Abstract
There has been no attempt to apply protein-based markers of exfoliated cervical cells (ECCs) for primary screening of cervical cancer. In the present study, the levels of six tumor-associated protein [TAPs: Sialyl Lewis A (SLeA), Cancer Antigen 15-3 (CA 15-3), p53, heat shock protein (Hsp)70, Hsp27 and squamous cervical carcinoma antigen (SCCA)]and of two human papillomavirus (HPV) viral proteins (HPV16 E7 and HPV16 L1) of ECCs lysates were evaluated by enzyme-linked immunosorbent assays (ELISAs).The wells of 96-well plates were coated with the ECCs lysates from normal, cervical intraepithelial neoplasia (CIN) I, CIN II, CIN III and cancer groups, and candidate proteins were detected by relevant antibodies. SLeA level decreased with increasing severity of lesions, whereas the levels of other candidate proteins increased. SLeA, HPV16 L1 and p53 levels appeared more useful for detecting cervical lesions than the other candidates. The combination of ELISA-SLeA and ELISA-HPV16 L1 could efficiently detect cervical lesions from normal. The combination of ELISA-SLeA and ELISA-p53 could powerfully discriminate cancer from normal with 91.3% sensitivity and 96.7% specificity. The protein levels of ECCs have great potential as biomarkers for primary screening of cervical cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the fourth most common cancer in women worldwide, and almost 100% of cervical cancers are caused by human papillomavirus (HPV) (Snijders et al. 2006; Simayi et al. 2013). HPV types are subdivided into low-risk (wart-causing) and high-risk (cancer-causing) and type 16 HPV itself causes nearly 50% of cervical cancers (Ghittoni et al. 2015). Invasive cervical cancer may develop from a preinvasive state termed a cervical intraepithelial neoplasia (CIN) (Snijders et al. 2006) and treatment at the CIN stage can prevent the development of invasive cervical cancer (Mishra et al. 2011). Therefore, early diagnosis and treatment of CINs provide an opportunity to reduce mortality from cervical cancer.
Pap smear test is the most common primary screening program for cervical cancer and is used to detect abnormal exfoliated cervical cells (ECCs), which are collected from superficial layer cells of the cervical squamous epithelium (Williams et al. 1998; Habis et al. 2004). Gynecologists then decide whether to carry out colposcopy to confirm lesions based on the results of the Pap test (Sahasrabuddhe et al. 2011). CIN is graded into levels I, II and III depending on the proportion of the thickness of the epithelium showing mature and differentiated cells (Mishra et al. 2011). Almost 90% of CIN I (low grade CIN) cases regress spontaneously within 2 years. However CIN II and CIN III (high grade CINs) can develop into cervical cancer if the high-risk HPV infection persists (Bosch et al. 2008). Therefore, it is important to detect precancerous cells in the primary screening. However, the sensitivity of the current Pap test for detecting abnormal precursor cells is relatively low: the mean sensitivity for CINs is suggested to be 51% (Litjens et al. 2013). The results of the Pap test are affected by sampling conditions and physicians’ interpretations because the test depends on visual inspection (Wentzensen et al. 2007). Therefore, the development of a method that is more objective and potentially standardized is a high priority.
Since the 1980s researchers have sought to develop protein-based biomarkers for detecting and monitoring cancers. It has been suggested that particular proteins termed tumor-associated proteins (TAPs) are overexpressed, modified, mutated or degraded during carcinogenesis (Anderson et al. 2005). Therefore, detection of these TAPs could increase the chance of detecting cancers and cancerous lesions. Among TAPs, Sialyllewis A (SLeA), p53, heat shock proteins (Hsps), Cancer Antigen 15-3 (CA 15-3) and squamous cervical carcinoma antigen (SCCA) have received much attention as potential biomarkers. SLeA is a carbohydrate ligand on cells; it is involved in interactions with E-selectin on vascular endothelial cells, and plays a major role in cancer cell metastasis and invasion (Kannagi et al. 2004). Blood SLeA levels increase in patients with pancreatic cancer, and urinary SLeA increases in patients with bladder cancer (Casetta et al. 1993; Duffy 1998; Ballehaninna et al. 2011). P53 is a well-known tumor suppressor protein. In response to DNA damage, it activates a molecular defense against carcinogenesis, stimulating DNA repair and inducing the death of mutated cell (Bhatt et al. 2010). Elevated levels of p53 are indeed found in a breast cancer cell line (MCF 7) (Alkhalaf et al. 2003).
Hsp expression is a tailored response to particular microenvironmental stresses (low glucose, change of pH, and viral and bacterial infections) (Zugel et al. 1999; Bhatt et al. 2010). Increased levels of Hsp70 (molecular weight: 70 kDa) are presented in sera from breast, lung and colorectal cancers and increased levels of Hsp27 (molecular weight: 27 kDa) are found in sera from breast, ovarian and endometrial cancers (De et al. 2004; Gunaldi et al. 2015a, b; Balazs et al. 2016).
