Abstract
Extracorporeal cardiopulmonary resuscitation (eCPR) can improve survival in selected patients with cardiac arrest (CA). In this meta-analysis, we evaluated factors associated with short-term survival and favorable neurologic outcome (FNO) post-eCPR. In June 2019, we systematically searched electronic databases for studies reporting on survival and predictors associated with short-term survival or FNO post-eCPR using multivariable analysis. We meta-analyzed outcomes and predictors using the inverse variance method with a random-effects model. We identified 92 studies with 13 factors amenable to meta-analysis. Pooled short-term survival and FNO were 25% and 16% respectively. Lower lactate, return of spontaneous circulation, shockable rhythm, shorter CPR duration, baseline pH, shorter low-flow time, and history of hypertension were significantly associated with short-term survival. In addition, shockable rhythm, lower lactate, and use of targeted temperature management were associated with FNO. The identified factors associated with short-term survival and FNO post-eCPR could guide prognosis prediction at the time of CA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac arrest (CA) portends a poor prognosis with survival rates of 10% in patients suffering an out-of-hospital CA (OHCA) [1, 2] and 25–40% in the event of an in-hospital CA (IHCA) [3, 4]. Despite the use of conventional cardiopulmonary resuscitation (CPR), only a small proportion of these patients achieve return of spontaneous circulation (ROSC), and even fewer survive to discharge. Of those that survive, many have unfavorable neurologic outcomes [3, 5]. Extracorporeal cardiopulmonary resuscitation (eCPR) by means of veno-arterial ECMO has the potential to restore circulation in patients in whom CPR has been unsuccessful. In matched observational studies, eCPR has demonstrated benefit in improving survival and neurologic outcomes, in comparison to conventional CPR in patients experiencing IHCA and OHCA [4, 6, 7], with a 13% increase in survival and a 14% increase in favorable neurologic outcomes at 30 days compared to CPR [6].
The potential benefit of eCPR should be balanced against its limits. It is important to identify factors that will predict outcomes in this patient population. The current Extracorporeal Life Support Organization (ELSO) [8] guidelines recommend veno-arterial extracorporeal membrane oxygenation (VA-ECMO) in patients with refractory cardiogenic shock but there are no current clear guidelines or consensus criteria for the initiation of VA-ECMO in cardiac arrest. In a meta-analysis that included 16 studies (1162 patients), 8 factors associated with adverse outcomes during eCPR were identified by pooling effect estimates from univariable analysis. This study demonstrated high inconsistency in results across studies that lacked a thorough analysis of study characteristics [9]. Furthermore, older studies have classically only described predictors of survival in patients with eCPR without an evaluation of predictors of neurologic outcomes. Therefore, this systematic review and meta-analysis on contemporary studies identified and summarized the outcomes of short-term survival and favorable neurologic outcome, and independent predictors associated with these outcomes in patients undergoing eCPR. This analysis will provide evidence to facilitate patient selection and address gaps in knowledge to direct future research efforts.
Methods
We prepared this study report based on the PRISMA statement (Appendix A) for.
reporting on systematic reviews and meta-analyses evaluating prognosis or diagnosis [10]. Both the analysis plan and study design were defined prior to study execution. As this study is a.
systematic review and meta-analysis including aggregate data from studies already published,
ethical approval was not required.
Data Sources and Search Strategy
On June 1st, 2019, with the assistance of an experienced research librarian, we conducted a systematic search of electronic databases, specifically Medline, EMBASE, Cochrane, Centre for Reviews and Dissemination, Health Technology Assessment, and NHS Economic Evaluation databases using several related terms: extracorporeal membrane oxygenation and mortality. Three additional studies were identified by searching the references of included publications and previously published meta-analyses.
