Abstract
Rhinoviral infection is associated with an increased risk of asthma attacks. The macrolide clarithromycin decreases cytokine production in nasopharyngeal aspirates from patients with wheezing, but the effects of macrolides on cytokine production in nasal epithelial cells obtained from asthmatic subjects remain unclear. Here, human nasal epithelial cells were infected with type-14 rhinovirus (RV14), a major RV group. Titers and RNA of RV14 and cytokine concentrations, including IL-1β and IL-6, were higher in the supernatants of the cells obtained from subjects with bronchial asthma (asthmatic group) than in those from the non-asthmatic group. Pretreatment with clarithromycin decreased RV14 titers, viral RNA and cytokine concentrations, and susceptibility to RV14 infection. Pretreatment with clarithromycin also decreased IL-33 production, which was detected after infection. Pretreatment with clarithromycin decreased the expression of intercellular adhesion molecule-1, the receptor for RV14, after infection, the number and fluorescence intensity of the acidic endosomes through which RV RNA enters the cytoplasm, and the activation of nuclear factor kappa-B proteins in nuclear extracts. These findings suggested that RV replication and cytokine production may be enhanced in nasal epithelial cells obtained from subjects with bronchial asthma and may be modulated by clarithromycin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rhinovirus (RV) infection is a major cause of exacerbation of bronchial asthma, and it induces frequent and long periods of lower airway symptoms in adult asthmatics (Nicholson et al. 1993; Johnston et al. 1995; Corne et al. 2002; Yamaya 2012a). Several events induced by RV infection have been suggested to be associated with the exacerbation of bronchial asthma, including increased airway responsiveness, eosinophil accumulation in airways, increases in smooth muscle contraction and mucus secretion (Lemanske et al. 1989; Fraenkel et al. 1995; Inoue et al. 2006). Furthermore, a higher frequency of colds in asthmatic adults and a higher detection rate of RV in asthmatic children with symptoms of a cold have been reported (Minor et al. 1974; Tarlo et al. 1979).
RV infection-induced cytokines, such as IL-5, IL-13, IL-25 and IL-33, are associated with persistent and severe asthma (Jackson et al. 2014; Beale et al. 2014). IL-1β and IL-33 enhance intercellular adhesion molecule (ICAM-1) expression in the airway epithelial cells and endothelial cells (Terajima et al. 1997; Demyanets et al. 2011; Choi et al. 2012). Because ICAM-1 is the receptor for the major RV types (Greve et al. 1989), the increased ICAM-1 expression in airway epithelial cells in asthmatic subjects (Wegner et al. 1990; Manolitsas et al. 1994) may cause increased susceptibility to RV infection (Manolitsas et al. 1994).
A variety of drugs decrease the frequency of asthma exacerbation, including inhaled corticosteroids, inhaled corticosteroids and long-acting β2 agonists, leukotriene receptor antagonists and anti-IgE antibodies (Pauwels et al. 1997; Sin et al. 2004; Ohta et al. 2009); however, many patients still have frequent and persistent asthma attacks due to respiratory infections (Wark and Gibson 2006), and they continue to have uncontrolled asthma symptoms despite treatment with inhaled corticosteroids (Bateman et al. 2004). Although antibodies for IL-5 and IL-13 improve lung function in asthmatic patients and decrease asthma exacerbations (Haldar et al. 2009; Corren et al. 2011), further development of agents to decrease asthma exacerbation is required.
Treatment with clarithromycin decreases the frequency of exacerbation in refractory asthma with neutrophilic inflammation (Simpson et al. 2008), improves pulmonary function, and decreases the eosinophil count in peripheral venous blood in children with asthma (Wan et al. 2016). Macrolides have several effects on airway epithelial cells, including inhibiting the replication of respiratory viruses, inhibiting the production of inflammatory cytokines and mucin induced by virus infection (Suzuki et al. 2002; Inoue et al. 2006; Yamaya et al. 2010, 2012b), inhibiting IL-13-induced goblet cell hyperplasia (Tanabe et al. 2011) and stimulating mucociliary transport (Rubin et al. 1997). Furthermore, clarithromycin has been found to decrease cytokine production in the nasopharyngeal aspirates of children with wheezing (Fonseca-Aten et al. 2006) and in sinonasal mucosal explants from patients with eosinophilc and non-eosinophilic chronic rhinosinusitis (Zeng et al. 2015). However, the inhibitory effects of clarithromycin on RV replication and the production of the inflammatory cytokines have not been studied in airway epithelial cells obtained from asthmatic patients.
In the present study, we examined the inhibitory effects of clarithromycin on the type-14 rhinovirus (RV14) infection, RV infection-induced cytokine production and the expression of ICAM-1, the receptor for RV14 (Greve et al. 1989), by using human nasal epithelial (HNE) cells obtained from patients with bronchial asthma.
Materials and methods
Human nasal epithelial cell cultures
The HNE cells were obtained from excised nasal specimens from the coronoid processes of asthmatic (n = 15, age: 45 ± 5 years; 5 females and 10 males, asthmatic group) and non-asthmatic (n = 12, age: 63 ± 3 years; 7 females and 5 males, non-asthmatic group) subjects undergoing endoscopic endonasal sinus surgery. The allergic diseases and the reasons to conduct endoscopic surgery on the subjects are summarized in Table 1.
Among the asthmatic subjects, nine also had chronic sinusitis, four had eosinophilic chronic sinusitis, one had pyogenic granuloma and one had sinus mycosis. The asthmatic subjects also had eosinophilia greater than 500/μL in their peripheral venous blood. The specific serum IgE antibody levels were greater than 170 IU/mL for at least one common inhalant allergen in all of the subjects in the asthmatic group. Bronchial asthma was defined according to the 2015 Global Initiative for Asthma (GINA) guidelines (2015).
The HNE cells were isolated using 0.05% protease, and primary cultures of HNE cells were cultured in plastic tubes (Becton–Dickinson, Franklin Lakes, NJ, USA), in 96-well plates or on coverslips in Petri dishes, as described previously, depending on the experiment (Lusamba Kalonji et al. 2015). We were able to obtain only a limited number of HNE cells, ranging from 3 × 106 to 8 × 106, from specimens from each patient; therefore, the cells were used for the experiments according to the number of isolated cells. We examined the effects of clarithromycin on RV14 proliferation and cytokine production, and then performed experiments to study the mechanisms underlying the inhibitory effects of clarithromycin and to study cell damage. Furthermore, when the cells isolated from the asthmatic patients were used, experiments were performed using the cells obtained from both types of asthmatic patients, i.e., those who had chronic sinusitis and eosinophilic chronic sinusitis, to match the allergic condition associated with the causes of endoscopic surgery.
None of the patients were being treated with oral steroids at the time of surgery. This study was approved by the Tohoku University Ethics Committee (IRB number: 2015-1-730, 2016-1-802).
Human embryonic fibroblast cell culture
Human embryonic fibroblast (HEF) cells (HFL-III cells, Riken Bio Resource Center Cell Bank, Cell No: RCB0523; Tsukuba, Japan) were cultured as previously described (Lusamba Kalonji et al. 2015).