CA 15-3 is a cell surface glycoprotein involved in cancer cell migration and metastasis (Bhatt et al. 2010). Blood CA 15-3 levels have been used to assess the prognosis of breast cancer, and increased levels of CA 15-3 are also found in lung, ovarian and colorectal cancers (Shering et al. 1998; Bhatt et al. 2010). Elevated SCCA level was suggested as serological marker in cervical carcinoma (Catanzaro et al. 2011). However, few studies have been conducted to assess whether these TAP can be used as biomarker of ECC for primary screening of cervical cancer.
Unlike other types of cancer, the causes of which vary, cervical cancer is invariably caused by HPV infection. Therefore, the presence of HPV proteins provides critical evidence for a risk of cervical cancer. The expression of the HPV E7 oncoprotein mainly starts in the basal layer cells of the cervical squamous epithelium and is maintained in the superficial layer (Litjens et al. 2013), and HPV L1 is mainly expressed in the superficial layer (Yemelyanova et al. 2013). Therefore, it is thought that the superficial layer cells may reflect the cancerous state of the cervix. However, there has been little effort to evaluate levels of HPV proteins in ECCs and no attempts to use them as biomarkers of ECCs.
In this study we measured the levels of six TAPs (SLeA, p53, Hsp70, Hsp27, CA 15-3 and SCCA) and two HPV proteins (HPV16 E7 and HPV16 L1) in the cytoplasmic fraction of ECCs using enzyme-linked immunosorbent assays (ELISAs), and assessed the possibility of using these proteins as biomarkers for primary screening of cervical cancer.
Materials and Methods
Ethics statement
This study was conducted with the approval of the Institutional Review Board of EwhaWomans University Mokdong Hospital (Approval No. EUMC 2016-07-067-002). Patients’ samples were collected in a prospective and consecutive manner after obtaining written informed consents.
Specimens
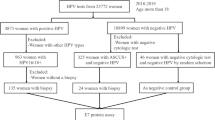
A total of 146 ECC samples from liquid-based cytology (LBC) were collected from women with normal cytology (n = 30), CIN I (n = 28), CIN II (n = 33), CIN III (n = 32) and cervical cancer (n = 23) with a Thinprep 2000 liquid-based cytology processor (Hologic, USA). All of the samples were collected under colposcopy-directed biopsy setting by three different gynecology oncology specialists. Cervical lesions were graded by hematoxylin and eosin (H&E) staining review.
Preparation of soluble factions of ECC lysates
The ECCs were washed gently once with ice cold phosphate-buffered saline (PBS) and suspended in lysis buffer (150 mM NaCl, 50 mM Tris, 1% Triton X-100, pH 7.2), then incubated on ice for 2 h. Thereafter, they were disrupted with a Dounce homogenizer (Wheaton, USA), and the lysates were incubated on ice for an additional 1 h. Finally, supernatants were collected after centrifugation at 14,000 rpm for 10 min at 4 °C. Protein concentrations were determined with a BCA protein assay kit (Pierce, USA).
Enzyme-linked immunosorbent assays (ELISAs)
96-well ELISA plates (Greiner, Germany) were coated overnight at 4 °C with optimum amounts of cell lysate [30 ng for ELISA-SLeA; 500 ng for ELISAs-p53, Hsp70, CA 15-3, HPV16 L1and SCCA; 250 ng for ELISA-Hsp27; 62.5 ng for ELISA-HPV16 E7]. The plates were blocked with 5% skim milk at room temperature (RT) for 2 h. Then mouse anti-SLeA monoclonal antibody (Millipore, MAB2095, USA, 1:10,000 dilution), mouse anti-p53 monoclonal antibody (Sigma,P6749, USA, 1:5000), mouse anti-Hsp70 monoclonal antibody (Fitzgerald, 10R-1046, USA, 1:2500), mouse anti-CA 15-3 monoclonal antibody (Fitzgerald, 10-C03E, USA, 1:3000), mouse anti-Hsp27 monoclonal antibody (Enzo, ADI-SPA-800, USA,1:2500), mouse anti-SCCA1/2 monoclonal antibody (Santacruz, sc-28384, USA, 1:1000), mouse anti-HPV16 E7 polyclonal antibody (in-house made antibody; 1:10,000) or mouse anti-HPV16 L1 monoclonal antibody (in-house made antibody; 1:20) were added to the wells and incubated for 90 min at 37 °C. Finally, antibodies bound to the antigens were detected with HRP-conjugated goat anti-mouse IgG (Bethyl, USA, 1:5,000). Color reactions were developed using o-phenylenediamine (Sigma, USA), and measured at 492 nm.
Evaluation of the linearity and reproducibility of ELISAs
To analyze the linearity of the ELISAs, ECC lysates from normal (n = 5) and cancer (n = 5) samples were diluted serially (two-fold) from 5 to 0.07 µg/ml (ELISA-SLeA), 10–0.16 µg/ml (ELISA-p53, HPV16 E7 and HPV16 L1) and 5–0.16 µg/ml (ELISA-Hsp70, CA 15-3, Hsp27and SCCA), respectively. 96-well plates were coated overnight with 100 µL of the serial dilutions at 4 °C, and candidate protein levels were measured as described above.