Study Selection
We included observational cohort studies or post hoc analysis of randomized controlled trials (RCTs) on adults (≥ 18 years) with CA of any etiology reporting on survival and neurologic outcomes and evaluating predictors of survival and/or neurologic outcomes by multivariate analysis, at any time point after VA-ECMO implantation. We included both IHCA and OHCA patients. We included abstracts if they provided sufficient data on the outcomes of interest or predictors. Studies of at least 10 patients and those published in 2010 or later were included to represent more contemporary data. We excluded studies of veno-venous ECMO, VA-ECMO used primarily in cardiogenic shock patients who have not suffered a CA, post-cardiotomy, primary septic shock, or primary respiratory failure. Studies were excluded if they removed patients who died within the first 24 h from their analysis, due to the risk of bias associated with preferential patient selection.
Using a study eligibility form (Appendix B), independent reviewers selected citations by screening titles and abstracts. Citations deemed eligible were included for screening of full-text versions of all articles in duplicate by two independent reviewers. In cases of disagreement, consensus was reached through discussion or participation of a third reviewer.
Data Abstraction
We abstracted data relating to the study and patient population including study design, recruitment time frame, median age, proportion of female patients, creatinine, pH and lactate prior to ECMO implant, etiology of CA, cardiovascular risk factors, location of cardiac arrest (IHCA versus OHCA), bystander CPR, shockable rhythm, targeted temperature management, CPR duration, low-flow time, no flow time, ROSC, survival during short-term follow-up (survival to discharge or 30 day survival), duration of ECMO support, ECMO complications, and neurologic outcomes of survivors. Among included studies, cerebral performance category (CPC) 1 and 2 was deemed as good neurologic recovery, while CPC 3 to 5 was regarded as poor neurologic recovery. We also abstracted data on the predictors associated with survival or good neurologic outcome, including the definition, effect estimate, and confidence intervals.
Risk of Bias Assessment
We performed a risk of bias assessment for each study overall and for each predictor of survival and favorable neurologic outcome, using a QUIPS (Quality in Prognosis Studies) tool [11]. Two independent reviewers appraised the risk of bias based on the domains of study participation, study attrition, prognostic factor measurement, outcome measurement, study confounders, and statistical analysis and reporting. For each domain, the risk of bias was judged as low, moderate, or high. We judged the overall risk of bias as low if all domains were at low risk of bias. Otherwise, the overall risk of bias was judged to be high.
Data Synthesis and Statistical Analysis
Study population characteristics were described using median and interquartile range.
(IQR). We summarized the outcomes of survival and good neurologic outcome as percentages with 95% confidence intervals (CI) and meta-analyzed the outcomes to provide pooled estimates. We meta-analyzed predictors reported in more than 1 multivariate study using a similar definition, evaluating the same outcome, using the inverse variance method with a random-effects model. If a predictor, for example, age, was defined per 10-year increase in age vs. per 1-year increase in age (i.e., unit change), we calculated the OR and corresponding CI associated with the same unit change between the studies so that effect estimates could be pooled. We converted HR to OR, where applicable as previously described [12, 13]. We evaluated inconsistency in results across studies by visual inspection of forest plots. A two-sided p-value of 0.05 or lower was considered statistically significant. Review Manager 5 was used as the statistical platform to conduct our meta-analysis and to create forest plots for graphical representation of meta-analyses. We planned to use funnel plots for representation and assessment of publication bias; however, the small number of studies (< 10 studies) in each meta-analysis precluded its use.
Certainty in the Evidence
To assess the certainty or confidence of pooled effect estimates across all studies reporting on a given predictor, we used the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach to rate the certainty of the evidence as high, moderate, low, or very low; based on risk of bias, imprecision, inconsistency, indirectness, and publication bias [14]. The presence of risk of bias, inconsistency, imprecision, indirectness, and reporting bias were all factors that reduced confidence in the overall body of evidence for a certain predictor. The presence of a large effect (e.g., arbitrarily chosen OR > 1.5 or < 0.7) and gradient response in the case of multi-categorical predictors increased the confidence in effect estimates.
Results
Study Selection and Characteristics
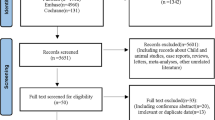
Our systematic search identified 17,305 citations. After screening, a total of 92 studies (52 full text articles and 40 abstracts) on 6793 patients were included (Fig. 1). Of these, 92 studies reported on short-term survival, 61 studies reported on favorable neurologic outcome, 29 studies including 3331 patients reported on 57 predictors and 13 predictors were amenable to meta-analysis.