Viral stock
The RV14 (a major RV group) stock was prepared from a patient with a common cold by infecting HEF cells as previously described (Lusamba Kalonji et al. 2015).
Detection and titration of viruses
RV14 in the supernatants (cell-culture medium) was detected and titrated using HEF cells with endpoint methods (Lusamba Kalonji et al. 2015). The rates of RV14 release into the supernatants are expressed as TCID50 (tissue culture infective dose) units/mL (Lusamba Kalonji et al. 2015).
Quantification of rhinoviral RNA
To quantify the RV14 RNA content and β-actin mRNA expression levels in the HNE cells, a two-step real-time quantitative reverse transcription (RT)-PCR assay using the TaqMan technique was performed using TaqMan® Gene Expression Master Mix (Applied Biosystems, Bedford, CA, USA), as previously described (Lusamba Kalonji et al. 2015). RT-PCR for β-actin was also performed as previously described (Lusamba Kalonji et al. 2015). The expression of the RV RNA was normalized to the constitutive expression of the β-actin mRNA.
Viral infection of epithelial cells
Infection of the HNE cells with RV14 (100 μL in each tube, 1.0 × 104 TCID50 units/100 μL, 2.0 × 10−2 TCID50 units/cell) was performed using previously described methods (Lusamba Kalonji et al. 2015). The cells in the tubes were cultured at 33 °C with rolling.
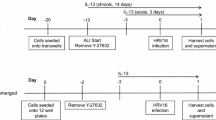
Pretreatment with clarithromycin
HNE cells were pretreated with either clarithromycin (10 μM unless otherwise specified) or vehicle [0.05% dimethyl sulfoxide (DMSO)] for 3 days (72 h) before infection to examine the effects of clarithromycin on RV14 release, RV14 RNA replication, ICAM-1 expression, endosomal acidification, cytokine secretion and NF-κB activation. The concentration of clarithromycin (10 μM) was chosen on the basis of the serum concentration in clinical use (Yamaya et al. 2010). Alternatively, the cells were cultured in medium alone. To examine the effects of clarithromycin on cell functions other than endosomal acidification, the cells were also treated with clarithromycin or the vehicle or cultured in medium alone after RV14 infection until the end of the experimental period.
Collection of the supernatants for measurement
To examine the effects of clarithromycin on viral release, the supernatants were collected at 1 days (24 h), 3 days (72 h) and 5 days (120 h) after infection. In the preliminary experiments, the secretion of IL-6, IL-8 and IL-33 into the supernatants increased 72 h after infection. Therefore, to examine the effects of clarithromycin on the secretion of the inflammatory cytokines, the supernatants were collected before infection and at 72 h after infection.
Effects of clarithromycin on the susceptibility to rhinovirus infection
Epithelial cells were pretreated with clarithromycin (10 μM) or vehicle for 72 h before infection, and the effects of clarithromycin on cellular susceptibility to RV14 infection were evaluated as previously described (Lusamba Kalonji et al. 2015).
Measurement of ICAM-1 expression and cytokine production
The membrane-bound form of ICAM-1 was examined via flow cytometry analysis using an anti-human CD54 antibody and a mouse IgG1, κ isotype control (FC) antibody (BIOLEGEND), as previously described (Suzuki et al. 2002). ICAM-1 mRNA levels were also examined via two-step, real-time, RT-PCR analysis using the methods described above (Quantification of rhinoviral RNA) with a forward primer designed for ICAM-1 (Lusamba Kalonji et al. 2015).
The concentration of the soluble form of ICAM-1 (sICAM-1) and the levels of IL-1β, IL-5, IL-6, IL-13, IL-25 and IL-33 in the supernatants were examined using specific enzyme-linked immunosorbent assays (ELISAs).
Measurement of the changes in the acidic endosomes
The distribution and fluorescence intensity of the acidic endosomes in the cells were measured with LysoSensor DND-189 dye (Molecular Probes, Eugene, OR, USA), by using live-cell imaging, as previously described (Lusamba Kalonji et al. 2015).
NF-κB assay
The presence of the p50 and p65 subunits in the nuclear extracts was assessed using a TransFactor Family Colorimetric Kit-NF-κB (BD Bioscience/CLONTECH) according to the manufacturer’s instructions, as previously described (Lusamba Kalonji et al. 2015).
Measurement of airway epithelial cell damage
To examine HNE cell damage, the viability of the cells adhered on the culture vessels of plastic tubes were measured by trypan blue exclusion. Lactate dehydrogenase (LDH) concentrations in the supernatants were also measured.
Statistical analysis
The results are expressed as the mean ± SEM. For comparing data between the two groups, Student’s t tests or Mann–Whitney U tests were performed. For comparing data between more than two groups, analysis of variance (ANOVA) and subsequent post hoc analysis with Bonferroni correction was used. For all analyses, values of p < 0.05 were considered significant. The number of donors from whom the cultured HNE cells were obtained is referred to as n.
Results
Effects of clarithromycin on rhinovirus replication in nasal epithelial cells from subjects with bronchial asthma
First, we examined the effects of clarithromycin on rhinovirus replication in HNE cells. RV14 was detected in the supernatants of HNE cells obtained from subjects in the asthmatic group (asthmatic subjects) (Fig. 1a) and in the non-asthmatic group (non-asthmatic subjects) (Fig. 1b) at 24 h. The viral titers in the supernatants increased significantly over time for the first 3 days (72 h), and consistent viral titers were detected at 5 days (120 h) after infection (Fig. 1a, b). The viral titers in the supernatants of the cells obtained from the asthmatic subjects were significantly higher than those obtained from non-asthmatic subjects (Fig. 1c).
a, b The time courses of viral release in the supernatants of the cells that were obtained from asthmatic (a) or non-asthmatic (b) subjects and pretreated with clarithromycin (10 μM) (open circles) or the vehicle (closed circles) at different times after RV14 infection. c Viral release in the supernatants of the cells that were obtained from asthmatic (BA) or non-asthmatic (non-BA) subjects and pretreated with clarithromycin (RV + CAM) or the vehicle (RV), or of the untreated cells (RV + Untreated) collected 72 h after RV14 infection. d The time-courses of RV14 RNA replication in the cells from asthmatic subjects obtained at different times after RV14 infection. e Replication of RV14 RNA in the cells that were obtained from asthmatic (BA) or non-asthmatic (non-BA) subjects and pretreated with clarithromycin (RV + CAM) or the vehicle (RV), or in the untreated cells (RV + untreated) 72 h after infection. f The minimum dose of RV14 necessary to cause infection in the HNE cells pretreated with the vehicle or clarithromycin (CAM), or in the untreated cells (untreated). a–f The results are presented as the mean ± SEM from nine (a–c), three (d, e), or four (f) subjects. The results of RV14 RNA (d, e) are expressed as the relative amount of RNA expression (%) compared with that of the peak level of RV14 RNA expression in cells that were obtained from the asthmatic subjects and pretreated with the vehicle 72 h after infection. Significant differences from the cells pretreated with the vehicle are indicated by *p < 0.05 and **p < 0.01 (a, b, f). Significant differences from the cells that were obtained from the asthmatic subjects pretreated with the vehicle are indicated by +p < 0.05 and ++p < 0.01 (c, e), and significant differences from the cells that were obtained from the non-asthmatic subjects and pretreated with the vehicle are indicated by §p < 0.05 (c, e)
Clarithromycin (10 μM) pretreatment of the HNE cells obtained from subjects in both groups resulted in significantly lower RV14 viral titers in the supernatants than those from cells pretreated with the vehicle (Fig. 1a–c). The viral titers of the cells obtained from subjects in both groups pretreated with the vehicle did not differ from the titers of the cells without any treatment (Fig. 1c).