Western blots for detecting SLeA
Samples of ECC lysates were fractionated on 12.5% polyacrylamide gels and the proteins were visualized by silver staining. The same samples were separated on 10% polyacrylamide gels and transferred onto polyvinylidene difluoride (PVDF) membranes (Millipore, USA). The membranes were blocked with 5% skim milk in Tris-buffered saline (TBS) containing 0.05% Tween 20 (TBST) for 2 h and reacted with mouse anti-SLeA monoclonal antibody (Millipore,1:10,000) for 1 h at RT. The membranes were then incubated with HRP-conjugated goat anti-mouse IgG (1:5000) and developed on X-ray film (Kodak, USA) using an enhanced chemiluminescence kit (Abclon, Korea).
Immunoprecipitation of protein carrying SLeA from ECC lysates
Immunoprecipitation was conducted using protein A agarose beads (10 µl, Sigma, USA) coupled with mouse anti-SLeA monoclonal antibody (Fitzgerald, 2 µg) from normal or cancer cell lysate (500 µg). SLeA levels in immunoprecipitates were detected with mouse anti-SLeA monoclonal antibody (1:50,000) followed by HRP-conjugated goat anti-mouse IgG(1:10,000) in Western blot.
Statistical analysis
Differences between groups were analyzed using two-tailed Student’s t-tests. P < 0.05 was considered statistically significant. Receiver operating characteristic (ROC) curves and areas under the curves (AUCs) were obtained using Graphpad version 5.01. The sensitivity and specificity of each assay were determined from the ROC curves. The optimum cut-off values were obtained from the Youden’s index of the ROC curves, which elicit the maximum values of sensitivity plus specificity. For the combination assays, the logistic regressions were performed using ‘Bia-reduced logistic regression version 1-1.23-r7′ (http://www.wessa.net/) software. Negative predictive values (NPV), positive predictive values (PPV) and accuracies were calculated using EPR-Val Test Pack 2 (http://www.hutchon.net/EPRval.htm). Statistical power (1-β error) was calculated using the G*power 3.1 program.
Results
Clinicopathological characteristics of normal, CIN I, CIN II, CIN III and cancer groups
As shown in Table 1, the mean age of normal, CIN I, CIN II, CIN III and cancer patients were 48.1, 40.2, 44.2, 37.8 and 51.0 years, respectively. HPV16 DNA positivities of those were 6.7, 16.0, 23.1, 44.8 and 37.5%, respectively. Moreover, the proportion of squamous cell carcinomas in the cancer group was 78.3% and that of adenocarcinomas was 21.7%.
Determination of amount of ECC lysate protein to use for coating in ELISAs
The linearity of each ELISA as a function of the amount of ECC lysate protein used for coating was assessed and the optimum amount for each ELISA was determined based on the linear phase of the response. As shown in Fig. 1, linear responses in the ELISA-SLeA, ELISA-HPV16 E7, ELISA-p53, ELISA-HPV16 L1, ELISA-Hsp70, ELISA-Hsp27, ELISA-CA 15-3 and ELISA-SCCA were observed in the ranges of 15–250, 16–1000, 31–500, 62.5–1000, 16–500, 31–250, 16–500, 16–500 ng/well, respectively.
Evaluation of the linearity of ELISAs. Details are given in Materials and Methods. Vertical dotted lines indicate the ranges of the calculated R2 values. Data are means ± SDs of five individual samples of the normal and cancer groups. Blue lines indicate normal group, and red lines cancer group. (Normal, n = 5; Cancer, n = 5). (Color figure online)
Levels of candidate proteins in the normal, CIN I, CIN II, CIN III and cervical cancer groups
As shown in Fig. 2, SLeA levels in the cervical cancers were significantly lower than in the normal, CIN I, CIN II or CIN III group whereas HPV16 E7, p53 or HPV16 L1 levels in the cancer group were considerable higher than in the other groups. Moreover, the SLeA, HPV16 E7, p53 or HPV16 L1 levels seemed useful for discriminating cervical cancer from CIN III, because of the marked changes in levels of these proteins in cervical cancer. In addition, Hsp70, Hsp27 and CA 15-3 tended to increase in the CIN I, CIN II, CIN III and cancer groups, compared to normal group. SCCA elevated only in cancer group.
Comparison of biomarker candidate levels in the normal, CIN I, CIN II, CIN III and cancer groups. Biomarker candidate levels were measured by ELISA as described in Materials and Methods. The central lines are medians, and the top and bottom lines refer to 75th and 25th percentiles, respectively. Normal, n = 30; CIN I, n = 28; CIN II, n = 33; CIN III, n = 32; Cancer n = 23. (*P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001; red asterisks indicate significance differences between the normal group and other groups.). (Color figure online)
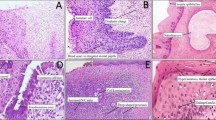
The decrease in SLeA level of cell lysates or immunoprecipitates with increasing severity of lesion was confirmed by Western blots (Fig. 3). The mean values of the coefficient variations (CVs) for inter-and intra-assay precision of each assay were < 10%, indicating satisfactory reproducibility (Supplementary Table S1).
