Abstract
This study aims to describe baseline characteristics and in-hospital management of a patient cohort hospitalized with acute heart failure (AHF). Adult patients in Denmark admitted with a medical diagnosis during a 7-day period were reviewed for symptoms and clinical findings suggestive of AHF. HFpEF was defined as LVEF ≥ 45%. Of 5194 patients, 290 (6%) had AHF. Sixty-two percent (n = 179) was diagnosed with HFpEF. Compared to HFrEF patients, HFpEF patients were more often women (48% vs. 31%, p = 0.004), less likely to have ischemic heart disease (31% vs. 53%, p = 0.002) and a pacemaker/ICD (7% vs. 21%, p < 0.001/1% vs. 8%, p < 0.001). Fewer HFpEF patients received intravenous diuretics (43% vs. 73%, p < 0.001) and inotropes (2% vs. 7%, p = 0.02), while more HFpEF patients received nitro-glycerine (59% vs. 44%, p = 0.02). Intubation/NIV, ICU admission, and revascularization were used similarly. Hospitalization was shorter for HFpEF patients (4 vs. 6 days, p < 0.001), with no significant difference in survival to discharge (96% vs. 91%, p = 0.07). Of AHF admissions, nearly two-thirds was due to HFpEF. Compared to HFrEF, HFpEF patients had a lower cardiac comorbidity and a 2-day shorter hospitalization.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Heart failure (HF) is known to be a major cause of both morbidity and mortality, with an estimated prevalence of 1–2% in economically developed countries [1,2,3]. An estimation from 2014 suggested that 26 million people worldwide were living with HF [4], and that approximately half of these patients had HF with preserved ejection fraction (HFpEF) [5,6,7]. Studies have indicated an increase in the prevalence of patients with HFpEF, probably due to an ageing population [6]. It is estimated that in Europe, a total of 1–4% of all both medical and surgical admissions in developed countries are caused by HF as the primary diagnosis [8].
Guidelines for the treatment of patients with HF with reduced ejection fraction (HFrEF) are based on several randomized controlled trials [9]. Apart from the EMPEROR-Preserved Trial finding a lower incidence of hospitalization for HF among patients with HFpEF treated with empagliflozin [10], no treatment has yet been proven to significantly and efficiently improve the prognosis in patients with HFpEF [11,12,13,14,15]. A phenotypical heterogeneity in the HFpEF population has been proposed as a reason for studies not being able to confirm a significant effect of different treatment entities [12, 16]. A study of clearly defined subgroups might contribute to target a specific and effective treatment.
The mortality rate for patients with HF is generally high, with a worse prognosis than patients with breast, bowel, or prostate cancer [8]. When comparing mortality rates in patients with HFrEF and HFpEF, the literature is not consistent. It has been suggested that further epidemiological studies characterizing the HFpEF population are important to improve future trial designs and reduce hospitalizations and mortality in patients with HFpEF [5].
The aim of the current DanAHF sub study was to characterize a consecutive cohort of patients with preserved ejection fraction admitted to hospital with acute HF, and more specifically to compare HFpEF and HFrEF in terms of comorbidity, clinical findings, in-hospital treatment, and mortality in a nationwide study in Denmark.
Method
DanAHF Study Design and Data Collection
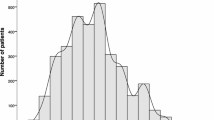
All admissions of adult patients (≥ 18 years) in Denmark with a medical diagnosis during a consecutive 7-day period in 2015 were systematically reviewed. All patient charts were individually assessed for symptoms, clinical findings, and in-hospital treatment and these findings were compared to a prespecified list of symptoms and treatment modalities suggestive of acute HF (Fig. 1). Patients were allocated 1 point for each symptom and treatment, respectively. An accumulated score of ≥ 3 points with at least one point from each category (symptoms or treatment, respectively) was included as a patient with acute HF according to the prespecified study protocol. Patients with acute HF were categorized as HFpEF or HFrEF based on the left ventricular ejection fraction (LVEF) obtained by 2D echocardiography during admission (see below). Patients without an available echocardiography were excluded from the current study (n = 45, 13%). Medication at the time of admission and discharge was registered using patient and medical charts.