The baseline characteristics are summarized in Table 1. The median sample size was 74 (IQR 31–101) patients. A minority of patients were female (median 28%, IQR 21–34%) and the median average population age was 56 (IQR 52–60) years. The median frequency of cardiovascular risk factors was 46% (IQR 37–54%) for hypertension, 28% (IQR 21–38%) for smoking, 24% (IQR 16–34%) for diabetes, and 33% (IQR 19–54%) for known history of coronary artery disease.
The frequency of IHCA was 44% (IQR 0–84%). The etiology was myocardial infarction (MI) in nearly half of cases (median 51%, IQR 32–65%) and a coronary angiogram was performed for 86% (IQR 53–100%) of patients. Bystander CPR was performed in a median of 73% (IQR 48–83%) of cases. Cardiac arrest was witnessed in a majority of cases (median 83%, IQR 73–92%). Nearly half of patients presented with a shockable rhythm (median 43%, IQR 35–58%) and only a median of 37% were treated with targeted temperature management (IQR 29–81%). In a vast majority of cases, ROSC was attained (median 80%, IQR 44–94%). The median (IQR) duration of ECMO support was 70 (IQR 45–93) hours.
Risk of Bias of Individual Studies
Of the 92 studies identified overall, 62 performed univariate analysis and were excluded for the meta-analysis. The 30 remaining studies involved multivariate analysis. Of these, 7 studies (23%) were judged to have a high risk of bias, 5 (17%) were judged to have a moderate risk of bias, and 18 (60%) were judged to have a low risk of bias. All studies were retrospective cohort studies. Full text was available for 77% of the studies. The main reason for high risk of bias was related to the use of non-consecutive sampling (5 studies). There was no missing data or loss to follow-up on short-term mortality.
Short-Term Survival and Favorable Neurologic Outcome
Pooled short-term survival was 25% in eCPR patients across multivariate studies (95%CI, 22–28%, Fig. 2) and pooled favorable neurologic outcome was 16% (95%CI, 13–19%, Fig. 3). Meta-regression analysis showed that recruitment year did not explain variation in results across studies for mortality (0.02, 95%CI0.01–0.04) or favorable neurologic outcome (0.01, 95%CI − 0.04–0.02), suggesting no significant changes in event rate over time (Fig. 4, 5).
Factors Associated with Short-Term Survival
A total of 13 potential predictors of short-term survival evaluated in multivariate analysis were meta-analyzed. Table 2 summarizes the characteristics of studies evaluating predictors of outcomes using multivariate analysis in eCPR patients. Figure 6 illustrates the pooled effect estimates of the predictors meta-analyzed. Factors that were significantly associated with improved short-term survival were lower lactate (OR 0.84 per mmol/L increase, 95%CI 0.73–0.98, low confidence, 3 studies), shockable rhythm (OR 3.22, 95%CI 1.43–7.28, high confidence, 7 studies), shorter CPR duration (OR 0.96 per-min increase, 95%CI 0.95–0.98, high confidence, 2 studies), higher baseline pH (OR 8.02, 95%CI 5.97–10.76, high confidence, 2 studies), history of hypertension (OR 1.98, 95%CI 1.18–3.3 moderate confidence, 2 studies), ROSC (OR 10.03, 95%CI 3.45–31.55, moderate confidence, 3 studies), and shorter low-flow time (OR 0.98 per 1-min increase, 95%CI 0.97–0.99, moderate confidence, 3 studies). An OR < 1 suggests a reduction in short-term survival as predictor level increases; an OR > 1 suggests an increase in short-term survival as predictor level increases. Other factors not significantly associated with short-term survival: older age (OR 0.98 per 1-year increase, 95%CI 0.96–1.0 moderate confidence, 7 studies), female sex (OR 2.96, 95%CI 1.00–8.82, moderate confidence, 5 studies), location of arrest (IHCA vs. OHCA) (OR 1.42, 95%CI 0.66–3.04, moderate confidence, 6 studies), revascularization (OR 2.99, 95%CI 0.67–13.29, low confidence, 2 studies), and ACS (OR 2.64, 95%CI 0.79–8.88, low confidence, 2 studies) (Fig. 6, Table 3).