Western blot analysis of SLeA levels. Three micrograms of cell lysate protein from the normal and cancer groups were loaded per well for SDS-PAGE (a), and 150 ng samples were loaded for Western blot to detect SLeA levels (b). Normal, n = 5; Cancer, n = 5. Mixtures of cell lysates from 20 individual samples were loaded for Western blot (c). Native SLeA (purified from a human colon adenocarcinoma cell line, Fitzgerald, USA) was used as positive control. The results show that Hela cells (a cervical cancer cell line) as well as ECCs from cervical cancers have considerably reduced SLeA levels. The reduced SLeA level in Hela cells supports our findings. The decreased SLeA level was also confirmed by immunoprecipitation followed by Western blot for detecting SLeA. Mixture of cell lysates was prepared from 10 individual samples from normal or cancer. Mouse anti-SLeA monoclonal IgG, 1% input of the mixture and 10% of its immunoprecipitates were loaded for Western blot (d). Anti-SLeA antibody dilution ratio: 1:10,000 for panel B and C; 1:50,000 for panel D
Evaluation of ELISAs for discriminating the CIN I+, CIN II+, CIN III+ and cancer groups from the normal group
The P-values, AUCs, sensitivities and specificities of the individual ELISAs were analyzed for their ability to discriminate between CIN I and worse (CIN I+), CIN II+, CIN III+and the actual cancer from the normal group (Table 2). AUC values, sensitivities and specificities were determined based on the ROC curve for each ELISA.
An AUC value > 0.6 is usually taken as acceptable for diagnosis (Fielding AH 1997). The AUC values of ELISA-SLeA and ELISA-HPV16 L1 were effective in discriminating CIN I+, CIN II+, CIN III+ and cervical cancer from normal, while ELISA-HPV16 E7 and ELISA-p53 could discriminate CIN III+ and cancer from normal, andELISA-Hsp70, ELISA-Hsp27 and ELISA-CA 15-3 were useful for discriminating cancer from normal.
Combination assays for distinguishing the CIN I+, CIN II+, CIN III+ and cancer groups from the normal group
Combination assays were conducted using logistic regression, the abilities of pairs of ELISA assays to discriminate cervical lesions from normal were assessed.
The combination of ELISA-SLeA and ELISA-HPV16 L1 had improved ability to discriminate CIN I+, CIN II+ or CIN III+ from normal, and the relevant statistical parameters are presented in Table 3. In addition, the combination of ELISA-SLeA and ELISA-p53 had increased sensitivity and specificity for discriminating cancer from normal. The power values (1-β) of all the combination assays exceeded 0.90, indicating that the sample sizes used supported statistical reliability. Moreover, the AUC values of the combination assays and the ROC curves are presented in Fig. 4. Taken together, these results indicate that the combination assays are more useful for discriminating patients with CIN I+, CIN II+, CIN III+ and cervical cancer from normal than the individual assays.
ROC curves of combination assays to discriminate CIN I+, CIN II+, CIN III+ and cancer samples from normal samples. ROC curves are shown for the combination of ELISA-SLeA and ELISA-HPV16 L1 to discriminate CIN I+from normal (a), CIN II+ from normal (b) and CIN III+ from normal (c). Panel D is a ROC curve for the combination of ELISA-SLeA and ELISA-p53 to discriminate the cancer group from the normal group (d)
Discussion
We have investigated the use of eight ECC proteins as biomarkers for primary screening of cervical cancer. SLeA, HPV16 L1 and p53 levels were more suitable for detecting cervical lesions than the other candidates (Table 2). The combination of ELISA-SLeA and ELISA-HPV16 L1 was found to discriminate cervical lesions from the normal group efficiently (Table 3). Moreover the combination of ELISA-SLeA and ELISA-p53 discriminated the cancer group from normal with 91.3% sensitivity and 96.7% specificity (Table 3).
We found that SLeA decreased with increasing severity of the cervical lesions (Fig. 2a), whereas increased SLeA levels have been reported in colon and breast cancer tissues (Renkonen et al. 1997; Matsui et al. 2004) and in the squamous epithelium of cervical cancer (Engelstaedter et al. 2012). Therefore, the trend of SLeA in the ECCs was contrary to previous results. Creuzot-Garcher et al. found reduced SLeA levels in pterygium tissue compared to normal conjunctiva and suggested that this was due to reduced Galb1-3GlcNAc a2,3-sialyltransferase (ST3Gal III) levels in the pterygium tissue. Furthermore, they found that SLeA was mainly located in the superficial layer of normal conjunctive tissue but in the deep layer of pterygium epithelium (Creuzot-Garcher et al. 1999). Thus, the SLeA distribution may differ according to tissue layer. The SLeA distribution in different cervical tissue layers needs to be investigated. Meanwhile a protein carrying SLeA of 180–245 kDa was found in immunoprecipitates and detected by Western blotting (Fig. 3d). The SLeA level appeared to be markedly reduced in cervical cancer (Supplementary Fig. S1A) although there was no difference in banding patterns between normal and cancer on SDS-PAGE as visualized by silver staining (Supplementary Fig. S1B). Therefore, it is likely that the reduced level of SLeA in cancer is caused by a reduced level of SLeA structures on the carrier protein, rather than a reduced amount of the protein carrying SLeA (Supplementary Fig. S1).