Consort diagram and point system used for diagnosing patients with acute heart failure in the DanAHF cohort. *Patients were allocated one point for each sign or treatment found in their journal. Only patients with at least one sign and one treatment were included in the heart failure group. GI, gastrointestinal; NIV, non-invasive ventilation
Definition of HFpEF
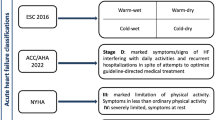
In 2016, the European Society of Cardiology introduced HF with mid-range ejection fraction (now mildly reduced ejection fraction, HFmrEF) in the HF guidelines, defined as LVEF 40–49% [9]. Until then, HF had been subdivided into only HFpEF and HFrEF, reflected in prior clinical trials. In this study, patients with acute HF were categorized in HFpEF defined as LVEF ≥ 45% and HFrEF as LVEF < 45%. This LVEF cut-off was chosen in accordance with the majority of HFpEF clinical trials to date, to ensure comparability between the current study and prior studies. Comparable studies include the TOPCAT Trial (Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist) [13], the PARAGON-HF Trial (Prospective Comparison of ARNI with ARB Global Outcomes in HF with Preserved Ejection Fraction) [12], the I-PRESERVE Trial (Irbesartan in patients with heart failure and PRESERVEd ejection fraction) [17], and the Ancillary DIG Trial (Digitalis Investigation Group) [14].
Statistics
For normally distributed data, continuous variables are presented as mean ± the standard deviation (SD), while non-normally distributed data are presented as median and interquartile ranges (Q1–Q3). Student’s unpaired t-test or Wilcoxon’s rank sum tests were applied to analyze the differences. Categorical variables are presented as number (n) and percentage and chi-square test were applied for the difference analyses. The statistical software SAS 9.4 was used for all analyses. All statistical tests were two-sided, and the significance level was chosen as p < 0.05.
Ethics
The DanAHF study and data collection has been authorized by the Danish Health and Medicines Authorities.
Results
A total of 5194 patients were admitted with a medical diagnosis in Denmark during the prespecified study week. Of them, 335 patients (6.4%) fulfilled the predetermined symptom and treatment criteria for acute HF. An echocardiography was available in 290 patients (87%) and patients with no available echocardiography were excluded from further analyses. A total of 179 patients (62%) were diagnosed with HFpEF and 111 patients (38%) with HFrEF.
Baseline Characteristics
The baseline characteristics for patients with HFpEF and HFrEF are shown in Table 1. Mean LVEF in the HFpEF group and HFrEF group were 56% (± 5%) and 29% (± 9%), respectively. Patients with HFpEF were more often women (48 vs. 31%, p = 0.004), less likely to have a past medical history of ischaemic heart disease (IHD) (31 vs. 53%, p = 0.002), known prior congestive HF (16 vs. 66%, p < 0.001), chronic kidney disease (10 vs. 23%, p = 0.002), and a previously implanted pacemaker or implantable cardiovert defibrillator (ICD) (7% vs. 21%, p < 0.001 and 1% vs. 11%, p < 0.001), compared to patients with HFrEF. In the HFpEF group, 28 of the 179 patients had a past medical history of HF, resulting in 151 new-onset (de novo) HF (84%), compared to 39 de novo HF (35%) in the HFrEF group. Patient with HFpEF and HFrEF was comparable with regard to age (71 vs. 72 years), body mass index (BMI) (28 vs. 27 kg/m [2]), previous history of atrial fibrillation (28% vs. 27%), hypertension (52% vs. 55%), chronic obstructive pulmonary disease (COPD) (23% vs. 19%), and diabetes (23% vs. 29%).
Clinical Presentation
Patient with HFpEF had a significantly higher systolic blood pressure at the time of admission (141 vs. 133 mmHg, p = 0.02) and a significantly lower heart rate (81 vs. 92 beats per minute, p < 0.001) (Table 2). Patients with HFrEF were significantly more likely to have an abnormal ECG, rales on auscultation, jugular vein distension, and a chest X-ray with stasis or cardiomegaly. No significant difference with regard to peripheral edema was found (37% in HFpEF vs. 46% in HFrEF). Patients with HFpEF had lower levels of serum creatinine (83 vs. 100 mmol/L, p < 0.001, normal reference range 60–105 mmol/L) compared to patients with HFrEF, but hemoglobin and lactate levels did not differ significantly. In the HFpEF and HFrEF group, 17 (24%) and 18 (31%) patients respectively had lactate levels > 2 mmol/L.
