Abstract
Anthracycline anticancer agents are widely used in the cancer chemotherapy for hepatocelluar carcinoma. However, accurate kinetic analyses of the hepatocellular uptake and efflux of the drugs have not been reported. We, therefore, investigated the hepatobiliary transport of epirubicin, an anthracycline derived antibiotic, after intravenous (i.v.) infusion in rats. The hepatic uptake mechanisms of epirubicin were also investigated in isolated rat hepatocytes. To analyze epirubicin levels in the biological samples, we used an HPLC-based method which has been validated for a kinetic study by suitable criteria. The uptake process of epirubicin by the hepatocytes revealed one saturable component, with a Km of 99.1 μg/mL and Vmax of 3.70 μg/min/106 cells. The initial uptake velocity of epirubicin was significantly inhibited in a temperature-dependent manner. The velocity was also reduced in the presence of metabolic inhibitors such as rotenone or carbonylcyanide-p-(trifluoromethoxy)-phenylhydrazone. Substrates for organic anion transporters such as bromosulfophthalein and taurocholate significantly inhibited the initial uptake velocity of epirubicin. We also attempted to determine the hepatobiliary transport of epirubicin after i.v. infusion in vivo. At steady-state after i.v. infusion of epirubicin (10–160 μg/min/kg), the drug was extensively accumulated in the liver, followed by excretion into bile. Furthermore, the CLbile,plasma and CLbile,liver decreased with a corresponding increase in the Css,plasma and Css,liver. In conclusion, present studies using isolated rat hepatocytes and in vivo i.v. infusion demonstrate that epirubicin is likely to be taken up into liver cells via organic anion transporting polypeptides, and that its biliary excretion might be mediated via specific transporters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anthracyclines are some of the most effective anticancer treatments ever developed and are effective against more types of cancer than any other class of chemotherapy agents (Minotti et al. 2004; Peng et al. 1993). Epirubicin, an antineoplastic drug, is favoured over doxorubicin, the most popular anthracycline, in some chemotherapy regimens as it appears to cause fewer side-effects (Berchem et al. 1996; Robert et al. 1993). In the case of cancer chemotherapy for hepatocellular carcinoma, epirubicin is widely used. Thus, determining its hepatobiliary transport is highly useful. Recently, we investigated the pharmacokinetics of epirubicin after an intravenous (i.v.) bolus administration at a dose of 2–50 mg/kg (Shin et al. 2013). The clearance of epirubicin showed nonlinear kinetics at high doses. Such a nonlinearity in the clearance of epirubicin might be attributable to the saturation in the elimination process in hepatobiliary transport (Shin et al. 2013). In our previous study, epirubicin mainly distributed to the liver, kidney and lungs after i.v. bolus administration, as was observed with the other anthracycline antibiotics (Fujita et al. 1986; Iguchi et al. 1980; Yoo et al. 2005; Nagata et al. 2008). Moreover, epirubicin was excreted largely in the bile after i.v. bolus administration (Shin et al. 2013). However, the mechanisms by which epirubicin is selectively excreted in the bile have not been clarified yet.
Hepatic uptake and biliary excretion were considered to be major pathways in the removal of epirubicin (Shin et al. 2013). In addition, it has been reported that carrier-mediated transport contributes to hepatic uptake and biliary excretion (Yamazaki et al. 1996). Thus, saturation of membrane transport proteins in both hepatic uptake and biliary excretion might be one of the factors that cause nonlinear clearance of epirubicin in vivo. We, therefore, have investigated the hepatobiliary transport of epirubicin in rats. The mechanisms of epirubicin uptake were determined in isolated rat hepatocytes. We also investigated the kinetics of hepatobiliary transport after i.v. infusion in vivo. To analyze epirubicin levels in biological samples, we used a simple HPLC-based method which was developed and validated in our laboratory.