HPV L1 is expressed during the maturation of basal cells into the superficial layer cells of cervix tissue, and may therefore be mainly found in the superficial layer (Yemelyanova et al. 2013; Lee et al. 2014). One study suggested that HPV L1 is located in the cytoplasm as well as the nuclei of cells of the superficial cervix tissue in cervical cancers (Lee et al. 2008), and others found that HPV was mainly located in the cytoplasm of the superficial layer cells in cervical cancer patients (Hernandez et al. 2011). Therefore we hypothesize that the HPV16 L1 levels of the cytoplasm of the superficial layer cells of the cervix may increase with the increasing severity of cervical lesions. HPV16 L1 appeared to be the most effective biomarker for discriminating CINs and cervical cancer from normal or cervical cancer from CINs (Table 2; Fig. 2d). Our results indicate that L1 protein level in the cytoplasmic fraction faithfully reflects the severity of cervical lesion (Fig. 2d).
Previous studies showed that p53 is overexpressed in cervical cancer tissue (Bremer et al. 1995; Dimitrakakis et al. 2000; Zhou et al. 2015). In the present study, p53 levels in the cytoplasmic fractions of superficial cervical layer cells increased with increasing stage of the cervical lesions (Fig. 2c). Therefore, it appears that the enhanced p53 levels in the basal layer cells of cervical neoplasias and cancers are also reflected in the superficial layers.
E7 protein, an oncoprotein of HPV, plays a major role in malignant transformation (Yim et al. 2005). The expression of E7 increases as a function of the severity of cervical lesions because integration of the gene into the host genome in high grade CIN stabilizes its expression (Narisawa-Saito et al. 2007). Previously, a study showed that integration of the HPV 16 gene increased with stage of cervical lesion (Li et al. 2008). The substantial increase of E7 protein in in ECCs in CIN III and cervical cancer in this study is consistent with previous suggestions (Fig. 2b).
Both Hsp27 and Hsp70 increased in low grade CIN as well as in high grade CIN and cervical cancer (Fig. 2e, f). The expression of heat shock proteins is closely related to virus infection because infection induces cellular stress (Zugel et al. 1999). And the heat shock responses primarily act to trigger the immune system (Merkling et al. 2015). Therefore, we supposed that Hsp27 and Hsp70 levels may increase even in early stages of cervical cancers, and the Hsp levels observed agrees with that idea (Fig. 2e, f).
CA 15-3 is a member of the mucin family involved in cancer cell proliferation and metastasis (Bhatt et al. 2010; Nath et al. 2014). In our study, an increased CA 15-3 level was found in the CIN I group (Fig. 2g). Therefore, CA 15-3 expression is sensitive to cervical lesions even though CIN I has almost no relation to metastasis. Expression of the mucin-type carbohydrate antigen Tn in cervix tissue is in the increasing order normal, CIN III and cervical cancer groups (Carrilho et al. 2000). These findings suggest the members of the mucin family could be potential biomarkers for cervical cancer screening.
In our study, an elevated SCCA level of cytoplasmic fractions of superficial cervix layer was found in cervical cancer group (Fig. 2h). Diaconu et al. also found increased SCCA levels not only in superficial layer but also in suprabasal layers in the basal cell carcinoma (Diaconu et al. 2007). Therefore, our result is consistent with that of Diaconu et al.
During the past two decade researchers have tried to develop new biomarkers while the majority of these biomarkers were discovered in histological samples and although they detect cervical cancer with high accuracy (Litjens et al. 2013) they are not suitable for primary screening for several reasons: sample collection causes patient stress, they are inaccurate and cannot cope with large numbers of sample and they need costly equipment. We expected that protein biomarkers from ECCs would be suitable for primary screening of cervical cancer because ECCs are easy to sample and can be used in a variety of molecular assays (Davey et al. 2006; Arbyn et al. 2008). Moreover, we thought that ECCs might reflect cellular changes during cervical carcinogenesis, because ECCs are derived from cells of the superficial layer that have migrated from the basal layer (Steinau et al. 2005). In this study, the simple format of ELISA was used to enhance the use of ECCs and it is also easy to standardize because results can be expressed numerically. It is likely that the accuracy of the ELISAs developed in this study could be increased by using precise cut-off values and that they could be validated in further studies.
