antiplatelet activities of pelargonidin in vivo and in vitro. Arch Pharm Res 39(3):398–408. https://doi.org/10.1007/s12272-016-0708-x
Lee W, Lee J, Kulkarni R, Kim M, Hwang JS, Na M, Bae J (2016) Antithrombotic and antiplatelet activities of small-molecule alkaloids from Scolopendra subspinipes mutilans. Sci Rep 6:21956. https://doi.org/10.1038/srep21956
Liu HM, Ma SL, Xia HR, Lou HX, Zhu FL, Sun LR (2018) Anti-inflammatory activities and potential mechanisms of phenolic acids isolated from Salvia miltiorrhiza f. alba roots in THP-1 macrophages. J Ethnopharmacol 222:201–207. https://doi.org/10.1016/j.jep.2018.05.008
Lopes-Bezerra LM, Filler SG (2003) Endothelial cells, tissue factor and infectious diseases. Braz J Med Biol Res 36(8):987–991. https://doi.org/10.1590/S0100-879X2003000800004
Nar H, Bauer M, Schmid A, Stassen J, Wienen W, Priepke HWM, Kauffmann IK, Ries UJ, Hauel NH (2001) Structural basis for inhibition promiscuity of dual specific thrombin and factor Xa blood coagulation inhibitors. Structure 9(1):29–37. https://doi.org/10.1016/S0969-2126(00)00551-7
Obermayer G, Afonyushkin T, Binder CJ (2018) Oxidized low-density lipoprotein in inflammation-driven thrombosis. J Thromb Haemost 16(3):418–428. https://doi.org/10.1111/jth.13925
Pergola GD, Mitrio VD, Giorgino F, Sciaraffia M, Minenna A, Bari LD, Pannacciulli N, Giorgino R (1997) Increase in both pro-thrombotic and anti-thrombotic factors in obese premenopausal women: relationship with body fat distribution. Int J Obes 21(7):527–535. https://doi.org/10.1038/sj.ijo.0800435
Prabhakara N, Smyth SS (2013) Inflammation and thrombosis in cardiovascular disease. Curr Opin Hematol 20(5):457–463. https://doi.org/10.1097/MOH.0b013e328364219d
Rauch U, Osende JI, Fuster V, Badimon JJ, Fayad Z, Chesebro JH (2001) Thrombus formation on atherosclerotic plaques: pathogenesis and clinical consequences. Ann Intern Med 134(3):224. https://doi.org/10.7326/0003-4819-134-3-200102060-00014
Sae-Kwang Ku, Lee I-C, Bae J-S (2014) Antithrombotic activities of oroxylin A in vitro and in vivo. Arch Pharm Res 37(5):679–686. https://doi.org/10.1007/s12272-013-0233-0
Sioulis A, Malindretos P, Makedou A, Makris P, Grekas D (2009) Coagulation factors as biological risk markers of endothelial dysfunction. Association with the thrombotic episodes of chronic hemodialysis patients. Hippokratia 13(4):237–241. https://doi.org/10.1093/fampra/cmp051
Tsantarliotou MP, Lavrentiadou SN, Psalla DA, Margaritis IE, Kritsepi MG, Zervos IA, Latsari MI, Sapanidou VG, Taitzoglou IA, Sinakos ZM (2019) Suppression of plasminogen activator inhibitor-1 (PAI-1) activity by crocin ameliorates lipopolysaccharide-induced thrombosis in rats. Food Chem Toxicol 125:190–197. https://doi.org/10.1016/j.fct.2019.01.001
Ulfhammer E, Larsson P, Karlsson L, Hrafnkelsdóttir T, Bokarewa M, Tarkowski A, Jern S (2006) TNF-alpha mediated suppression of tissue type plasminogen activator expression in vascular endothelial cells is NF-kappa B- and p38 MAPK-dependent. J Thromb Haemost 4(8):1781–1789. https://doi.org/10.1111/j.1538-7836.2006.02035.x
Ward AO, Caputo M, Angelini GD, George SJ, Zakkar M (2017) Activation and inflammation of the venous endothelium in vein graft disease. Atherosclerosis 265:266–274. https://doi.org/10.1016/j.atherosclerosis.2017.08.023
Winckers K, Cate HT, Hacken TM (2013) The role of tissue factor pathway inhibitor in atherosclerosis and arterial thrombosis. Blood Rev 27(3):119–132. https://doi.org/10.1016/j.blre.2013.03.001
Xue X, Jiang LS, Duenninger E, Muenzel M, Guan S, Fazakas A, Cheng FZ, Illnitzky J, Keil T, Yu JT (2018) Impact of chronic kidney disease on Watchman implantation: experience with 300 consecutive left atrial appendage closures at a single center. Heart Vessels 33(9):1068–1075. https://doi.org/10.1007/s00380-018-1157-x
Zhang Y, Zhu HL, Sun LR (2017) Phenolic acids from the roots of Salvia miltiorrhiza var alba. Chin Med Mater 40(4):855–858. https://doi.org/10.13863/j.issn1001-4454.2017.04.021
Zhang ZR, Ji JB, Zhang DW, Ma MQ, Sun LR (2020) Protective effects and potential mechanism of salvianolic acid B on sodium laurate-induced thromboangiitis obliterans in rats. Phytomedicine. https://doi.org/10.1016/j.phymed.2019.153110s
Zhou Z, Liu Y, Miao AD, Wang SQ (2005) Salvianolic acid B attenuates plasminogen activator inhibitor type 1 production in TNF-alpha treated human umbilical vein endothelial cells. J Cell Biochem 96(1):109–116. https://doi.org/10.1002/jcb.20567
Zhu HL, Zhang DW, Sun LR, Ji JB, Wu K (2012) Effects of total salvianolic acid from Salvia miltiorrhiza f. alba on thromboangiitis obliterans in rats. Chin Tradit Herbal Drugs 43(8):1565–1569
Acknowledgements
Natural Science Foundation of Shandong Province (No. ZR2019MH088) provided assistance in the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interests should be declared by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zheng, X., Liu, H., Ma, M. et al. Anti-thrombotic activity of phenolic acids obtained from Salvia miltiorrhiza f. alba in TNF-α-stimulated endothelial cells via the NF-κB/JNK/p38 MAPK signaling pathway. Arch. Pharm. Res. 44, 427–438 (2021). https://doi.org/10.1007/s12272-021-01325-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-021-01325-7