In-hospital Management
During the index hospital admission, significantly fewer patients with HFpEF were treated with intravenous (IV) diuretics (43% vs. 73%, p < 0.001), and inotropes (2% vs. 7%, p = 0.017) along with a borderline significant tendency towards fewer patients with HFpEF receiving vasopressors (1% vs. 4%, p = 0.051). Nitro-glycerine was more often administered to patients with HFpEF (59% vs. 44%, p = 0.016) (Table 3). Intubation or non-invasive ventilation (NIV) was used equally in both groups (8% vs. 9%, p = 0.84), and there was no significant difference in the percentage admitted to the intensive care unit (ICU) (10% vs. 13%, p = 0.47). The number of coronary angiographies (CAGs) and revascularizations (percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG)) performed during admission did not differ between patients with HFpEF and HFrEF (36% vs. 34% for CAG and 62% vs. 56% for revascularization of the CAGs performed).
Medication
Medication prescribed prior to hospital admission and at hospital discharge is shown in Table 4. Prior to hospital admission, patients with HFpEF were significantly less likely to receive treatment with diuretics (43% vs. 63%, p = 0.001), beta-blockers (38% vs. 59%, p < 0.001), ACE-inhibitors (ACEIs) (20% vs. 32%, p = 0.032), and aldosterone antagonists (MRAs) (5% vs. 16%, p = 0.002), compared to patients with HFrEF. There was no significant difference in the pre-admission treatment with anticoagulants (37% vs. 42%), platelet inhibitors (24% vs. 28%), angiotensin receptor blockers (ARBs) (13% vs. 15%), or COPD inhalers (23% vs. 18%). At discharge, the same tendency was seen with significantly fewer patients with HFpEF receiving diuretics (51% vs. 77%, p < 0.001), beta-blockers (58% vs. 77%, p = 0.001), ACEIs (22% vs. 43%, p < 0.001), and MRAs (10% vs. 27%, p < 0.001).
Comparing medication at admission and at discharge for both patients with HFpEF and HFrEF (Fig. 2), there was a significant increase in the number of patients receiving platelet inhibitors, anticoagulants, diuretics, beta-blockers, and MRAs at discharge. Only patients with HFrEF had a significant increase in ACEIs and digoxin. No significant change was seen regarding amiodarone, calcium channel blockers, ARBs, or COPD inhalers.
Re-admission Rate and Mortality
Patients with HFpEF were generally hospitalized for a shorter period compared to patients with HFrEF, with a median duration of hospitalization of 4 vs. 6 days, respectively (p < 0.001). A trend towards increased in-hospital mortality in the HFrEF group was seen (7 HFpEF (3.9%) vs. 10 HFrEF (9.0%) in-hospital deaths), but no significant difference in survival to discharge was found (96% vs. 91%, p = 0.07).
Comparing medical readmissions for any cause during the first month after discharge, there was no significant difference (20% vs. 26%, p = 0.2). However, during the first year after discharge, patients with HFpEF had a significantly lower readmission rate (43% vs. 57%, p = 0.023). Comparing readmissions with HF as the primary diagnosis, significantly fewer patients with HFpEF were readmitted both within 1 month (3% vs. 14%, p < 0.001) and within 12 months (5% vs. 31%, p < 0.001) after discharge.
Sensitivity Analysis
Of the 335 patients with acute HF, 45 patients had no available echocardiography and could not be included for further analysis. Comparing these 45 patients to the 290 patients with HFpEF/HFrEF, they were 2 years older and more likely to be women (58% vs. 42%, p = 0.04). In the group with missing echocardiography, significantly fewer had a past medical history of atrial fibrillation (12% vs. 27%, p = 0.03), IHD (14% vs. 39%, p = 0.002), and HF (13% vs. 35%, p = 0.005) compared to the HFpEF/HFrEF group. A past medical history of COPD was significantly more common in patients with a missing echocardiography (37% vs. 22%, p = 0.03) and likewise with regard to cancer (21% vs. 10%, p = 0.04). No differences in the past medical history of diabetes, hypertension, stroke, or chronic kidney disease were seen.