The goal of primary screening of cervical cancer is to discriminate CIN II+ patients from normal patients. Because almost 90% of CIN I regresses within 2 years, treatment is recommended for CIN II+ cases (Litjens et al. 2013). Therefore, the ability of each candidate to discriminate between the (normal + CIN I) group and the CIN II+ group was also assessed (Supplementary Table S2). The values of Youden’s Index and AUCs indicated that SLeA and HPV16 L1 were the most promising markers for discriminating the CIN II+group from the control (normal + CIN I) group. Both markers were also found to be the most powerful markers for discriminating the CIN I+, CIN II+, CIN III+ and cancer groups from the normal group (Table 2). Therefore it appears that SLeA and HPV16 L1 may be useful in clinical application.
The rates of HPV16 DNA positivity in low-grade squamous intraepithelial lesions (LSIL) and high grade intraepithelial lesions (HSIL) have been reported to be 25.1 and 47.5%, respectively (Guan et al. 2012), and positive rates for HPV16 L1 protein in the cervical tissue of LSIL and HSIL patients were found to be 74 and 52%, respectively (Uranbolor Jugder 2015). These findings indicate that HPV viral proteins as well as HPV DNA could be useful for detecting cervical lesions. HPV16 L1 and HPV16 E7 levels in the HPV16 DNA positive group and HPV16 DNA negative group (other types of HPV DNA positives) are compared in Supplementary Figure S2). The levels of HPV viral proteins were compared in the high grade CIN, cancer and CIN II+ groups, and elevated levels of HPV16 L1 and HPV16 E7 were found not only in the HPV16 DNA positive group but also in the “other types of HPV DNA positive group”. It has been suggested that the antibody against HPV16 L1 has cross-reactivity towards HPV11, HPV31, HPV33, HPV52 or HPV58 L1, and that the antibody against HPV16 E7 also has cross-reactivity towards HPV31, HPV33, HPV35 or HPV58 (Scherpenisse et al. 2013; Combes et al. 2014). Therefore, it is likely that this cross-reactivity is responsible for the high apparent rate of detection of HPV16 viral proteins. It has been reported that the use of multiple high risk types of HPV DNA increases the sensitivity of detection of cervical lesions compared with using a single type of HPV DNA (Agorastos et al. 2015). Therefore, simultaneous testing for several HPV viral proteins is expected to increase the sensitivity and specificity of detection of cervical lesions.
Although just eight candidates were used in the present study, most of them showed considerable potential as biomarkers. Therefore, it is expected that ECCs contain many more potential candidate proteins. We suggest that care should be taken to record any changes in protein levels in ECCs as a basis for discovering new biomarkers for cervical cancer.
References
Agorastos T, Chatzistamatiou K, Katsamagkas T, Koliopoulos G, Daponte A, Constantinidis T, Constantinidis TC (2015) Primary screening for cervical cancer based on high-risk human papillomavirus (HPV) detection and HPV 16 and HPV 18 genotyping, in comparison to cytology. PLoS ONE 10:e0119755
Alkhalaf M, El-Mowafy AM (2003) Overexpression of wild-type p53 gene renders MCF-7 breast cancer cells more sensitive to the antiproliferative effect of progesterone. J Endocrinol 179:55–62
Anderson KS, LaBaer J (2005) The sentinel within: exploiting the immune system for cancer biomarkers. J Proteome Res 4:1123–1133
Arbyn M, Bergeron C, Klinkhamer P, Martin-Hirsch P, Siebers AG, Bulten J (2008) Liquid compared with conventional cervical cytology: a systematic review and meta-analysis. Obstet Gynecol 111:167–177
Balazs M, Zsolt H, Laszlo G, Gabriella G, Lilla T, Gyula O, Balazs D, Eva M, Zoltan B, Zoltan P and Judit K (2016) Serum Heat Shock Protein 70, as a Potential Biomarker for Small Cell Lung Cancer. Pathol Oncol Res
Ballehaninna UK, Chamberlain RS (2011) Serum CA 19-9 as a Biomarker for Pancreatic Cancer-A Comprehensive Review. Indian J Surg Oncol 2:88–100
Bhatt AN, Mathur R, Farooque A, Verma A, Dwarakanath BS (2010) Cancer biomarkers—current perspectives. Indian J Med Res 132:129–149
Bosch FX, Burchell AN, Schiffman M, Giuliano AR, de Sanjose S, Bruni L, Tortolero-Luna G, Kjaer SK, Munoz N (2008) Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine 26(Suppl 10):K1–16
Bremer GL, Tieboschb AT, van der Putten HW, de Haan J, Arends JW (1995) p53 tumor suppressor gene protein expression in cervical cancer: relationship to prognosis. Eur J Obstet Gynecol Reprod Biol 63:55–59