RV14 RNA was consistently observed in the HNE cells from 24 h after infection in the cells obtained from asthmatic (Fig. 1d) and non-asthmatic (data not shown) subjects. Subsequent increases were observed between 24 and 72 h after infection, and maximal levels of RV14 RNA were observed at 72 h after infection (Fig. 1d).
The RV14 RNA levels in the cells obtained from the asthmatic subjects were significantly higher than those in the cells from the non-asthmatic subjects (Fig. 1e). Pretreatment of the HNE cells obtained from subjects in both groups with clarithromycin resulted in RV14 RNA levels at 72 h after infection that were significantly lower than those of the cells pretreated with the vehicle (Fig. 1e). The RV14 RNA levels in the cells obtained from both groups pretreated with the vehicle did not differ from the levels in the cells without any treatment (Fig. 1e).
Effects on susceptibility to rhinovirus infection
To examine the effects of clarithromycin on the susceptibility to rhinovirus infection, we measured the minimum dose of RV14 that was necessary to cause infection. This minimum dose in the HNE cells pretreated with the vehicle did not differ from that in the untreated cells (Fig. 1f). In contrast, pretreatment of the cells with clarithromycin significantly decreased the susceptibility of the cells to RV14 infection. The minimum dose of RV14 that was necessary to cause infection in the cells pretreated with clarithromycin was significantly higher than that for the cells pretreated with the vehicle alone (Fig. 1f).
Effects on ICAM-1 expression
We examined the effects of clarithromycin on the expression of ICAM-1, the receptor for the major group of RVs (Greve et al. 1989), to study the mechanisms underlying the anti-rhinoviral effects of this drug. The expression of the membrane-bound form of ICAM-1 was assayed via flow cytometric analysis. Seventy-two hours after RV14 infection, the HNE cells exhibited higher ICAM-1-specific fluorescence intensity than that in the untreated cells before infection (Fig. 2c, f, g). Pretreatment and treatment with clarithromycin decreased the increases in the intensity that would otherwise be induced by RV14 infection (Fig. 2d, e, g), although clarithromycin did not change the baseline ICAM-1-specific fluorescence intensity (Fig. 2a, b, g).
a–g ICAM-1 expression assayed by flow cytometry in the cells obtained from the asthmatic subjects before (Vehicle, CAM, untreated) (a–c) and 72 h after (RV, RV + CAM, RV + untreated) (d–f) RV14 infection pretreated with clarithromycin (CAM, RV + CAM) or the vehicle (Vehicle, RV), or in the untreated cells before (untreated) or after (RV + untreated) infection. The median value of the ICAM-1-specific fluorescence intensity in the cells treated with the vehicle before infection was set to 1.0 (g). h, i Expression of ICAM-1 mRNA (h) and sICAM-1 concentrations in the supernatants (i) before (Vehicle, CAM, untreated) and 24 h after (RV, RV + CAM, RV + untreated) RV14 infection in the cells that were obtained from the asthmatic subjects and pretreated with clarithromycin (CAM, RV + CAM) or vehicle (Vehicle, RV), or in the untreated cells before (untreated) or after (RV + untreated) infection. The expression of ICAM-1 mRNA was normalized to the constitutive expression of β-actin mRNA. The mean value of the expression of ICAM-1 mRNA in the cells treated with the vehicle before infection was set to 1.0. g–i The results are presented as the mean ± SEM from three (g) or five (h, i) subjects. Significant differences from the values for the cells pretreated with the vehicle (Vehicle) before infection are indicated by *p < 0.05. Significant differences from the values for the cells pretreated with the vehicle after infection (RV) are indicated by +p < 0.05
We also examined the effects of clarithromycin on the ICAM-1 mRNA expression. The levels of ICAM-1 mRNA expression in the cells obtained from asthmatic subjects increased after RV14 infection (Fig. 2h). When the cells were pretreated and treated with clarithromycin before and after infection, the ICAM-1 mRNA expression decreased after infection (Fig. 2h). In contrast, pretreatment of the cells with clarithromycin did not decrease the baseline ICAM-1 mRNA expression relative to the levels detected in the cells pretreated with the vehicle before RV14 infection (Fig. 2h).
The levels of ICAM-1 mRNA expression in the cells that were obtained from the asthmatic subjects and pretreated with the vehicle before infection did not differ from those of the untreated cells cultured in the medium alone (Fig. 2h). Similarly, at 72 h after infection, the levels of ICAM-1 mRNA expression in the cells pretreated with the vehicle did not differ from those of the untreated cells cultured in the medium alone.
The sICAM-1 concentrations in the supernatants of the cells obtained from the asthmatic subjects were higher 72 h after RV14 infection (Fig. 2i). When the cells were treated with clarithromycin before and after infection, the sICAM-1 concentrations in the cells decreased after RV14 infection (Fig. 2i). In contrast, pretreatment of the cells with clarithromycin tended to result in sICAM-1 concentrations lower than those in the cells pretreated with the vehicle before RV14 infection, although the results did not reach statistical significance (Fig. 2i).
The concentrations of sICAM-1 in the cells that were obtained from the asthmatic subjects and pretreated with the vehicle did not differ from those in the untreated cells before infection (Fig. 2i). Similarly, the concentrations of sICAM-1 in the cells pretreated with the vehicle did not differ from those in the untreated cells at 72 h after infection.
Effects on the acidification of endosomes
To study another mechanism underlying the anti-rhinoviral effects of this drug, we also examined the effects of clarithromycin on the pH of endosomes, where RV14 RNA enters into cytoplasm (Mellman et al. 1986; Casasnovas and Springer 1994).