Factors Associated with Favorable Neurologic Outcome
A total of 6 potential predictors of favorable neurologic outcome were reported in multivariate analyses and meta-analyzed. Factors significantly associated with favorable neurologic outcome were shockable rhythm (OR 3.14, 95%CI 1.69–5.81, high confidence, 5 studies), lower lactate (OR 0.91 per mmol/l increase, 95%CI 0.85–0.97, high confidence, 2 studies), and targeted temperature management (OR 4.45, 95%CI 3.58–5.54, moderate confidence, 2 studies). Other factors not significantly associated with favorable neurologic outcome included age per year increase (OR 1.00 per year increase, 95%CI 0.93–1.07, moderate confidence, 2 studies), female sex (OR 1.39, 95%CI 0.44–4.42, moderate confidence, 2 studies), and shorter CPR duration (OR 1.0 per minute increase, 95%CI 0.97–1.02, moderate confidence, 2 studies) (Fig. 6, Table 3).
ECMO Complications
Of the 92 studies included, 44 studies reported on ECMO complications. Requirement for dialysis (median 39%, IQR 29–52%) and multi-organ failure (median 36%, IQR 13–77%) were the most frequently reported complications followed by bleeding (median 36%, IQR 18–48%) and hemolysis (median 32%, median 23–47%). Other reported complications include peripheral vascular complications (median 11.2%, IQR 4.3–20%) and stroke/transient ischemic attack (11%, IQR 3–20%).
Discussion
In this meta-analysis of 92 studies including 6836 patients, the pooled estimate of short-term survival was 30% and favorable neurologic outcomes was 18% in patients who had a CA (both IHCA and OHCA), treated with VA-ECMO. These event rates have remained stable over time. Lower lactate, the presence of a shockable rhythm, shorter CPR duration, higher pH, history of hypertension, shorter low-flow time, and ROSC were factors associated with improved short-term survival while shockable rhythm, lower lactate, and use of targeted temperature management (TTM) were factors associated with favorable neurologic outcomes. Age and sex were not associated with outcomes.
Relation to Previous Work
Advances in therapies have improved the outcomes in patients with CA though survival rates remain low; 10% in an OHCA and 25–40% in the event of an IHCA. [1,2,3,4]. These improvements are not seen uniformly. Between 2006 and 2013, in patients experiencing an OHCA, survival to hospital discharge doubled (4.8 to 9.4%; P < 0.0001), and survival with good neurologic outcome increased (6.2 to 8.5%; P = 0.005) [15]. Furthermore, results from the Resuscitation Outcomes Consortium demonstrated similar findings with survival rates increasing from 8.2 to 10.4% [1]. On the other hand, reports in patients with IHCA have similarly shown that survival to discharge has increased from 3.7% in 2000 to 22.3% in 2009 and rates of clinically significant neurologic disability have decreased over time with a risk-adjusted rate of 32.9% in 2000 and 28.1% in 2009 [16]. Functional and neurologic outcomes are of the utmost importance when predicting patient prognosis and when considering a very resource-intensive and costly intervention such as VA-ECMO [17]. This underlines the importance of identifying predictors that determine not only who will survive, but also who will have a good functional recovery. Conventional CPR can provide 25 to 30% of baseline cardiac output [18] whereas eCPR can provide 60–80% of resting cardiac output, which is sufficient to perfuse all organs, including the brain [19, 20]. Thus, rapid initiation of VA-ECMO in selected candidates is key to increase the chance of favorable neurologic outcomes.
In the only published RCT reporting standard CPR versus eCPR use in 30 patients with OHCA, 43% of the eCPR group, compared to only 7% of the standard CPR group, survived to hospital discharge [21]. In this study, all patients who survived had a favorable neurologic outcome. This study was stopped early due to the significant benefit demonstrated. Patients in the intervention arm supported with eCPR showed higher rates of survival compared to our meta-analysis (43% vs 25%) as well as neurologic recovery (43% vs 16%), which may be due to best practices at a center of excellence, the contemporary nature of the data or possibly a refined patient population.