Materials and methods
Materials
Epirubicin was obtained from Boryung Pharmaceutical Co. Ltd. (Seoul, Korea). Solvents used in the epirubicin analysis were of HPLC grade and were filtered and degassed just prior to use. All other chemicals used in this study were of analytical reagent grade.
Adult male Sprague–Dawley rats weighing 230–250 g (Sam Tac Co. Ltd., Suwon, Gyeonggi-do, Korea) were used for the kinetic studies. They were housed in individual metabolic cages and maintained under a 12 h light/dark cycle with free access to water.
HPLC analysis of epirubicin levels in biological samples
Epirubicin levels were assayed by reverse phase HPLC on a Luna C18 column (4.6 mm × 250 mm, 5 μm) (Phenomenex, Torrance, CA, USA) that was interfaced with a HPLC system (Jasco Co. Ltd., Tokyo, Japan) (Shin et al. 2013). This system consisted of a model PU-980 pump, a model AS-950-10 autoinjector, a model FP-2020 fluorescence detector, and a LC-Net II control Borwin integrator (Jasco Co. Ltd., Tokyo, Japan). The mobile phase was a mixture of 0.02 M NaH2PO4 buffer and MeOH (38:62, v/v %). The flow rate was 0.7 mL/min. The epirubicin in elutes was monitored fluorometrically at an excitation wavelength (λex) of 480 nm and an emission wavelength (λem) of 550 nm.
The retention time of epirubicin and the internal standard (I.S.; daunorubicin) were 18.7 and 12.8 min, respectively. The chromatogram shows no peaks that interfere with the epirubicin and I.S. signals. To determine the linearity of the HPLC method, quality control samples were prepared, five for each of nine epirubicin concentrations ranging from 0.01 to 100 μg/mL. These samples were assayed on the day of preparation and on the following four consecutive days. The mean regression equation for plasma was y = 0.215x − 0.008 (r2 = 0.999), where y is the peak area ratio and x is the concentration. This equation shows significant linearity (P < 0.01) over the concentration range of 0.01–100 μg/mL. The mean regression equations for bile and tissue homogenates were not significantly different from the equation for plasma. Variations for both precision and accuracy of the inter- and intra-day results never exceeded 15 %. The lower limit of quantification (LOQ) was, therefore, defined as 0.01 μg/mL. The mean absolute recovery of epirubicin was over 96 % (Shin et al. 2013).
I.V. infusion of epirubicin and analysis of its plasma and bile levels
Under light pentobarbital sodium anesthesia, the femoral vein and artery were cannulated with PE-50 polyethylene tubing (Intramedic, Clay Adams, Parsippany, NJ, USA.) for epirubicin administration and blood sampling, respectively. A catheter (PE-10, Intramedic, Clay Adams, Parsippany, NJ, USA) was implanted into the bile duct via a small abdominal incision for bile sampling. Epirubicin was infused through the rat femoral vein at a flow rate of either 10, 20, 40, 80 or 160 μg/min/kg. At designated times, blood and bile samples were collected up to 24 h post infusion.
The blood samples were centrifuged for 15 min at 1,500×g and the plasma was harvested. Immediately after collecting the plasma (100 μL) samples, daunorubicin (10 μL, 50 μg/mL) was added to each plasma test tube as an internal standard. Methanol (3 mL) was then added to precipitate the proteins and extract the compounds of interest. These mixtures were vortexed for 15 min and centrifuged for 15 min at 1,500×g. The supernatants were withdrawn, dried under a stream of dry nitrogen and reconstituted in 150 μL mobile phase for quantitative HPLC analyses. The epirubicin levels in the bile were determined as described above (Shin et al. 2013).
Determination of the liver concentration of epirubicin
The rats were decapitated when the steady-state concentration was reached after continuous i.v. infusion of epirubicin at a flow rate of 10, 20, 40, 80 or 160 μg/min/kg. The liver was immediately removed, blotted onto filter papers, and weighed. The tissues were rinsed in ice-cold 50 mM tris–HCl buffer (containing 0.25 M sucrose, pH 7.4) and homogenized with a glass Potter–Elvehjem-type homogenizer with a Teflon pestle. After extracting 100 μL of 20 % homogenate with 3 mL of methanol, the concentration of epirubicin in the supernatant was measured as described above (Shin et al. 2013).