Pretreatment with clarithromycin decreased the number of acidic endosomes in the HNE cells obtained from the asthmatic subjects (Fig. 3a–c). Moreover, pretreatment with clarithromycin decreased the fluorescence intensity compared with that of cells that were pretreated with the vehicle and untreated cells cultured in medium alone (Fig. 3d). Pretreatment with the vehicle for 72 h did not alter the number of acidic endosomes in the cells, on the basis of the presence of green fluorescence (Fig. 3b) and the fluorescence intensity of the acidic endosomes (Fig. 3d) compared with the intensity in the untreated cells.
a–c Distribution of the acidic endosomes exhibiting green fluorescence in HNE cells obtained from asthmatic subjects 72 h after pretreatment with clarithromycin (CAM, 10 μM) (c) or the vehicle (b), or untreated cells (a). Data are representative of four different experiments (Bar = 100 μm). d The fluorescence intensity of the acidic endosomes in the cells 72 h after pretreatment with clarithromycin (CAM) or the vehicle, or in the untreated cells (untreated). The mean value of the fluorescence intensity in the vehicle-treated cells was set to 100%. The results are presented as the mean ± SEM from eight subjects. Significant differences from the values for the cells pretreated with the vehicle are indicated by *p < 0.05
Effects on cytokine production
To study the anti-inflammatory effects of clarithromycin, we measured the cytokine levels in the supernatants. Significant levels of IL-6 and IL-8 were detected in the supernatants of the untreated cells and the cells pretreated with the vehicle obtained from non-asthmatic and asthmatic subjects. The levels of IL-6 and IL-8 in the cells from the asthmatic subjects were higher than those in the cells from the non-asthmatic subjects before infection (Table 2). Furthermore, the levels of IL-6 and IL-8 in the cells that were obtained from non-asthmatic and asthmatic subjects and pretreated with clarithromycin were lower than those in the cells pretreated with the vehicle before infection (Table 2). The levels of IL-6 and IL-8 in the untreated HNE cells before infection did not differ from the levels in the cells pretreated with the vehicle.
RV14 infection increased the secretion of IL-6 and IL-8 in the supernatants of the untreated cells and the cells pretreated with the vehicle at 72 h after infection (Table 2). The levels of IL-6 and IL-8 in the cells obtained from the asthmatic subjects were higher than those of the cells obtained from the non-asthmatic subjects after infection (Table 2). Furthermore, the levels of IL-6 and IL-8 in the cells that were obtained from the non-asthmatic subjects and pretreated with clarithromycin were lower than those of the cells pretreated with the vehicle after infection (Table 2). Similarly, the levels of IL-6 and IL-8 in the supernatants of the cells that were obtained from the asthmatic subjects and pretreated with clarithromycin were lower than those of the cells pretreated with the vehicle after infection (Table 2). The levels of IL-6 and IL-8 in the untreated cells from both groups did not differ from the levels in the cells pretreated with the vehicle after infection.
Before infection, the supernatants of the cells did not contain a significant amount of IL-33, but a significant amount was detected after infection (Table 2). The levels of IL-33 in the cells obtained from the asthmatic subjects were higher than those in the cells from the non-asthmatic subjects after infection (Table 2). Furthermore, the levels of IL-33 in the cells that were obtained from non-asthmatic and asthmatic subjects and pretreated with clarithromycin were lower than those in the cells pretreated with the vehicle after infection (Table 2).
The concentrations of IL-5, IL-13 and IL-25 were lower than the detection limits (<4 pg/mL for IL-5, <16 pg/mL for IL-25 and <6 pg/mL for IL-13).
Effects on NF-κB
To study the mechanisms underlying the anti-inflammatory and anti-rhinoviral effects of clarithromycin, we measured the effects of clarithromycin on NF-κB activity, because NF-κB increases the gene expression of ICAM-1 and pro-inflammatory cytokines and regulates endosomal pH (Zhu et al. 1996; Papi and Johnston 1999; Yamaya et al. 2016).
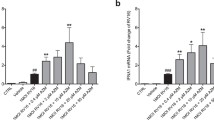
Pretreatment of the HNE cells obtained from the asthmatic subjects with clarithromycin resulted in lower levels of NF-κB p50 and p65 in the nuclear extracts than those in the cells pretreated with the vehicle before RV14 infection (Fig. 4a, b).
Amount of p50 (a) and p65 (b) in the nuclear extracts of the HNE cells obtained from the asthmatic subjects before (Vehicle, CAM) and 72 h after (RV, RV + CAM) RV14 infection. The cells were pretreated with clarithromycin (CAM, 10 μM) or vehicle (Vehicle) for 72 h before infection or were pretreated starting at 72 h before infection and treated until 72 h after infection with clarithromycin (RV + CAM) or the vehicle (RV). The results are expressed as the optical density (OD) and are given as the mean ± SEM for cells from four subjects. Significant differences compared with the vehicle alone before infection (Vehicle) are indicated by *p < 0.05. Significant differences compared with pretreatment with the vehicle after infection (RV) are indicated by +p < 0.05
RV14 infection increased the amount of NF-κB p50 in the cells pretreated with the vehicle, and clarithromycin decreased the amount of p50 after infection when the cells were pretreated before infection and treated after infection with clarithromycin (Fig. 4a).
RV14 infection tended to increase the amount of NF-κB p65 in the cells pretreated with the vehicle, and clarithromycin tended to decrease the amount of p65 following infection when the cells were treated with clarithromycin before and after infection, although the results did not reach statistical significance (Fig. 4b).
The amount of NF-κB p50 and p65 in the untreated cells [0.33 ± 0.02 optical density (OD), n = 4, and 0.42 ± 0.03 OD, n = 3] did not differ from the cells pretreated with the vehicle (p > 0.02) before RV14 infection.
Effects on cytotoxicity
We examined the cytotoxic effects of clarithromycin to demonstrate that the decreased production of ICAM-1 and pro-inflammatory cytokines in the cells pretreated with clarithromycin after RV 14 infection was not caused by the cytotoxic effects of this drug.
Pretreating the HNE cells with clarithromycin (10 μM) or the vehicle for 72 h did not increase the proportion of dead cells among the attached cells (98 ± 1% in clarithromycin, 98 ± 1% in the vehicle, and 97 ± 1% in the medium alone) (p > 0.20; compared with pretreatment with the vehicle, n = 4). Furthermore, pretreatment with clarithromycin for 72 h did not change the concentrations of LDH in the supernatants (34 ± 3 IU/L in clarithromycin, 32 ± 3 IU/L in the vehicle, and 33 ± 3 IU/L in the medium alone; p > 0.20, n = 5).
Discussion
In the present study, we demonstrated that pretreatment with the macrolide clarithromycin decreased the RV14 titers and cytokine concentrations in the supernatants of primary cultures of human nasal epithelial (HNE) cells as well as RV14 RNA replication within the cells obtained from asthmatic and non-asthmatic subjects. Pretreatment with clarithromycin decreased the mRNA and protein expression of ICAM-1, the receptor for the major group of RVs (Greve et al. 1989), after RV14 infection. Pretreatment with clarithromycin also decreased the number and fluorescence intensity of acidic endosomes through which RV RNA enters the cytoplasm (Pérez and Carrasco 1993; Casasnovas and Springer 1994) and increased the minimum dose of RV14 necessary to cause a viral infection. These findings suggested that clarithromycin inhibited RV14 infection partially by decreasing the production of its receptor and the number of acidic endosomes.
Macrolide antibiotics, including erythromycin and clarithromycin, decrease the replication of respiratory viruses, such as RV, influenza virus and respiratory syncytial virus (Suzuki et al. 2002; Yamaya et al. 2010, 2012). Macrolide antibiotics also decrease the production of pro-inflammatory cytokines, such as IL-1β and IL-6, and a major component of mucin, MUC5AC, in human tracheal epithelial (HTE) and HNE cells infected with RV (Suzuki et al. 2002; Inoue et al. 2006). We observed that pretreatment with the macrolide clarithromycin decreased the production of IL-6 and IL-8 in the supernatants after RV14 infection. These findings suggested that the anti-inflammatory effects of macrolides may contribute to the lower frequency of exacerbation and improved symptoms in severe neutrophilic asthma (Simpson et al. 2008).