Subdividing the 290 patients with acute HF and an available echocardiography into 3 groups instead of 2 results in the following: HFrEF (LVEF < 40%, n = 93), HFmrEF (LVEF 40–49%, n = 43), and HFpEF (≥ 50%, n = 154). Patients with HFpEF had a significantly shorter hospital admission compared to patients with HFmrEF and HFrEF (4 days vs. 7 and 6 days, p < 0.001). There was no significant difference in medical readmission due to any cause within 1 month or 1 year between the groups. There was a significant difference between the groups comparing readmission rate due to HF both within 1 month (HFpEF 2%, HFmrEF 9%, and HFrEF 15%, p < 0.001) and within 1 year (HFpEF 4%, HFmrEF 14%, and HFrEF 32%, p < 0.001).
Discussion
The current nationwide DanAHF study provides a large set of data including all medical admissions in Denmark for an entire week, with more than 5000 patient admissions. A total of 335 was according to predefined symptom and treatment algorithm categorized as acute HF patients. This enables an analysis of a consecutive and unselected cohort of acute HF patients and facilitates an understanding of this complex population in order to optimize future studies in the field. In the DanAHF population, only 32% of the patient had a past medical history of HF meaning that 68% had de novo HF. With a LVEF limit of 45%, a total of 62% of the acute HF patients were diagnosed with HFpEF and 38% with HFrEF, confirming previous large observational studies showing that patients with HFpEF are a frequent cause of acute HF [18,19,20]. Compared to patients with HFrEF, patients with HFpEF had a shorter admission period and a lower rate of readmissions due to HF. Furthermore, there was a nonsignificant tendency towards more patients with HFpEF being discharged alive. Patients with HFpEF were less likely to have a past medical history with IHD, congestive HF, and an implanted pacemaker/ICD, indicating a more favorable pre-admission cardiac status compared to patients with HFrEF. The lower cardiac comorbidity burden may be a reason for the significantly shorter hospital stay for patients with HFpEF.
Most HFpEF studies to date found patients with HFpEF to be older with a higher prevalence of hypertension and atrial fibrillation compared to patients with HFrEF [3, 21]. In the DanAHF population, no significant difference in these parameters was seen. It is well known that comorbidity increases with age, indicating why patients with HFpEF and HFrEF of similar age in the DanAHF population also have the same prevalence of hypertension and atrial fibrillation. Furthermore, a mean age of 71 years among patients with HFpEF in the DanAHF study is similar to the mean age in the meta-analysis MAGGIC [21]. This possibly suggests that the same comorbidity prevalence among patients with HFpEF and HFrEF is more likely due to a higher mean age among patients with HFrEF in the DanAHF population than to a phenotypical different HFpEF population.
The pathophysiology in HFpEF is defined as an abnormal active relaxation of the left ventricle along with increased passive chamber stiffness. As a direct consequence, the patients will exhibit a disproportionate increase in left ventricle filling pressure with an increase in volume or afterload and thus vulnerable to develop pulmonary oedema [22]. Consistent with a higher systolic blood pressure among patients with HFpEF in the DanAHF study. Except for the EMPEROR-Preserved Trial finding a lower incidence of hospitalization for HF among patients with HFpEF treated with empagliflozin [10], no treatment has to date significantly shown to reduce morbidity or mortality. Current treatment options therefore focus on symptoms and comorbidity [9]. It has been suggested that treating especially systolic hypertension plays an important role in patients with HFpEF, and that diuretics improve symptoms of HF irrespective of LVEF [9]. In the current study, it is accordingly seen that diuretics and antihypertensive medication are prevalent among patients with HFpEF.