Preparation of isolated rat hepatocytes
Hepatocytes were isolated from male rats by the procedure of Iga et al. (1979). After isolation, hepatocytes were suspended (1.7 × 106 cell/ml) at 0 °C in the albumin-free Krebs-Henseleit buffer supplemented with 12.5 mM HEPES (pH 7.4). The viability of isolated cells was determined by 0.4 % trypan blue exclusion test. The value obtained usually ranged from 95 to 98 %.
Uptake of epirubicin by isolated hepatocytes
To determine the uptake rate of epirubicin, isolated hepatocytes (1.7 × 106 cells/ml) were incubated at 37 °C with various concentrations of epirubicin. After 5 min of preincubating the cells at 37 °C, an aliquot (50 μl) of epirubicin was added to start uptake. Initial concentrations of epirubicin ranged from 5 to 400 μg/mL. The incubation medium (albumin-free) in the uptake experiment contained 137 mM NaCl, 5.4 mM KCI, 1.25 mM CaCl2, 1.0 mM MgCl2, 0.8 mM MgSO4, 0.5 mM NaH2PO4, 0.4 mM Na2HPO4, 4.2 mM NaHCO3, 10 mM HEPES, and 5 mM glucose (pH 7.4).
An aliquot of the cell suspension (100 μL) was taken at the indicated times (30, 60, 90, 120, 180, 300 and 600 s), and laid on top of a two-phase system in microfuge tubes. The bottom phase consisted of glycerol (100 μL). This was overlaid with 500 μL of silicone mineral oil (density 1.015). The tubes were then centrifuged for 20 s in a table-top microfuge (Beckman Instruments, Fullerton, CA, USA). Three milliliters of methanol was added to the glycerol solution. After centrifugation of the mixtures at 3,000 rpm for 15 min at 4 °C, epirubicin amounts in the organic phase were measured as described above. Amounts taken up by hepatocytes were corrected for the adherent film (2.2 μL/mg protein). Adherent water volume was determined with [14C] inulin and 3H2O (Yamazaki et al. 1992). Protein was determined by protein assay kits (Bio-Rad Co. Ltd., Hercules, CA, USA). Bovine serum albumin was the standard.
Determination of the uptake permeability clearance
The initial uptake rate of epirubicin (vinf) was obtained by regression of the linear portion of the uptake time course (within 2 min). The relationship between initial uptake rate (vinf) and the initial epirubicin concentration in the medium (s) was plotted as an Eadie–Hofstee plot. This plot revealed the straight line, and therefore we fitted the uptake data to a Michaelis–Menten equation with a saturable component.
where Vmax and Km represent the maximum uptake velocity and Michaelis–Menten constant, respectively. The Vmax and Km values were calculated with a nonlinear least squares method. Furthermore, we obtained the permeability-surface area product (PSinf) for epirubicin uptake in vitro, which was calculated as Vmax/Km after converting the Vmax value to that per gram of liver, assuming that 1 mg protein contains 1.1 × 106 cells and 1 g liver contains 1.3 × 108 cells (Yamazaki et al. 1992).