Carrilho C, Cantel M, Gouveia P, David L (2000) Simple mucin-type carbohydrate antigens (Tn, sialosyl-Tn, T and sialosyl-T) and gp 230 mucin-like glycoprotein are candidate markers for neoplastic transformation of the human cervix. Virchows Arch 437:173–179
Casetta G, Piana P, Cavallini A, Vottero M, Tizzani A (1993) Urinary levels of tumour associated antigens (CA 19-9, TPA and CEA) in patients with neoplastic and non-neoplastic urothelial abnormalities. Br J Urol 72:60–64
Catanzaro JM, Guerriero JL, Liu J, Ullman E, Sheshadri N, Chen JJ, Zong WX (2011) Elevated expression of squamous cell carcinoma antigen (SCCA) is associated with human breast carcinoma. PLoS ONE 6:e19096
Combes JD, Pawlita M, Waterboer T, Hammouda D, Rajkumar T, Vanhems P, Snijders P, Herrero R, Franceschi S, Clifford G (2014) Antibodies against high-risk human papillomavirus proteins as markers for invasive cervical cancer. Int J Cancer 135:2453–2461
Creuzot-Garcher C, Guerzider V, Assem M, Bron AM, Delannoy P, Bara J (1999) Alteration of sialyl Lewis epitope expression in pterygium. Invest Ophthalmol Vis Sci 40:1631–1636
Davey E, Barratt A, Irwig L, Chan SF, Macaskill P, Mannes P, Saville AM (2006) Effect of study design and quality on unsatisfactory rates, cytology classifications, and accuracy in liquid-based versus conventional cervical cytology: a systematic review. Lancet 367:122–132
De AK, Roach SE (2004) Detection of the soluble heat shock protein 27 (hsp27) in human serum by an ELISA. J Immunoassay Immunochem 25:159–170
Diaconu NC, Kaminska R, Naukkarinen A, Harvima RJ, Harvima IT (2007) The increase in tryptase- and chymase-positive mast cells is associated with partial inactivation of chymase and increase in protease inhibitors in basal cell carcinoma. J Eur Acad Dermatol Venereol 21:908–915
Dimitrakakis C, Kymionis G, Diakomanolis E, Papaspyrou I, Rodolakis A, Arzimanoglou I, Leandros E, Michalas S (2000) The possible role of p53 and bcl-2 expression in cervical carcinomas and their premalignant lesions. Gynecol Oncol 77:129–136
Duffy MJ (1998) CA 19-9 as a marker for gastrointestinal cancers: a review. Ann Clin Biochem 35(Pt 3):364–370
Engelstaedter V, Fluegel B, Kunze S, Mayr D, Friese K, Jeschke U, Bergauer F (2012) Expression of the carbohydrate tumour marker Sialyl Lewis A, Sialyl Lewis X, Lewis Y and Thomsen-Friedenreich antigen in normal squamous epithelium of the uterine cervix, cervical dysplasia and cervical cancer. Histol Histopathol 27:507–514
Fielding AHBJ (1997) A review of methods for the assessment of prediction errors in conservation presence/absence models. Environ Conserv 24:38–49
Ghittoni R, Accardi R, Chiocca S, Tommasino M (2015) Role of human papillomaviruses in carcinogenesis. Ecancermedicalscience 9:526
Guan P, Howell-Jones R, Li N, Bruni L, de Sanjose S, Franceschi S, Clifford GM (2012) Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer 131:2349–2359
Gunaldi M, Afsar CU, Okuturlar Y, Gedikbasi A, Kocoglu H, Kural A, Akarsu C, Gunduz U, Tiken EE (2015a) Elevated serum levels of heat shock protein 70 are associated with breast cancer. Tohoku J Exp Med 236:97–102
Gunaldi M, Kocoglu H, Okuturlar Y, Gedikbasi A, Karabulut M, Alis H, Hursitoglu M (2015b) Heat shock protein 70 is a useful marker for predicting colorectal cancer. J BUON 20:1464–1470
Habis AH, Vernon SD, Lee DR, Verma M, Unger ER (2004) Molecular quality of exfoliated cervical cells: implications for molecular epidemiology and biomarker discovery. Cancer Epidemiol Biomarkers Prev 13:492–496
Hernandez J, Elahi A, Siegel E, Coppola D, Riggs B, Shibata D (2011) HPV L1 capsid protein detection and progression of anal squamous neoplasia. Am J Clin Pathol 135:436–441
Kannagi R, Izawa M, Koike T, Miyazaki K, Kimura N (2004) Carbohydrate-mediated cell adhesion in cancer metastasis and angiogenesis. Cancer Sci 95:377–384
Lee H, Lee KJ, Jung CK, Hong JH, Lee YS, Choi YJ, Lee KY, Park G (2008) Expression of HPV L1 capsid protein in cervical specimens with HPV infection. Diagn Cytopathol 36:864–867
Lee SJ, Lee AW, Kang CS, Park JS, Park DC, Ki EY, Lee KH, Yoon JH, Hur SY, Kim TJ (2014) Clinicopathological implications of human papilloma virus (HPV) L1 capsid protein immunoreactivity in HPV16-positive cervical cytology. Int J Med Sci 11:80–86
Li W, Wang W, Si M, Han L, Gao Q, Luo A, Li Y, Lu Y, Wang S, Ma D (2008) The physical state of HPV16 infection and its clinical significance in cancer precursor lesion and cervical carcinoma. J Cancer Res Clin Oncol 134:1355–1361