ICAM-1 expressed on the cells is the site of attachment for the major group of RVs, such as RV14 (Greve et al. 1989). RVs form RV-soluble ICAM-1 complexes, and these complexes release viral RNA (Casasnovas and Springer 1994). Furthermore, after attaching to ICAM-1, RVs are internalized, delivered to endosomes, where they release RNA after exposure to the acidic pH in the endosomes (Mellman et al. 1986; Casasnovas and Springer 1994). Thus, the entry of RV14 RNA into the cytoplasm in infected cells appears to be mediated by destabilization due to receptor binding, endosomal acidification, or both (Casasnovas and Springer 1994). In contrast, infection of HeLa cells and HTE cells by RV14 is inhibited by the macrolide bafilomycin A1 (Pérez and Carrasco 1993; Suzuki et al. 2001). Endosomal pH is regulated by the vacuolar H+-ATPase (Mellman et al. 1986) and ion transport across Na+/H+ exchangers (Nass and Rao 1998). The macrolide bafilomycin A1 inhibits vacuolar H+-ATPase (Pérez and Carrasco 1993) and increases endosomal pH (Pérez and Carrasco 1993; Suzuki et al. 2001). In the present study, the ICAM-1 expression in the HNE cells was decreased by clarithromycin treatment after RV14 infection, and this treatment increased the endosomal pH in the cells. Therefore, the decreased expression of ICAM-1 and increased pH in the acidic endosomes through the inhibition of vacuolar H+-ATPase might be associated with the decrease in RV14 proliferation, as shown previously (Pérez and Carrasco 1993; Suzuki et al. 2001; Lusamba Kalonji et al. 2015). Furthermore, in addition to these mechanisms, Gielen et al. have suggested that azithromycin has anti-rhinoviral activity through the up-regulation of anti-virus substrate IFNs (Gielen et al. 2010).
We demonstrated that pretreatment of HNE cells with clarithromycin decreased the ICAM-1 expression and the production of pro-inflammatory cytokines after RV14 infection and increased the endosomal pH in the absence of RV14 infection. NF-κB increases the gene expression of ICAM-1, vacuolar H+-ATPase (van der Kraan et al. 2013) and pro-inflammatory cytokines, such as IL-6 (Zhu et al. 1996; Papi and Johnston 1999). We have previously reported that the decreased production of ICAM-1 and pro-inflammatory cytokines, including IL-6 and IL-8, and the increased endosomal pH in HTE and HNE cells by erythromycin and the non-antibiotic macrolide EM900 is associated with inhibition of NF-κB (Suzuki et al. 2002; Lusamba Kalonji et al. 2015). Furthermore, treatment with an inhibitor of NF-kB, caffeic acid phenethyl ester, increases endosomal pH in HNE cells (Yamaya et al. 2016). The inhibition of NF-κB activity exerted by clarithromycin that was observed in the present study are consistent with the findings of a previous study showing that clarithromycin decreases NF-κB activation in HTE cells after influenza virus infection (Yamaya et al. 2010). Thus, the decreased production of ICAM-1, IL-6 and IL-8 and the increased endosomal pH by clarithromycin through the modulation of NF-κB activation may be associated with anti-viral and anti-inflammatory effects.
In contrast, the production of IL-33 is enhanced by inflammatory substrates, such as TNF-α (Kempuraj et al. 2013), whose release is enhanced in response to RV infection (Terajima et al. 1997; Suzuki et al. 2002), and IL-33 activates NF-kB (Funakoshi-Tago et al. 2011). Therefore, the decreased production of IL-33 by clarithromycin may be partially caused by the decreased production of inflammatory substrates through the inhibition of NF-kB by clarithromycin.
The 12-, 14- and 15-membered macrolides, including EM900, erythromycin and azithromycin, have anti-rhinoviral effects (Suzuki et al. 2002; Gielen et al. 2010; Lusamba Kalonji et al. 2015), and we demonstrated the anti-rhinoviral effect of the 14-membered macrolide clarithromycin. In contrast, the 16-membered macrolide telithromycin does not decrease RV replication (Gielen et al. 2010); however, another 16-membered macrolide, bafilomycin A1, has anti-rhinoviral effects (Pérez and Carrasco 1993; Suzuki et al. 2001). On the basis of these findings, anti-rhinoviral activities may differ among the types of macrolides.
The relationship between the structure of clarithromycin and its anti-inflammatory and anti-viral effects has been unclear. Sugawara et al. have demonstrated that the modification of the N,N-dimethylamino group on the desosamine moiety of EM900, an analogue of erythromycin, changes its anti-inflammatory activity (Sugawara et al. 2012). Similarly, Bosnar et al. have demonstrated that erythromycin-derived macrolides, including clarithromycin, characterized by N′-substituted 2′-O,3′-N-carbonimidoyl bridged desosamine sugars, have anti-inflammatory effects (Bosnar et al. 2012); however, those studies have not shown a decrease in ICAM-1. In the present and previous studies, we have demonstrated that macrolides, including clarithromycin and erythromycin, may decrease RV14 replication through reducing ICAM-1 expression via the modulation of NF-κB (Suzuki et al. 2001, 2002; Lusamba Kalonji et al. 2015); however, no study has investigated the relationship between the structure of clarithromycin and the decrease in ICAM-1 expression and the modulation of NF-κB.
A macrolide and a potent inhibitor of the vacuolar H+-ATPase bafilomycin A1 (Pérez and Carrasco 1993) decreases RV replication through increasing pH of acidic endosomes (Pérez and Carrasco 1993; Suzuki et al. 2001). Regarding the structure of bafilomycin A1, Shibata et al. have demonstrated that the absence of two methyl groups located at C-6 and C-8 causes a conformational change in the macrocyclic core structure of bafilomycin A1, and this change is necessary for binding to the vacuolar H+-ATPase (2015); however, no study has demonstrated the relationship between the structure of clarithromycin and the binding activity to the vacuolar H+-ATPase.
Thus, the findings reported by three study groups (Sugawara et al. 2012; Bosnar et al. 2012; Shibata et al. 2015) have suggested the relationship between the structure of macrolides and the anti-viral and anti-inflammatory activities; however, further studies are required to clarify the structure–function relationship of clarithromycin.
Asthmatic patients have bronchial epithelial cells and bronchoalveolar lavage cells that exhibit defective RV-induced IFN production (Wark et al. 2005), which is correlated with the severity of RV-induced asthma exacerbation and RV replication (Contoli et al. 2006). This mechanism has been suggested to cause RV infection-induced asthma exacerbations (Jackson and Johnston 2010).