Effect of temperature, various inhibitors or substrates on the uptake rate of epirubicin
Temperature dependency of the epirubicin uptake was measured at 0, 27 and 37 °C. The rate of change of a biological system as a consequence of increasing the temperature (Q10, temperature coefficient) was calculated as: Q10 = (vinf at 37 °C)/(vinf at 27 °C). To investigate the effects of inhibitors on the initial uptake rate of epirubicin, p-chloromercuribenzenesulfonic acid (PCMB, 500 μM, sulfhydryl-modifying agent), 4,4′-diisothiocyanatostilbene-2,2′-disulfonic acid (DIDS, 500 μM, anion exchange inhibitor), rotenone (30 μM, metabolic inhibitor) and carbonyl cyanide p-trifluoromethoxyphenylhydrazone (FCCP, 2 μM, metabolic inhibitor) were tested with the same method of Yamazaki et al. (1993). Various substrates of uptake transporters such as organic anion transporting polypetides (Oatps), organic cation transporters (Octs) and a sodium taurocholate cotransporting polypeptide (Ntcp) were also evaluated: bromosulfophthalein (BSP, 50 μM, Oatp1 and Oatp3 substrate), digoxin (1 μM, Oatp2 substrate), metformin (100 μM, Oct1 substrate), cimetidine (25 μM, Oct2 substrate) and taurocholate (500 μM, Ntcp substrate) (Yamazaki et al. 1993).
Kinetic analysis after i.v. infusion of epirubicin
After epirubicin was infused through the rat femoral vein at a flow rate of 40, 100, 200, 300 or 400 μg/min/kg, the concentrations of epirubicin in the plasma, bile and liver were measured as described above. Biliary clearances based on plasma and liver concentrations of epirubicin (CLbile,plasma, CLbile,liver) were determined as follows
where Vbile is the biliary excretion rate of epirubicin, and Css.plasma and Css.liver represent the plasma and liver concentration of epirubicin, respectively, at steady-state (8 h) after i.v. infusion.
Statistical analysis
The unpaired Student’s t test was used to compare two groups. One-way analysis of variance was used to test for significant differences between multiple groups. Statistical significance was defined as P < 0.05.
Results
Concentration dependency of epirubicin uptake by isolated hepatocytes
Figure 1 shows the time courses of epirubicin uptake by isolated hepatocytes at various concentrations (5–400 μg/mL). The process of epirubicin uptake is linear within 2 min for each concentration, and the initial uptake rate (vinf) for each epirubicin concentration was calculated from the initial slope by linear regression. When the uptake rates were plotted versus the intial epirubicin concentration, a hyperbolic curve was obtained, demonstrating the epirubicin uptake process that increased in a saturated manner (Fig. 2A). A linear transformation of this curve (Eadie-Hofstee plot) yields a straight line (Fig. 2B). The maximal uptake velocity (Vmax) and the Michaelis–Menten constant (Km) were calculated to be 3.70 ± 0.21 (μg/min/106 cells), and 99.1 ± 6.41 μg/mL, respectively.
Time course of uptake of epirubicin into isolated hepatocytes. Hepatocytes (1.7 × 106 cells/ml) were preincubated for 5 min at 37 °C prior to the addition of epirubicin. The initial concentrations were ranged from 5 to 400 μg/mL. Each point represents the mean ± S.E. of three experiments. Keys: (●) 5 μg/mL; (◯) 10 μg/mL; (▼) 25 μg/mL; (▽) 50 μg/mL; (■) 100 μg/mL; (□) 200 μM; (◆) 400 μg/mL
Kinetics of epirubicin uptake in isolated rat hepatoyctes. (A) Plot of initial uptake rate versus epirubicin concentration. (B) Eadie-Hofstee plot of epirubicin uptake into isolated hepatocytes. The iInitial uptake rate was measured within 2 min of incubation, and was calculated by linear regression. Each point represents the mean ± SE of three experiments
Effect of temperature, metabolic inhibitors, sulfhydryl-modifying reagent and anion exchange inhibitor on the initial uptake rate of epirubicin
The epirubicin uptake exhibited remarkable temperature dependency and the initial uptake rate decreased by 57.4 % at 27 °C and 37.3 % at 0 °C (Fig. 3A). The Q10 value was thus calculated as 1.74 (vinf at 37 °C divided by vinf at 27 °C). The uptake decreased greatly after the addition of either a sulfhydryl-modifying reagent (PCMB, 500 μM) or an anion exchange inhibitor (DIDS, 500 μM). PCMB and DIDS inhibited the initial uptake rate of epirubicin by 37.8 and 53.7 % of initial values, respectively. In addition, in the presence of metabolic inhibitors such as rotenone (30 μM) or FCCP (2 μM), initial uptake rate of epirubicin fell to 49.7 and 59.5 % of initial levels, respectively.