Clinical Presentation
At hospital admission, patients with HFpEF presented with a significantly higher systolic blood pressure and a lower heart rate compared to patients with HFrEF, indicating two hypotheses: (1) hypertensive pulmonary edema was more common among patients with HFpEF, supported by the higher proportion of patients with HFpEF receiving nitro-glycerine, despite no difference in the number of CAGs performed. (2) Patients with HFrEF had a lower stroke volume, especially when decompensated, supported by the fact that significantly more patients with HFrEF received inotropes during admission. Fewer patients with HFpEF were treated with IV diuretics and were also less likely to have X-ray-verified stasis or cardiomegaly, suggesting less congestion in patients with HFpEF.
It is well known that patients with HFrEF often have abnormal ECGs; this study reveals that it does not apply to patients with HFpEF to the same degree. CAGs were only performed in one-third of the acute HF patients with approximately 60% of them receiving revascularization. This accentuating that the DanAHF population not only included patients with myocardial infarction but also reflects a real-world HF population.
Mortality
Comparing mortality rates in patients with HFpEF and HFrEF, the literature is not consistent. Epidemiological and registry-based studies have reported similar survival in the two groups, but later, a meta-analysis from 2009 demonstrated that mortality in patients with HFpEF was only half the mortality observed in patients with HFrEF [6, 18, 23, 24]. This was later supported in the “Meta-analysis Global Group in Chronic Heart Failure” (MAGGIC) from 2012 including 31 studies and nearly 42,000 patients, showing that patients with HFrEF have a higher risk of death than patients with HFpEF [21]. However, the MAGGIC study also illustrated that initial mortality between HFrEF and HFpEF is comparable, consistent with a non-significant difference in survival to discharge in the current study of the DanAHF population.
Limitations
As any other retrospective study, the DanAHF study is exposed to limitations inherent in observational studies. Inclusion criteria were created with the purpose of identifying a true and unselected population of patients with acute HF, unlike many other studies performed up till now. The diagnosis of HF was established by a review of hospital records, ensuring relevant signs, symptoms, and treatment. However, we cannot out rule that patients with acute HF may have been missed due to a lack of documented information.
ESC Guidelines from 2016 subdivide HF in HFrEF (LVEF < 40%), HFmrEF (LVEF 40–49%), and HFpEF (≥ 50%) [9]. All subgroups should by definition have symptoms of HF that may be accompanied by signs. To fulfil the diagnostic criteria for HFmrEF and HFpEF, natriuretic peptides should be elevated, and/or echocardiographic signs of HF should be present (relevant structural heart disease or diastolic dysfunction). Shortage in these last criteria in the DanAHF study could result in a deficient diagnosis. Furthermore, a potential diversity in echocardiographic measurements could lead to intercenter and interindividual bias.
Of the population with acute HF, 13% had no available echocardiography and could not be included for further analysis. The difference in cardiac comorbidity between the group with a missing echocardiography and the patients with HFpEF/HFrEF could explain why some patients did not have an echocardiography performed. Due to the fact that in a clinical setting, the probability of having an echocardiography performed increases with cardiac comorbidity. Another explanation could be that clinicians due to a history of COPD interpreted symptoms as COPD exacerbations instead of HF and therefore did not perform an echocardiography. Furthermore, an advanced cancer diagnosis could have made an echocardiography inconsequential.
Conclusion
Of acute HF admissions, nearly two-thirds were due to HFpEF. Patients with HFpEF were less likely to have a past medical history with IHD, congestive HF and an implanted pacemaker/ICD, indicating a more favorable pre-admission cardiac status compared to patients with HFrEF. Patients with HFpEF were during admission less frequently treated with IV diuretics and inotropes, indicating a higher stroke volume and less congestion compared to patients with HFrEF. There was no significant difference in the use of intubation/NIV, ICU admissions, or revascularization. Patients with HFpEF had a 2-day shorter admission period, but there was no significant difference in survival to discharge in the two groups. By describing the characteristics of the HFpEF phenotype, this article hopefully both contributes to a clinical awareness of these patients and improves future planning of HFpEF studies in order to develop successful treatment modalities and options.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACEI :
-
ACE-inhibitor
- ARB :
-
Angiotensin receptor blockers
- BMI :
-
Body mass index
- CABG :
-
Coronary artery bypass graft
- CAG :
-
Coronary angiography
- COPD :
-
Chronic obstructive pulmonary disease
- HF :
-
Heart failure
- HFpEF :
-
Heart failure with preserved ejection fraction
- HFrEF :
-
Heart failure with reduced ejection fraction
- ICD :
-
Implantable cardioverter defibrillator
- ICU :
-
Intensive care unit
- IHD :
-
Ischemic heart disease
- LVEF :
-
Left ventricular ejection fraction
- MRA :
-
Aldosterone antagonists
- NIV :
-
Non-invasive ventilation
- PCI :
-
Percutaneous coronary intervention
References
Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007;93(9):1137–46.