Furthermore, the increased ICAM-1 expression has been observed in the airway of asthmatic subjects (Wegner et al. 1990; Manolitsas et al. 1994), although ICAM-1 expression has not been found to be different between asthmatic subjects and healthy controls in a report by Wark et al. (2005). We also observed increased ICAM-1 expression in HNE cells obtained from asthmatic subjects in the present study. Because ICAM-1 is the receptor for the major group of RVs, including RV14 (Greve et al. 1989), increased ICAM-1 expression may increase susceptibility to RV infection, as suggested by Manolitsas et al. (1994). The increased RV replication and cytokine production in the asthmatic subjects in the present study was consistent with previously reported findings in in vitro (Contoli et al. 2006; Jackson et al. 2014) and in vivo (de Kluijver et al. 2003; Jackson et al. 2014). Therefore, enhanced RV14 replication and cytokine production in the airway in asthmatic subjects may cause more severe airway inflammation and subsequent asthma exacerbation.
In the present study, clarithromycin also decreased the production of IL-33 after RV infection in HNE cells, although the levels of IL-33 have been found to be lower than those in nasal lavage fluids after experimental RV infection in an in vivo study (Jackson et al. 2014). IL-33 induces mucin gene expression and goblet cell hyperplasia (Ishinaga et al. 2016). Furthermore, the IL-33-induced production of IL-5 and IL-13 in innate type-2 lymphoid stimulates airway eosinophils in allergic patients (Barnes 2015). Clarithromycin has been found to inhibit mucus hypersecretion and IL-13-induced goblet cell hyperplasia (Rubin et al. 1997; Tanabe et al. 2011) and to inhibit IL-33 mRNA expression by sinonasal mucosa in an explant model study (Zeng et al. 2015). The anti-inflammatory action of macrolides during allergic inflammation has been demonstrated in mice with steroid-insensitive inflammation (Essilfire et al. 2015). These findings suggest that the inhibitory effects of macrolides on mucus hypersecretion and eosinophil stimulation induced by IL-33 may also be associated with improved pulmonary function and eosinophilic inflammation in children with asthma (Wan et al. 2016).
Jackson et al. have reported the up-regulation of inflammatory substrates, including IL-5, IL-13 and IL-33, after experimental exposure to RV in nasal lavage samples in an in vivo study and in the supernatants of human bronchial epithelial cells in an in vitro study (2014). In contrast, we did not detect significant amounts of IL-5 and IL-13 in the supernatants of the cells. The production of IL-33 was detected in the supernatants after RV14 infection, but the levels were lower than those reported by Jackson et al. (2014). The reasons for these differences are unclear; however, we used primary cultures of HNE cells in which inflammatory cells, such as eosinophils, and fibroblasts are absent (Yamaya et al. 2016). Furthermore, the culture methods, including the culture medium components, that we used in the present study were different from those in the report by Jackson et al. (2014). Therefore, the absence of cells other than epithelial cells and the differences in the types of epithelial cells and in the culture methods may be associated with the differences in cytokine production observed in the present study. The mild severity of asthmatic symptoms in the subjects in the present study may also be related to the low IL-33 values, as observed by Jackson et al. in nasal lavage samples from asthmatic subjects with mild symptoms (2014).
Pretreatment with clarithromycin decreased the expression of ICAM-1 after RV14 infection, although this pretreatment did not decrease ICAM-1 expression before infection. In contrast, erythromycin decreased ICAM-1 expression in the HTE cells before infection, as we have previously reported (Suzuki et al. 2002). The precise reasons for these differences are unclear, but treatment with EM900, the non-antibiotic macrolide, also has not been found to have significant inhibitory effects on the ICAM-1 expression in HNE cells before RV infection (Lusamba Kalonji et al. 2015). Differences in cell type may be associated with the effects of clarithromycin on ICAM-1 expression before infection; however, the decreased ICAM-1 expression induced by RV infection may have been associated with decreased RV replication in the present study.
We have previously reported that RV14 titers and cytokine concentrations, including IL-6 and IL-8, in the supernatants, RV14 RNA replication and susceptibility to RV14 infection are higher in HNE cells obtained from allergic subjects, including patients with bronchial asthma and allergic rhinitis, than in cells from non-allergic subjects (Yamaya et al. 2016). The ICAM-1 expression and the number and fluorescence intensity of acidic endosomes were higher in HNE cells from the allergic subjects. The abundance of p50 and p65 subunits of transcription factor NF-κB in the nuclear extracts of cells from allergic subjects was also greater than that in non-allergic subjects. Therefore, the increased RV14 replication observed in HNE cells obtained from the asthmatic subjects in the present study may have been partly associated with the enhanced ICAM-1 expression and decreased endosomal pH through NF-κB activation, as previously reported (Yamaya et al. 2016).
Treatment of the cells with clarithromycin did not change the viability of HNE cells or LDH levels in the supernatants, thus indicating no apparent cytotoxicity from clarithromycin, as we have previously demonstrated in HTE cells (Yamaya et al. 2010). Therefore, the decreased production of pro-inflammatory cytokines and ICAM-1 after RV 14 infection was not likely to be caused by cytotoxic effects of clarithromycin.
In conclusion, an evaluation of the results of this study is limited because we used a cellular model that consisted of culturing the HNE cells under immersed feeding conditions; however, RV replication and cytokine production may be enhanced in nasal epithelial cells obtained from asthmatic subjects and may be modulated by clarithromycin.