Effect of temperature, inhibitors or substrates on the initial uptake velocity of epirubicin (15 μg/mL) by isolated hepatocytes. Each bar represents the mean ± SE of three experiments. *Significantly different from the control group (P < 0.01). (A) Temperatures (27 °C, 0 °C), metabolic inhibitors (FCCP, p-trifluoromethoxyphenylhydrazone, 2 μM; Rotenone, 30 μM), sulfhydryl-modifying reagent (PCMB, p-chloromercuribenzenesulfonic acid, 500 μM) and anion exchange inhibitor (DIDS, 4,4′-diisothiocyanatostilbene-2,2′-disulfonic acid, 500 μM). (B) Organic anion transport substrates (TCA, taurocholate, 500 μM; BSP, bromosulfophthalein, 50 μM; DGX, digoxin, 1 μM) and organic cation transport substrates (metformin, 100 μM; cimetidine, 25 μM)
Inhibition of initial uptake rate of epirubicin by organic anion transport substrates and organic cation transport substrates
We tested effects of various substrates for organic anion transporters and organic cation transporters on the initial uptake of epirubicin into isolated rat hepatocytes (Fig. 3B). TCA (Ntcp substrate) significantly inhibited the initial uptake rate of epirubicin by 54.8 % of the initial value. Moreover, BSP (Oatp1 and Oatp3 substrate) also significantly inhibited the velocity by 51.4 % of the initial value. In contrast, digoxin (Oatp2 substrate), cimetidine (Oct2 substrate) and metformin (Oct1 substrate) slightly reduced the uptake of epirubicin, but its statistical significance was not determined.
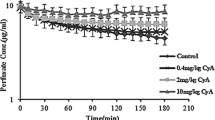
In vivo i.v. infusion studies
After i.v. infusion of epirubicin into rats at flow rates of 10, 20, 40, 80 and 160 μg/min/kg, the plasma concentration and biliary excretion rate were measured. Both parameters reached at steady-state 8 h after i.v. infusion (Fig. 4). We measured the epirubicin concentration at steady-state (8 h) in the plasma (Css,plasma), liver (Css,liver) and bile (Css,bile) after i.v. infusion. The epirubicin concentration ratio at steady-state was obtained by regression of the linear portion of the curve (Fig. 5). The ratios of Css,liver/Css,plasma, Css,bile/Css,liver and Css,bile/Css,plasma were calculated to be 152 ± 9.53, 3.99 ± 0.256 and 513 ± 47.4, respectively. These values indicate that epirubicin accumulated extensively in the liver, followed by excretion into bile. We calculated the biliary excretion clearances based on the plasma (CLbile,plasma) and liver (CLbile,liver) concentrations of epirubicin. The CLbile,plasma and CLbile,liver decreased as Css,plasma and Css,liver increased (Fig. 6). The extent of the CLbile,liver decrease was more pronounced than that of CLbile,plasma.