Litjens RJ, Hopman AH, van de Vijver KK, Ramaekers FC, Kruitwagen RF, Kruse AJ (2013) Molecular biomarkers in cervical cancer diagnosis: a critical appraisal. Expert Opin Med Diagn 7:365–377
Matsui T, Kojima H, Suzuki H, Hamajima H, Nakazato H, Ito K, Nakao A, Sakamoto J (2004) Sialyl Lewisa expression as a predictor of the prognosis of colon carcinoma patients in a prospective randomized clinical trial. Jpn J Clin Oncol 34:588–593
Merkling SH, Overheul GJ, van Mierlo JT, Arends D, Gilissen C, van Rij RP (2015) The heat shock response restricts virus infection in Drosophila. Sci Rep 5:12758
Mishra GA, Pimple SA, Shastri SS (2011) An overview of prevention and early detection of cervical cancers. Indian J Med Paediatr Oncol 32:125–132
Narisawa-Saito M, Kiyono T (2007) Basic mechanisms of high-risk human papillomavirus-induced carcinogenesis: roles of E6 and E7 proteins. Cancer Sci 98:1505–1511
Nath S, Mukherjee P (2014) MUC1: a multifaceted oncoprotein with a key role in cancer progression. Trends Mol Med 20:332–342
Renkonen J, Paavonen T, Renkonen R (1997) Endothelial and epithelial expression of sialyl Lewis(x) and sialyl Lewis(a) in lesions of breast carcinoma. Int J Cancer 74:296–300
Sahasrabuddhe VV, Luhn P, Wentzensen N (2011) Human papillomavirus and cervical cancer: biomarkers for improved prevention efforts. Future Microbiol 6:1083–1098
Scherpenisse M, Schepp RM, Mollers M, Meijer CJ, Berbers GA, van der Klis FR (2013) Characteristics of HPV-specific antibody responses induced by infection and vaccination: cross-reactivity, neutralizing activity, avidity and IgG subclasses. PLoS ONE 8:e74797
Shering SG, Sherry F, McDermott EW, O’Higgins NJ, Duffy MJ (1998) Preoperative CA 15-3 concentrations predict outcome of patients with breast carcinoma. Cancer 83:2521–2527
Simayi D, Yang L, Li F, Wang YH, Amanguli A, Zhang W, Mohemaiti M, Tao L, Zhao J, Jing MX, Wang W, Saimaiti A, Zou XG, Maimaiti A, Ma ZP, Hao XL, Duan F, Jing F, Bai HL, Liu Z, Zhang L, Chen C, Cong L, Zhang X, Zhang HY, Zhan JQ, Zhang WJ (2013) Implementing a cervical cancer awareness program in low- income settings in Western China: a community-based locally affordable intervention for risk reduction. Asian Pac J Cancer Prev 14:7459–7466
Snijders PJ, Steenbergen RD, Heideman DA, Meijer CJ (2006) HPV-mediated cervical carcinogenesis: concepts and clinical implications. J Pathol 208:152–164
Steinau M, Lee DR, Rajeevan MS, Vernon SD, Ruffin MT, Unger ER (2005) Gene expression profile of cervical tissue compared to exfoliated cells: impact on biomarker discovery. BMC Genom 6:64
Uranbolor Jugder ED, Galtsog Lodon, Jav Baldan, Sarantuya Jav (2015) The Detection of Human Papillomavirus 16 and 18 Type L1 Capsid Protein in Cervical Lesion Specimens Among Mongolian Women. Centeral Asian Journal of Medical Sciences November 1 (1) 56–59
Wentzensen N, von Knebel Doeberitz M (2007) Biomarkers in cervical cancer screening. Dis Markers 23:315–330
Williams GH, Romanowski P, Morris L, Madine M, Mills AD, Stoeber K, Marr J, Laskey RA, Coleman N (1998) Improved cervical smear assessment using antibodies against proteins that regulate DNA replication. Proc Natl Acad Sci U S A 95:14932–14937
Yemelyanova A, Gravitt PE, Ronnett BM, Rositch AF, Ogurtsova A, Seidman J, Roden RB (2013) Immunohistochemical detection of human papillomavirus capsid proteins L1 and L2 in squamous intraepithelial lesions: potential utility in diagnosis and management. Mod Pathol 26:268–274
Yim EK, Park JS (2005) The role of HPV E6 and E7 oncoproteins in HPV-associated cervical carcinogenesis. Cancer Res Treat 37:319–324
Zhou R, Wei C, Liu J, Luo Y, Tang W (2015) The prognostic value of p53 expression for patients with cervical cancer: a meta analysis. Eur J Obstet Gynecol Reprod Biol 195:210–213
Zugel U, Kaufmann SH (1999) Role of heat shock proteins in protection from and pathogenesis of infectious diseases. Clin Microbiol Rev 12:19–39
Acknowledgements
The present study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI12C0050). URL: https://www.htdream.kr/.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no competing interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jin, Y., Kim, S.C., Kim, H.J. et al. Use of protein-based biomarkers of exfoliated cervical cells for primary screening of cervical cancer. Arch. Pharm. Res. 41, 438–449 (2018). https://doi.org/10.1007/s12272-018-1015-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-018-1015-5