In our meta-analysis, we found that shockable rhythm is significantly associated with more than twice the odds of short-term survival (OR 2.18, 95%CI 1.03–4.62) post-CA. This is congruent with the literature on CA survival dichotomized by shockable vs non-shockable rhythms. The American Heart Association’s Resuscitation Registry of 45,567 patients (2001–2011) with IHCA reported unadjusted 1-year survival rates of 6.2% in those with a non-shockable rhythm and 21.8% in those with a shockable rhythm [22]. There was significant inconsistency of the effect estimate between studies which may be explained by the fact that the comparator used in the different studies (e.g., asystole or non-shockable rhythm or other) varied in definition.
An increase of 1 min in CPR duration was associated with a relative 4% decrease in survival. This finding is in keeping with the published literature which quotes a survival of < 5% in OHCA patients after 20 min of CPR and < 1% in OHCA patients after 30 min of CPR [23]. As low-flow time (during CPR) increases, end-organ dysfunction ensues, pH drops, and the chances of cardiac recovery are lower [24]. A higher pH was associated with a significant increase in survival (OR 8.02, 95%CI 5.97–10.76). Mechanistically, a lower pH correlates with the length of time in cardiogenic shock, as described by the Society for Cardiovascular Angiography and Interventions scoring system [25].
Patients on VA-ECMO, who had ROSC after CA, had 10 times the odds of short-term survival. This could be explained by the fact that patients who attain ROSC are illustrating signs of regained cardiac function and thus potential recovery. The three studies meta-analyzed for ROSC had varying definitions of this factor including: “any ROSC during ACLS [26], any ROSC before eCPR [27], signs of life before eCPR [28].” The study with the most liberal definition of ROSC (any ROSC during ACLS) had the smallest risk estimate, suggesting that the meta-analysis effect estimate is conservative.
Despite a positive association in prior published studies [29], our meta-analysis did not find a significant relationship between location of arrest (IHCA vs OHCA) and short-term survival (OR 1.42, 95%CI 0.66–3.04). One of the hypotheses for the favorable survival in IHCA is the shorter cannulation time for IHCA vs OHCA. However, the study by Dennis et al. specifically compared cannulation time between IHCA and OHCA, with no significant difference, which would reduce the impact of location on survival between these two groups [30]. Moreover, patients with OHCA were significantly younger (median age 56, IQR 49–64; 77 patients) as compared to IHCA patients (median age 68, IQR 58–73, p < 0.01) and had a higher percentage of shockable rhythms (VF 49% vs 26%, p = 0.04), which would favor better outcomes in this group. Moreover, patients admitted to hospital who then suffer a CA tend to have more comorbidities, which may increase their risk of mortality. Finally, the median rate of bystander CPR across studies was very high at 73%, which is greater than the current rate in North America (45% as per the American Heart Association). These findings could have mitigated the expected survival benefit of IHCA over OHCA in this meta-analysis.
A shorter low-flow time was significantly associated with short-term survival in this meta-analysis (OR 0.98, 95%CI 0.97–0.99). This is congruent to prior reports whereby low-flow time was associated with survival [29]. In a contemporary eCPR tool developed by Ryu et al., low-flow time (CPR duration) > 30 min was one of the strongest predictors of poor outcome [31].
CPR duration was not associated with FNO. Since low-flow time has been previously associated with survival, patients with prolonged low-flow time may not survive at all, making neurologic assessment irrelevant.