Plots of Css,liver vs Css,plasma (A), Css,bile vs Css,liver (B), and Css,bile vs Css,plasma (C) of epirubicin after i.v. infusion in rats. The infusion rates were 10, 20, 40, 80 and 160 μg/min/kg. The concentrations of plasma, liver and bile were measured at steady-state after i.v. infusion of epirubicin. Each point represents the mean ± SE of three rats
Discussion
Epirubicin, an antineoplastic drug, is widely used in chemotherapy for hepatocelluar carcinoma. Thus, studies on the efflux process of epirubicin have been widely reported in tumor cells and animal tissues (Hu et al. 1999; Lo 2000, 2003). However, accurate kinetic analyses of the cellular uptake of epirubicin have not been reported. Consequently, in the present study, we have characterized the hepatic uptake of epirubicin by isolated hepatocytes. The uptake process of epirubicin was saturable with a Km of 99.1 μg/mL and Vmax of 3.70 μg/min/106 cells (Fig. 1), which is comparable with Iwakiri’s study (2008). They determined the intracellular drug amount 10 min after incubation by the primary cultured hepatocytes. In the present study, we measured the initial uptake velocity of epirubicin within 2 min after incubation by fresh isolated hepatocytes. As shown in the Eadie–Hofstee plot, the uptake process of epirubicin revealed one saturable component (Fig. 2). Taking into account the fact that therapeutic serum epirubicin concentration is much lower than the Km value (Danesi et al. 2002), the carrier-mediated uptake clearance under linear condition (Vmax/Km) can be calculated to be 37.4 μL/min/106 cells. Based on the reported value, 1 g liver contains 1.3 × 108 cells (Yamazaki et al. 1992), the PSinf value is calculated as 4.86 mL/min/g liver. These analyses suggest that epirubicin might be taken up by hepatocytes via a carrier-mediated system.
The initial uptake velocity of epirubicin was significantly inhibited in a temperature-dependent manner (Fig. 3A), suggesting that epirubicin might depend on energy to be taken up by hepatocytes. Indeed, the epirubicin influx process was substantially inhibited by ATP suppression in hepatocytes. The initial uptake velocity of epirubicin by the hepatocytes was significantly inhibited in the presence of metabolic inhibitors such as rotenone or FCCP (Fig. 3A). Yamazaki et al. (1993) have demonstrated that metabolic inhibitors (rotenone and FCCP) decreased the cellular ATP level rapidly within 1 min to 19 and 15 % of the initial value, respectively. However, 30 or 15 % of the initial value was still maintained after a 30-min incubation with rotenone and FCCP, respectively. In the present study, the initial uptake velocity of epirubicin remained at 46–63 % of the control value (Fig. 3A). The uptake velocity of epirubicin was also significantly reduced after the addition of sulfhydryl-modifying reagent (PCMB) or an anion exchange inhibitor (DIDS) (Fig. 3A). These findings indicated that the uptake of epirubicin might be mediated by the active transport protein in hepatocytes.
Substrates for organic anion transporters such as TCA and BSP significantly inhibited the initial uptake velocity of epirubicin (Fig. 3B). In contrast, statistical significance for epirubicin uptake was not determined after the addition of substrates for organic cation transporters such as cimetidine and metformin (Fig. 3B). Iwakiri’s study (2008) with the cultured hepatocytes demonstrated that the uptake process of epirubicin revealed biphasic profiles, and that the process was slightly reduced by the treatment of organic cation transport inhibitors such as verapamil and tetraethylammonium. However they measured the total intracelluar amount of drug at one time period at the end of the incubation. In the present study, the initial uptake rate (vinf) for each epirubicin concentration was calculated from the initial slope by a linear regression. It is likely that in their study, a one-point determination of the amount of drug taken up was not enough to evaluate the initial uptake velocity by the hepatocytes. However, the major results of Iwakiri’s study (2008) are comparable to the present study, and suggest that inhibiting the transporter involved in the cellular influx of epirubicin mitigated its cytotoxicity. Taken together, the two criteria for carrier-mediated active transport were satisfied in the hepatic transport of epirubicin; one is that metabolic energy is required for epirubicin transport, and the other is that epirubicin was taken up via organic anion transporting polypeptides.