References
Barnes PJ (2015) Therapeutic approaches to asthma-chronic obstructive pulmonary disease overlap syndromes. J Allegy Clin Immunol 136:531–545
Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, Pedersen SE, GOAL Investigators Group (2004) Can guideline-defined asthma control be achieved? The gaining optimal asthma control study. Am J Respir Crit Care Med 170:836–844
Beale J, Jayaraman A, Jackson DJ, Macintyre JD, Edwards MR, Walton RP, Zhu J, Ching YM, Shamji B, Edwards M, Westwick J, Cousins DJ, Hwang YY, McKenzie A, Johnston SL, Bartlett NW (2014) Rhinovirus-induced IL-25 in asthma exacerbation drives type 2 immunity and allergic pulmonary inflammation. Sci Transl Med 6:256ra134
Bosnar M, Kragol G, Koštrun S, Vujasinović I, Bošnjak B, Mihaljević VB, Ištuk ZM, Kapić S, Hrvačić B, Brajša K, Tavčar B, Jelić D, Glojnarić I, Verbanac D, Čulić O, Padovan J, Alihodžić S, Haber VE, Spaventi R (2012) N′-Substituted-2′-O,3′-N-carbonimidoyl bridged macrolides: novel anti-inflammatory macrolides without antimicrobial activity. J Med Chem 55:6111–6123
Casasnovas JM, Springer TA (1994) Pathway of rhinovirus disruption by soluble intercellular adhesion molecule 1 (ICAM-1): an intermediate in which ICAM-1 is bound and RNA is released. J Virol 68:5882–5889
Choi YS, Park JA, Kim J, Rho SS, Park H, Kim YM, Kwon YG (2012) Nuclear IL-33 is a transcriptional regulator of NF-κB p65 and induces endothelial cell activation. Biochem Biophys Res Commun 421:305–311
Contoli M, Message SD, Laza-Stanca V, Edwards MR, Wark PA, Barlett NW, Kebadze T, Mallia P, Stanciu LA, Parker HL, Alater L, Lewis-Antes A, Kon OM, Holgate ST, Davies DE, Kotenko SV, Papi A, Johnston SL (2006) Role of deficient type III interferon-lambda production in asthma exacerbations. Nat Med 12:1023–1026
Corne JM, Marshall C, Smith S, Schreiber J, Sanderson G, Holgate ST, Johnston SL (2002) Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: a longitudinal cohort study. Lancet 359:831–834
Corren J, Lemanske RF Jr, Hanania N, Korenblat PE, Parsey MV, Arron JR, Harris JM, Scheerens H, Wu LC, Su Z, Mosesova S, Eisner MD, Bohen S, Matthews JG (2011) Lebrikizumab treatment in adults with asthma. New Engl J Med 365:1088–1098
de Kluijver J, Grünberg K, Pons D, de Klerk EP, Dick CR, Sterk PJ, Hiemstra PS (2003) Interleukin-1β and interleukin-1ra levels in nasal lavages during experimental rhinovirus infection in asthmatic and non-asthmatic subjects. Clin Exp Allergy 33:1415–1418
Demyanets S, Konya V, Kastl SP, Kaun C, Rauscher S, Niessner A, Pentz R, Pfaffenberger S, Rychli K, Lemberger CE, de Martin R, Heinemann A, Huk I, Gröger M, Maurer G, Huber K, Wojta J (2011) Interleukin-33 induces expression of adhesion molecules and inflammatory activation in human endothelial cells and in human atherosclerotic plaques. Arterioscler Thromb Vasc Biol 31:2080–2090
Essilfire AT, Horvat JC, Kim R, Mayall JR, Pinkerton JW, Beckett EL, Starkey MR, Simpson JL, Foster PS, Gibson PG, Hansbro PM (2015) Macrolide therapy suppress key features of experimental steroid-sensitive and steroid-insensitive asthma. Thorax 70:458–467
Fonseca-Aten M, Okada PJ, Bowlware KL, Chavez-Bueno S, Mejias A, Rois AM, Katz K, Ng S, McCracken GH, Ramilo O, Hardy RD (2006) Effect of clarithromycin on cytokines and chemokines in children with an acute exacerbation of recurrent wheezing: a double-blind, randomized, placebo-controlled trial. Ann Allergy Asthma Immunol 97:457–463
Fraenkel DJ, Bardin PG, Sanderson G, Lampe F, Johnston SL, Holgate ST (1995) Lower airways inflammation during rhinovirus colds in normal and in asthmatic subjects. Am J Respir Crit Care Med 151:879–886
Funakoshi-Tago M, Tago K, Sato Y, Tominaga S, Kasahara T (2011) JAK2 is an important signal transducer in IL-33-induced NF-κB activation. Cell Signal 23:363–370
Gielen V, Johnston SL, Edwards MR (2010) Azithromycin induces anti-viral responses in bronchial epithelial cells. Eur Respir J 36:646–654
Greve JM, Davis G, Meyer AM, Forte CP, Yost SC, Marior CW, Kamarck ME, McClelland A (1989) The major human rhinovirus receptor is ICAM-1. Cell 56:839–847
Halder P, Brightling CE, Hargadon B, Gupta S, Monteiro W, Sousa A, Marshall RP, Bradding P, Green RH, Wardlaw AJ, Pavord ID (2009) Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med 360:973–984
Inoue D, Yamaya M, Sasaki T, Hosoda M, Kubo H, Numazaki M, Tomioka Y, Yasuda H, Sekizawa K, Nishimura H, Sasaki H (2006) Mechanisms of mucin production by rhinovirus infection in cultured human tracheal surface epithelium and submucosal glands. Respir Physiol Neurobiol 154:484–499
Ishinaga H, Kitano M, Tada M, D’Alessandro-Gabazza CN, Gabazza EC, Shah SA, Tekeuchi K (2016) Interleukin-33 induces mucin gene expression and goblet cell hyperplasia in human nasal epithelial cells. Cytokine 90:60–65
Jackson DJ, Johnston SL (2010) The role of viruses in acute exacerbations of asthma. J Allergy Clin Immunol 126:1178–1187
Jackson DJ, Makrinioti H, Rana BM, Shamji BW, Trujillo-Torralbo MB, Footitt J, Del-Rosario Jerico, Telcian AG, Nikonova A, Zhu J, Aniscenko J, Gogsadze L, Bakhsoliani E, Traub S, Dhariwal J, Porter J, Hunt D, Hunt T, Hunt T, Stanciu LA, Khaitov M, Bartlett NW, Edwards MR, Kon OM, Mallia P, Papadopoulos NG, Akdis CA, Westwick J, Edwards MJ, Cousins DJ, Walton RP, Johnston SL (2014) IL-33-dependent type 2 inflammation during rhinovirus-induced asthma exacerbations in vivo. Am J Respir Crit Care Med 190:1373–1382
Johnston SL, Pattemore PK, Sanderson G, Smith S, Lampe F, Josephs L, Symington P, O’Toole S, Mynt SH, Tyrrell DA, Holgate ST (1995) Community study of role of viral infections in exacerbations of asthma in 9-11 year old children. Br Med J 310:1225–1229
Kempuraj D, Twait EC, Williard DE, Yuan Z, Meyerholz DK, Samuel I (2013) TNF-α stimulation increased IL-33 release while IL-33 stimulation increased proinflammatory cytokine release. PLoS ONE 8:e56866
Lemanske RF, Dick EC, Swenson CA, Vrtis RF, Busse WW (1989) Rhinovirus upper respiratory infection increases airway hyperreactivity and late asthmatic reactions. J Clin Investig 83:1–10
Lusamba Kalonji N, Nomura K, Kawase T, Ota C, Kubo H, Sato T, Yanagisawa T, Sunazuka T, Ōmura S, Yamaya M (2015) The non-antibiotic macrolide EM900 inhibits rhinovirus infection and cytokine production in human airway epithelial cells. Physiol Rep 3:e12557
Manolitsas ND, Trigg CJ, McAulay AE, Wang JH, Jordan SE, D’Ardenne AJ, Davies RJ (1994) The expression of intercellular adhesion molecule-1 and the & 1-integrins in asthma. Eur Respir J 7:1439–1444
Mellman I, Fuchs R, Helenius A (1986) Acidification of the endocytic and exocytic pathways. Ann Rev Biochem 55:663–700