Implications for Clinical Practice
Given the scarcity of RCTs evaluating the outcomes in patients with CA and VA-ECMO with one RCT published to date [21], our study identified predictors that can optimize patient prognostication following eCPR. This is particularly important as patients can have a wide range of neurologic outcomes post eCPR. Both factors associated with favorable neurologic outcomes identified in our study, shockable rhythm and the use of TTM, have been shown in prior studies to portend a favorable outcome [32, 33]. Despite the contemporary nature of our study selection, neurologic outcomes were only reported in 43% of studies. Reporting of neurologic outcomes in trials evaluating patients with VA-ECMO has increased but the paucity of predictors for favorable neurologic outcomes compared to those for survival likely stems from a delay in reporting. Larger RCTs are needed to evaluate the impact of VA-ECMO on survival and neurologic outcomes in patients with cardiac arrest given the poor prognosis despite current therapies. These studies can help identify predictors and assist with the development of prediction models from high-quality evidence. While awaiting a large RCT, large multicenter registries and data from meta-analyses, such as this one, can identify patients who may have increased rates of survival or good neurologic outcomes post eCPR. There are currently several ongoing RCTs evaluating eCPR in cardiac arrest patients. The largest being the INCEPTION trial, which is a multicenter RCT that evaluates the effect of eCPR on survival and neurologic outcomes in patients in refractory OHCA presenting with ventricular fibrillation or tachycardia [34]. Other trials include Emergency Cardiopulmonary Bypass for Cardiac Arrest (ECPB4OHCA), NCT01605409.
Limitations
There are several limitations to our study. All of the data collected was observational and retrospective in nature. We attempted to mitigate confounders associated with these types of studies by utilizing data from only multivariate models in our analysis. Even with these attempts, we identified several articles that derived their multivariate data from using only univariate predictors that were determined to be significant. Due to the limited number of studies per predictor (on average 2–7 studies), especially with predictors of favorable neurologic outcomes, we could not evaluate for potential publication bias. This could, as a result, lead to effect overestimation. Furthermore, we pooled different definitions of short-term survival together (including both survival to discharge and 30-day survival) due to the limited studies and varied definitions in the literature available, which prevented us from being able to assess mortality at specific time points. However, we performed a subgroup analysis of studies looking at 30-day survival (74% median survival, IQR 63–38%) vs survival to discharge (73% median survival, IQR 63–81%) which showed no significant difference in mortality estimates; therefore, we pooled studies together.
Conclusion
This meta-analysis identified several factors associated with short-term survival and favorable neurologic outcomes in patients treated with eCPR for both IHCA or OHCA. These factors are important prognostically as they can guide clinical decision-making amongst this population of patients with historically poor prognosis. Further research evaluating the combined prognostic value of these factors along with large RCTs evaluating eCPR benefit based on patient characteristics are required to create and validate predictive models and evaluate their impact on guiding patient care.
Change history
15 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12265-022-10234-z
Abbreviations
- AMI:
-
Acute myocardial infarction
- CA:
-
Cardiac arrest
- CPR:
-
Cardiopulmonary resuscitation
- CS:
-
Cardiogenic shock
- ELSO:
-
Extracorporeal Life Support Organization
- IHCA:
-
In-hospital cardiac arrest
- QUIPS:
-
Quality in Prognosis Studies
- MCS:
-
Mechanical circulatory support
- OHCA:
-
Out of hospital cardiac arrest
- ROSC:
-
Return of spontaneous circulation
- TTM:
-
Targeted temperature management
- VA-ECMO:
-
Veno-arterial extracorporeal membrane oxygenation
References
Daya, M. R., Schmiker, R. H., Zive, D. M., et al. (2015). Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation, 91, 108–115.
Neumar, R. W. (2016). Doubling cardiac arrest survival by 2020. Circulation, 134, 2037–2039.
Benjamin, E. J., Viran, S.S., Callaway, C.W., et al. (2018). Heart disease and stroke statistics - 2018 update: A report from the American Heart Association. Circulation vol, 137.
Twohig, C. J., Singer, B., Grier, G., et al. (2019). A systematic literature review and meta-analysis of the effectiveness of extracorporeal-CPR versus conventional-CPR for adult patients in cardiac arrest. Journal Intensive Care Society., 20, 347–357.
Andersen, L. W., Holmberg, M. J., Berg, K. M., et al. (2019). In-hospital cardiac arrest. HHS Public. Access, 321, 1200–1210.