We also attempted to determine the hepatobiliary transport of epirubicin after in vivo i.v. infusion. In our previous study (Shin et al. 2013), epirubicin accumulated selectively into the liver after an i.v. bolus administration in rats, and was mostly excreted into bile. The concentrating process in biliary excretion from the liver might be one reason for the selective accumulation of epirubicin in bile. However, this potential mechanism has not been clarified yet. In the present study, at the steady-state after i.v. infusion of epirubicin, Css,liver was about 152-fold higher than Css,plasma, and Css,bile was about 3.99-fold higher than Css,liver in the linear portion of the curve (Fig. 5), indicating that epirubicin extensively accumulated in the liver, followed by excretion into bile. These findings suggest that both hepatic uptake and biliary excretion of epirubicin are mediated via specific transporters. Recently, we clarified the dose-dependent pharmacokinetics of epirubicin after its i.v. bolus administration in rats (Shin et al. 2013). In the previous study, the CLtot values significantly decreased after i.v. administration with the increase in dose from 2 to 50 mg/kg. The amounts of epirubicin found in the bile by 12 h after its administration of 2–50 mg/kg decreased from 27.9 to 21.5 % of the initial dose, however, the significant differences were not observed (Shin et al. 2013). Unlike the single i.v. bolus administration study (Shin et al. 2013), the CLbile,plasma and CLbile,liver decreased as Css,plasma and Css,liver increased at the steady-state after i.v. infusion of epirubicin (Fig. 6). The extent of the CLbile,liver decrease was more pronounced than that of CLbile,plasma (Fig. 6), suggesting that its saturation in hepatobiliary transport might be mainly responsible for the nonlinearity of the biliary excretion process. Recently, it has been demonstrated that the efflux of the lipophilic antineoplastic drugs from tumor cells were extensively stimulated via transport proteins such as P-glycoprotein (P-gp) and multidrug-resistance associated proteins (MRP) (Nagasawa et al. 1996; Hu et al. 1999; Lo 2000). Therefore, these proteins may play a major role in the biliary excretion of epirubicin from the bile canalicular membrane. In conclusion, present studies using isolated rat hepatocytes and in vivo i.v. infusion demonstrate that epirubicin is likely to be taken into the liver cells via organic anion transporting polypeptides, and that its biliary excretion might be mediated via specific transporters.
References
Berchem, G.J., F. Ries, J. Hanfelt, C. Duhem, M. Keipes, C. Delagardelle, and M. Dicato. 1996. Epirubicin cardiotoxicity: a study comparing low- with high-dose-intensity weekly schedules. Supportive Care in Cancer 4: 308–312.
Danesi, R., F. Innocenti, S. Fogli, A. Gennari, E. Baldini, A.D. Paolo, B. Salvadori, G. Bocci, P.F. Conte, and M.D. Tacca. 2002. Pharmacokinetics and pharmacodynamics of combination chemotherapy with paclitaxel and epirubicin in breast cancer patients. British Journal of Clinical Pharmacology 10: 508–518.
Fujita, H., K. Ogawa, H. Tone, H. Iguchi, T. Shomura, and S. Murata. 1986. Pharmacokinetics of doxorubicin, (2″R)-4′-O-tetrahydropyranyl-adriamycin and aclarubicin. Japanese Journal of Antibiotics 39: 1321–1336.
Hu, X.F., A. Slater, D. Rischin, P. Kantharidis, J.D. Parkin, and J. Zalcberg. 1999. Induction of MDR1 gene expression by anthracycline analogues in a human drug resistant leukaemia cell line. British Journal of Cancer 79: 831–837.
Iga, T., D.L. Eaton, and C.D. Klaassen. 1979. Uptake of unconjugated bilirubin by isolated rat hepatocytes. American Journal of Physiology 10: 9–14.
Iguchi, H., Y. Seryu, T. Kiyosaki, S. Hori, H. Tone, and T. Oki. 1980. Studies on the absorption, excretion and distribution of aclacinomycin A: Absorption, excretion and distribution of 14C- or 3H-aclacinomycin A in mice, rats and rabbits. Japanese Journal of Antibiotics 33: 169–178.