Bleumink GS, Knetsch AM, Sturkenboom MCJM, Straus SMJM, Hofman A, Deckers JW, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure - the Rotterdam Study. Eur Heart J. 2004;25(18):1614–9.
Lam CSP, Donal E, Kraigher-Krainer E, Vasan RS. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13(1):18–28.
Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63(12):1123–33. https://doi.org/10.1016/j.jacc.2013.11.053.
Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;03(01):7–11 (Available from: https://www.cfrjournal.com/articles/global-public-health-burden-heart-failure).
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355(3):251–9.
Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function: epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol. 2004;43(3):317–27. https://doi.org/10.1016/j.jacc.2003.07.046.
Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, et al. Heart failure: preventing disease and death worldwide. ESC Hear Fail. 2014;1(1):4–25.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37(27):2129–2200m.
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/34449189).
Borlaug BA. Defining HFpEF: Where do we draw the line? Eur Heart J. 2016;37(5):463–5.
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20.
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation. 2006;114(5):397–403.
Redfield MM, Anstrom KJ, Levine JA, Koepp GA, Borlaug BA, Chen HH, et al. Isosorbide mononitrate in heart failure with preserved ejection fraction. N Engl J Med. 2015;373(24):2314–24.
Flint KM, Shah SJ, Lewis EF, Kao DP. Variation in clinical and patient‐reported outcomes among complex heart failure with preserved ejection fraction phenotypes. ESC Heart Failure. 2020;7(3):811–24.
Forman D, Gaziano JM. Irbesartan in patients with heart failure and preserved ejection fraction. Curr Cardiovasc Risk Rep. 2009;3(5):311–2.
Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure. A Report From the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007;50(8):768–77.
Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) database. J Am Coll Cardiol. 2006;47(1):76–84. https://doi.org/10.1016/j.jacc.2005.09.022.
Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola VP, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: Description of population. Eur Heart J. 2006;27(22):2725–36.
Doughty RN, Cubbon R, Ezekowitz J, Gonzalez-Juanatey J, Gorini M, Gotsman I, et al. The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis: Meta-analysis Global Group in Chronic Heart Failure (MAGGIC). Eur Heart J. 2012;33(14):1750–7.
Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure - abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med. 2004;350(19):1953–9.
Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355(3):260–9.
Somaratne JB, Berry C, McMurray JJV, Poppe KK, Doughty RN, Whalley GA. The prognostic significance of heart failure with preserved left ventricular ejection fraction: A literature-based meta-analysis. Eur J Heart Fail. 2009;11(9):855–62.
Acknowledgements
The authors wish to thank all the nurses, who helped collecting data.
Funding
This work was supported by Novartis, unrestricted grant (F-22963–01).
Author information
Authors and Affiliations
Contributions
ML interpreted the data and drafted the work. ES analyzed the data and revised the work. HS was a major contributor in writing the manuscript. CH and JM substantively revised the work. NK and MGL designed and revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The DanAHF study and data collection has been authorized by the Danish Health and Medicines Authorities.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Associate Editor Jozine ter Maaten oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lassen, M., Seven, E., Søholm, H. et al. Heart Failure with Preserved vs. Reduced Ejection Fraction: Patient Characteristics, In-hospital Treatment and Mortality—DanAHF, a Nationwide Prospective Study. J. of Cardiovasc. Trans. Res. 17, 265–274 (2024). https://doi.org/10.1007/s12265-023-10385-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-023-10385-7