Ouweneel, D. M., Schotborgh, J. V., Limpens, J., et al. (2016). Extracorporeal life support during cardiac arrest and cardiogenic shock: A systematic review and meta-analysis. Intensive Care Medicine., 42, 1922–1934.
Ahn, C., Kim, H., Cho, Y., et al. (2016). Efficacy of extracorporeal cardiopulmonary resuscitation compared to conventional cardiopulmonary resuscitation for adult cardiac arrest patients: A systematic review and meta-analysis. Scientific Reports, 6, 1–8.
ELSO. (2017). Guidelines for cardiopulmonary extracorporeal life support. ELSO Guidelines, 1–26.
Wang, J., Ma, Q., Zhang, H., et al. (2018). Predictors of survival and neurologic outcome for adults with extracorporeal cardiopulmonary resuscitation: A systematic review and meta-analysis. Medicine (Baltimore), 97(48), e13257. https://doi.org/10.1097/MD.0000000000013257
Moher, D., Libearati, A., Tetzlaff, J., et al. (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336–341.
Hayden, J. A., van der Windt, D. A., Cartwright, J. L., et al. (2013). Assessing bias in studies of prognostic factors. Annals of Internal Medicine, 158(4), 280–286.
Grant RL. (2014). Converting an odds ratio to a range of plausible relative risks for better communication of research findings. British Medical Journal, 348:f7450.
Tierney, J. F., Stewart, L. A., Ghersi, D., et al. (2007). Practical methods for incorporating summary time-to-event data into meta-analysis. Trials, 8, 16.
Iorio, A., Spencer, F.A., Falavigna, M., et al. (2015). Use of GRADE for assessment of evidence about prognosis: Rating confidence in estimates of event rates in broad categories of patients. British Medical Journal, 350:h870
Buick, J. E., Drennan, I. R., Scales, D. C., et al. (2018). Improving temporal trends in survival and neurological outcomes after out-of-hospital cardiac arrest. Circulation Cardiovascular Quality Outcomes, 11(1), e003561. https://doi.org/10.1161/CIRCOUTCOMES.117.003561
Girotra, S., Nallamothu, B. K., Spertus, J. A., et al. (2012). Trends in survival after in-hospital cardiac arrest. New England Journal of Medicine, 367(20), 1912–1920.
Mulaikal, T. A., Nakagawa, S., Prager, K. M., et al. (2019). Extracorporeal membrane oxygenation bridge to no recovery. Circulation, 139, 428–430.
Barsan, W. G., Levy, R. C., et al. (1981). Experimental design for study of cardiopulmonary resuscitation in dogs. Annals of Emergency Medicine, 10, 135–137.
Belohlavek, J., Huptych, M., Svoboda, T., et al. (2012). Coronary versus carotid blood flow and coronary perfusion pressure in a pig model of prolonged cardiac arrest treated by different modes of venoarterial ECMO and intraaortic balloon counterpulsation. Critical Care, 16, R50.
Chung, M., Shiloh, A.L., Carlese, A et al. (2014). Monitoring of the adult patient on venoarterial extracorporeal membrane oxygenation. Scientific World Journal, 393258–10.
Yannopoulos, D., Raveendran, G., Walser, E. ,et al. (2020). Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled trial. Lancet. Published Online November 13, 2020 10.1016/ S0140–6736(20)32338–2
Thompson, L. E., Chan, P. S., Tang, F., et al. (2018). American Heart Association’s Get With the Guidelines-Resuscitation Investigators. Long-term survival trends of Medicare patients after in-hospital cardiac arrest: Insights from Get With The Guidelines-Resuscitation. Resuscitation, 123, 58–64.
Goto, Y., Maeda, T., Funada, A., et al. (2015). Duration of resuscitation efforts and survival after out-of-hospital cardiac arrest: An observational study. European Heart Journal, 36, 192.
Lemkes, J. S., Janssens, G. N., van der Hoeven, N. W., et al. (2019). Coronary angiography after cardiac arrest without ST-segment elevation. New England Journal of Medicine, 380(15), 1397–1407.