Iwakiri, T., M. Okumura, M. Hidaka, Y. Kumagai, E. Ichihara, Y. Kawano, and K. Arimori. 2008. Inhibition of carrier-mediated uptake of epirubicin reduces cytotoxicity in primary culture of rat hepatocytes. Journal of Applied Toxicology 28: 329–336.
Lo, Y.L. 2000. Phospholipids as multidrug resistance modulators of the transport of epirubicin in human intestinal epithelial Caco-2 cell layers and everted gut sacs of rats. Biochemical Pharmacology 60: 1381–1390.
Lo, Y.L. 2003. Relationships between the hydrophilic-lipophilic balance values of pharmaceutical excipients and their multidrug resistance modulating effect in Caco-2 cells and rat intestines. Journal of Controlled Release 90: 37–48.
Minotti, G., P. Menna, E. Salvatorelli, G. Cairo, and L. Gianni. 2004. Anthracyclines: Molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacological Reviews 56: 185–229.
Nagasawa, K., T. Natazuka, K. Chihara, F. Kitazawa, A. Tsumura, K. Takara, M. Nomiyama, N. Ohnishi, and T. Yokoyama. 1996. Transport mechanism of anthracycline derivatives in human leukemia cell lines: Uptake and efflux of pirarubicin in HL60 and pirarubicin-resistant HL60 cells. Cancer Chemotherapy and Pharmacology 37: 297–304.
Nagata, M., Y. Matsuo, M. Hidaka, Y. Kawano, M. Okumura, J. Tokunaga, N. Takamura, and K. Arimori. 2008. Effect of acute hepatic failure on epirubicin pharmacokinetics after intrahepatic arterial injection in rats. Biological and Pharmaceutical Bulletin 31: 493–496.
Peng, X., B. Chen, C.C. Lim, and D.B. Sawyer. 1993. The cardiotoxicology of anthracycline chemotherapeutics: Translating molecular mechanism into preventative medicine. Molecular Interventions 5: 163–171.
Robert, J. 1993. Epirubicin. Clinical pharmacology and dose-effect relationship. Drugs 45(Suppl. 2): 20–30.
Shin, D.H., S.H. Park, O.-S. Kwon, C.-U. Park, K. Han, and Y.B. Chung. 2013. Validation of high-performance liqid chromatography method to determine epirubicin and its pharmacokinetics after intravenous bolus administration in rats. Journal of Pharmaceutical Investigation 43: 243–249.
Yamazaki, M., H. Suzuki, Y. Sugiyama, T. Iga, and M. Hanano. 1992. Uptake of organic anions by isolated rat hepatocytes: A classification in terms of ATP-dependency. Journal of Hepatology 14: 41–47.
Yamazaki, M., H. Suzuki, M. Hanano, T. Tokui, T. Komai, and Y. Sugiyama. 1993. Na+-independent multispecific anion transporter mediates active transport of pravastatin into rat liver. American Journal of Physiology 264: G36–G44.
Yamazaki, M., H. Suzuki, and Y. Sugiyama. 1996. Recent advances in carrier-mediated hepatic uptake and biliary excretion of xenobiotics. Pharmaceutical Research 13: 497–513.
Yoo, B.I., K.B. Ahan, M.H. Kang, D.C. Moon, O.S. Kwon, H.S. Lee, J.S. Ryu, T.Y. Kim, S. Song, and Y.B. Chung. 2005. HPLC analysis and pharmacokinetic characteristics of 11-hydroxyaclacinomycin X (ID-6105), a novel anthracycline, in rats and beagle dogs. Biological and Pharmaceutical Bulletin 28: 88–693.
Acknowledgments
This work was supported by the research grant of the Chungbuk National University in 2012.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shin, D.H., Park, S.H., Jeong, S.W. et al. Hepatic uptake of epirubicin by isolated rat hepatocytes and its biliary excretion after intravenous infusion in rats. Arch. Pharm. Res. 37, 1599–1606 (2014). https://doi.org/10.1007/s12272-014-0475-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-014-0475-5