Minor TE, Baker JW, Dick EC, DeMeo AN, Oullette JJ, Cohen M, Reed CE (1974) Greater frequency of viral respiratory infections in asthmatic children as compared with their non-asthmatic siblings. J Pediatr 85:472–477
Nass R, Rao R (1998) Novel localization of a Na+/H+ exchanger in a late endosomal compartment of yeast. Implications for vacuole biogenesis. J Biol Chem 273:21054–21060
Nicholson KG, Kent J, Ireland DC (1993) Respiratory viruses and exacerbations of asthma in adults. Br Med J 307:982–986
Ohta K, Miyamoto T, Amagasaki T, Yamamoto M (2009) Efficacy and safety of omalizumab in an Asian population with moderate-to-severe persistent athma. Respirology 14:1156–1165
Papi A, Johnston SL (1999) Respiratory epithelial cell expression of vascular cell adhesion molecule-1 and its up-regulation by rhinovirus infection via NF-κB and GATA transcription factors. J Biol Chem 274:30041–30051
Pauwels RA, Löfdahl CG, Postma DS, Tattersfield AE, O’Byrne P, Barnes PJ, Ullman A (1997) Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N Engl J Med 337:1405–1411
Pérez L, Carrasco L (1993) Entry of poliovirus into cells does not require a low-pH step. J Virol 67:4543–4548
Rubin BK, Druce H, Ramirez OE, Palmer R (1997) Effect of clarithromycin on nasal mucus properties in healthy subjects and in patients with purulent rhinitis. Am J Respir Crit Care Med 155:2018–2023
Shibata H, Tsuchikawa H, Hayashi T, Matsumori N, Murata M, Usui T (2015) Modification of bafilomycin structure to efficiently synthesize solid-state NMR probes that selectively bind to vacuolar-type ATPase. Chem Asian J 10:915–924
Simpson JL, Powell H, Boyle MJ, Scott RJ, Gibson PG (2008) Clarithromycin targets neutrophilic airway inflammation in refractory asthma. Am J Respir Crit Care Med 177:148–155
Sin DD, Man J, Sharpe H, Gan WQ, Man SF (2004) Pharmacologic management to reduce exacerbations in adults with asthma: a systematic review and meta analysis. JAMA 292:367–376
Sugawara A, Sueki A, Hirose T, Shima H, Akagawa KS, Omura S, Sunazuka T (2012) Novel 12-membered non-antibiotic macrolides, EM900 series with anti-inflammatory and/or immunomodulatory activity; synthesis, structure-activity relationships and in vivo study. J Antibiot (Tokyo) 65:487–490
Suzuki T, Yamaya M, Sekizawa K, Hosoda M, Yamada N, Ishizuka S, Nakayama K, Yanai M, Numazaki Y, Sasaki H (2001) Bafilomycin A1 inhibits rhinovirus infection in human airway epithelium: effects on endosome and ICAM-1. Am J Physiol 280:L1115–L1127
Suzuki T, Yamaya M, Sekizawa K, Hosoda M, Yamada N, Ishizuka S, Yoshino A, Yasuda H, Takahashi H, Nishimura H, Sasaki H (2002) Erythromycin inhibits rhinovirus infection in cultured human tracheal epithelial cells. Am J Respir Crit Care Med 165:1113–1118
Tanabe T, Kanoh S, Tsushima K, Yamazaki Y, Kubo K, Rubin KR (2011) Clarithromycin inhibits interleukin-13-induced goblet cell hyperplasia in human airway cells. Am J Respir Cell Mol Biol 45:1075–1083
Tarlo S, Broder I, Spence L (1979) A prospective study of respiratory infection in adult asthmatics and their normal spouses. Clin Allergy 9:293–301
Terajima M, Yamaya M, Sekizawa K, Okinaga S, Suzuki T, Yamada N, Nakayama K, Ohrui T, Oshima T, Numazaki Y, Sasaki H (1997) Rhinovirus infection of primary cultures of human tracheal epithelium: role of ICAM-1 and IL-1β. Am J Physiol 273:L749–L759
U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute (2015) Global initiative for asthma: global strategy for asthma management and prevention 2015. www.ginasthma.org/local/uploads/files/GINA_Report_2015_May19.pdf
van der Kraan AG, Chai RC, Singh PP, Lang BJ, Xu J, Gillespie MT, Price JT, Quinn JM (2013) HSP90 inhibitors enhance differentiation and MITF (microphthalmia transcription factor) activity in osteoclast progenitors. Biochem J 451:235–244
Wan KS, Liu YC, Huang CS, Su YM (2016) Effects of low-dose clarithromycin added to fluticasone on inflammatory markers and pulmonary function test among children with asthma: a randomized clinical trial. Allergy Rhinol 7:e131–e134
Wark PAB, Gibson PG (2006) Asthma exacerbation. Thorax 61:909–915
Wark PA, Johnston SL, Bucchieri F, Powell R, Puddicombe S, Laza-Stanca V, Holgate ST, Davies DE (2005) Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med 201:937–947
Wegner CD, Gundel RH, Reilly P, Haynes N, Letts LG, Rothlein R (1990) Intercellular adhesion molecule-1 (ICAM-1) in the pathogenesis of asthma. Science 247:456–459
Yamaya M (2012) Virus infection-induced bronchial asthma exacerbation. Pulm Med 2012:834826
Yamaya M, Shinya K, Hatachi Y, Kubo H, Asada M, Yasuda H, Nishimura H, Nagatomi R (2010) Clarithromycin inhibits type A seasonal influenza virus infection in human airway epithelial cells. J Pharmacol Exp Ther 333:81–90
Yamaya M, Azuma A, Takizawa H, Kadota J, Tamaoki J, Kudoh S (2012) Macrolide effects on the prevention of COPD exacerbations. Eur Respir J 40:485–494
Yamaya M, Nomura K, Arakawa K, Nishimura H, Lusamba Kalonji N, Kubo H, Nagatomi R, Kawase T (2016) Increased rhinovirus replication in nasal mucosa cells in allergic subjects is associated with increased ICAM-1 levels and endosomal acidification and is inhibited by l-carbocisteine. Immun Inflamm Dis 4:166–181
Zeng M, Li ZY, Ma J, Cao PP, Wang H, Cui YH, Liu Z (2015) Clarithromycin and dexamethasone show similar anti-inflammatory effects on distinct phenotypic chronic rhinosinusitis: an explant model study. BMC Immunol 16:37
Zhu Z, Tang W, Ray A, Wu Y, Einarsson O, Landry ML, Gwaltney Jr J, Elias JA (1996) Rhinovirus stimulation of interleukin-6 in vivo and in vitro. Evidence for nuclear factor & kappa B-dependent transcriptional activation. J Clin Investig 97:421–430
Acknowledgements
We thank Biomedical Research Unit of Tohoku University Hospital for technical support. Dr. Yamaya is a Professor in the Advanced Preventive Medicine for Infectious Disease, Tohoku University Graduate School of Medicine. This department was funded by eight pharmaceutical companies, which are as follows: Kyorin Pharmaceutical Co. Ltd., Mylan EPD, LLC., Taisho Toyama Pharmaceutical Co., Ltd., Toyama Chemical Co., Ltd., Nippon Boehringer-Ingelheim Co., Ltd., Teijin Pharma Co., Ltd., and AstraZeneca Co. Ltd. and Otsuka Pharmaceutical Co. Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Yamaya, M., Nomura, K., Arakawa, K. et al. Clarithromycin decreases rhinovirus replication and cytokine production in nasal epithelial cells from subjects with bronchial asthma: effects on IL-6, IL-8 and IL-33. Arch. Pharm. Res. 43, 526–539 (2020). https://doi.org/10.1007/s12272-017-0950-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-017-0950-x