Baran, D. A., Grines, C. L., Bailey, S., et al. (2019). SCAI clinical expert consensus statement on the classification of cardiogenic shock. Catheterization and Cardiovascular Interventions, 94, 29–37.
Han, K. S., Kim, S. J., Lee, E. J., et al. (2019). Experience of extracorporeal cardiopulmonary resuscitation in a refractory cardiac arrest patient at the emergency department”. Clinical Cardiology, 42(4), 459–466. https://doi.org/10.1002/clc.23169
Lee, S. W., Park, J. S., Lee, J. S., et al. (2017). Prognostic indicators of survival and survival prediction model following extracorporeal cardiopulmonary resuscitation in patients with sudden refractory cardiac arrest. Annals of intensive care, 7, 187. https://doi.org/10.1186/s13613-017-0309-y
Lamhaut, L., Bougouin, W., Soldan, M., et al. Abstract 113 (2012): ECLS implementation by emergency-intensivist physician for refractory cardiac arrest. Circulation vol 126:A113
Wengenmayer, T., Rombach, S., Ramshorn, F., et al. (2017). Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Critical Care. June 21(1):157.
Dennis, M., McCanny, P., D’Souza, M., et al. (2017). Extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest: A multicentre experience. International journal of cardiology, 231, 131–136. https://doi.org/10.1016/j.ijcard.2016.12.003
Ryu, J. A., Chung, C. R., Cho, Y. H., et al. (2019). Neurologic outcomes in patients who undergo extracorporeal cardiopulmonary resuscitation. Annals Thoracic Surgery, 108, 749–755.
Holzer, M., et al. (2002). Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. The New England Journal of Medicine, 346(8), 549–556.
Daou, O., Winiszewski, H., Besch, G., et al. (2020). Initial pH and shockable rhythm are associated with favorable neurological outcome in cardiac arrest patients resuscitated with extracorporeal cardiopulmonary resuscitation. Journal Thoracic Disease, 12(3), 849–857.
Bol, M. E., Suverein, M. M., Lorusso, R., et al. (2018). Early initiation of extracorporeal life support in refractory out-of-hospital cardiac arrest: Design and rationale of the INCEPTION trial. American Heart Journal, 210, 58–68. https://doi.org/10.1016/j.ahj.2018.12.008
Funding
Dr. Billia receives funding by the Canadian Institutes for Health Research Clinician-Scientist Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval.
No human studies were carried out by the authors for this article. No animal studies were carried out by the authors for this article.
Competing Interests
Dr. Vivek Rao is a consultant to Medtronic, Gore, and Abbott; serves on the Surgical Advisory board to Medtronic; and has an equity interest in Medtronic (minor < $25 k). The rest of the authors have no disclosures to state.
*Median and IQR values reported unless otherwise stated. Values reported represent the median of values taken from each study unless otherwise stated. **Population type unknown in 6 studies.
A. Too few: too few studies to interpret Funnel Plots.
B. Large effect defined as: OR > 1.5 or OR < 0.7.
C. *Although serious risk of bias on initial assessment, there was no significant difference between studies with high risk of bias and those without, thus risk of bias conclusion was “not serious.”
D. Imprecision was deemed serious if the 95%CI overlapped 1.
E. Inconsistency was judged based on similarity of point of estimates, extent of overlap of confidence intervals, and statistical criteria including tests of heterogeneity and I2.
F. Age (per year increase); CPR duration (per minute increase); Low-flow time (per minute increase); pH (mean baseline); Lactate (per 1 mmol/L increase); Hypertension (history of).
Additional information
Associate Editor Navin Kumar Kapur oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mia Bertic and Mali Worme are co-first authors.
Filio Billia and An a C Alba are co-senior authors.
The original version of this article was revised: An incorrect version of Table 2 was presented in this article as originally published and has been replaced.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bertic, M., Worme, M., Foroutan, F. et al. Predictors of Survival and Favorable Neurologic Outcome in Patients Treated with eCPR: a Systematic Review and Meta-analysis. J. of Cardiovasc. Trans. Res. 15, 279–290 (2022). https://doi.org/10.1007/s12265-021-10195-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-021-10195-9