Abstract
Acute pulmonary embolism (APE) is a common sudden venous thromboembolism with high rates of morbidity and mortality. Several studies have concluded that microRNA-134 could be a potential biomarker for APE. However, the sensitivity of these studies varies widely. This study aimed to evaluate the diagnostic value of circulating microRNA-134 levels for APE. Four databases were searched to retrieve articles focusing on microRNA-134 detection in APE diagnosis. The Quality Assessment of Diagnostic Accuracy Studies-2 was used to evaluate the quality of the included literature. This meta-analysis included seven studies and 383 subjects. The microRNA-134 levels in APE patients were higher than those in controls (SMD = 2.84, z = 3.69, p < 0.001). The pooled sensitivity, specificity, and diagnostic odds ratio were 0.86 (0.72–0.94), 0.75 (0.66–0.82), and 19 (7–51), respectively. The positive and negative likelihood ratios were 3.4 (2.4–4.8) and 0.18 (0.08–0.40), respectively. The area under the summary receiver operating characteristic curve was 0.81 (0.77–0.84). Circulating microRNA-134 may be a new biomarker for the diagnosis of APE, but more tests and studies are needed to further explore and prove this. Trial registration number: PROSPERO registration #CRD42020184072
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute pulmonary embolism (APE) is a common sudden venous thromboembolism with high rates of morbidity and mortality [1]. Acute myocardial infarction, stroke, and APE rank first, second, and third, respectively, in terms of death from cardiovascular disease, and APE causes about 60,000 to 100,000 deaths every year in the USA, which implies that there are 100 to 200 APE cases in every 100,000 persons [2,3,4]. Due to the different clinical manifestations and severity of APE and the lack of specificity, the associated rates of misdiagnosis, missed diagnosis, and mortality are high. Therefore, early and accurate diagnosis is an effective method to reduce the incidence and mortality of APE. The methods of diagnosing pulmonary embolism mainly include imaging examinations and biomarkers. The currently accepted gold standard is pulmonary angiography, which is an invasive test that may cause serious complications [5]. In recent years, CT pulmonary angiography has become more widely used. It is the preferred diagnostic method for patients with suspected high-risk pulmonary embolism and plays an important role in the differential diagnosis and treatment of pulmonary embolism [6,7,8]. D-dimer, as a biomarker, is also widely measured in the diagnosis of pulmonary embolism. The test has high sensitivity and poor specificity, and it can effectively exclude patients with pulmonary embolism, but patients with positive results still require imaging examinations [9, 10]. Early and accurate diagnosis can make the patient be treated more effectively and reduce the mortality. Therefore, it is important to find a safe and efficient diagnostic method and improve the accuracy of pulmonary embolism diagnosis.
microRNAs are endogenous non-coding small-molecule single-stranded RNAs that can inhibit the translation of target mRNAs by specific binding to the 3′ non-coding regions of target genes in order to regulate them. Circulating microRNAs have significance as molecular biomarkers for the diagnosis of a variety of diseases [11]. Circulating microRNAs have a variety of advantages as potential biomarkers for the diagnosis of APE. In terms of disease development, some microRNAs are activated and exist at different levels between those with and without disease. Circulating microRNAs are stable, resistant to enzymes and heat, not easily decomposed, and easy to collect and reproduce. They can enter the blood through the peripheral circulation, and they can quickly be detected in the plasma or serum. Detection is sensitive and quantitative, so it is possible to identify a disease in the early stage and assess the severity of the disease according to microRNA levels. Furthermore, compared with pulmonary angiography and D-dimer tests, microRNA detection is not invasive and can be easily accomplished by using real-time quantitative polymerase chain reaction (PCR) at low cost. In addition, microRNA detection possesses high sensitivity and specificity. It can also accurately identify APE and non-ST segment elevation myocardial infarction (NSTEMI), which are two diseases that are hard to differentiate [12]. However, some cells secrete many kinds of microRNAs, and other cells can secrete the same microRNAs, which may make it difficult to distinguish the source of the target microRNA. Single microRNAs may not have good representativeness, and diagnostic accuracy is not very high. It may be useful to screen APE-related differentially expressed genes by gene sequencing and confirmed their product reference ranges and thresholds. The combined detection of several specific microRNAs can also increase diagnostic accuracy. In brief, microRNA has the potential to be an early diagnostic method. Previous research involving three studies combined four different microRNAs (miR-134, miR-1233, miR-28-3p, and miR-27a) inappropriately to evaluate the overall diagnostic value of microRNAs for APE, and it was concluded that microRNAs had good accuracy and could be potential biomarkers for APE; however, the study did not assess the diagnostic value of single microRNAs for APE [13]. The present study aims to estimate the value of a single microRNA for APE diagnosis. Circulating microRNA-134 is the first microRNA used for APE diagnosis, and it is also the most widely studied microRNA to date [14]. Xiao was the first to use microRNA-134 for APE diagnosis and found that compared with controls, miR-134 levels in APE patients were observably higher, suggesting that miR-134 could be used as a biomarker for APE [15]. Other studies have arrived at the same conclusion [12, 16,17,18,19]. However, the sensitivity of these studies varied widely, with a maximum sensitivity of 100% and a minimum sensitivity of 68.8%. In addition, these studies were limited by small sample sizes. Thus, the accuracy of miR-134 tests for APE diagnosis is still not clear. Therefore, the purpose of this study is to investigate the diagnostic value of miR-134 detection for APE by means of a meta-analysis, combining existing studies on miR-134 detection in the diagnosis of APE.
Methods
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses of Diagnostic Test Accuracy (PRISMA-DTA) [20]. A relative protocol has been registered on PROSPERO (ID: CRD42020184072). This study did not need ethical approval because it was a review of existing literature and did not use any individual patient data.
Data Sources and Retrieval Strategy
The PubMed, Web of Science, WanFang, and China National Knowledge Infrastructure databases were searched to retrieve relevant articles focusing on microRNA-134 detection and APE diagnosis. Retrieval ended on April 30, 2020. We retrieved articles published since 1990 from the China National Knowledge Infrastructure, WanFang, and Web of Science databases and since 1960 from the PubMed database. The search terms included “microRNA,” “miRNA,” “miR,” “RNA,” “pulmonary embolism,” “embolism, pulmonary,” “pulmonary thromboembolism,” “thromboembolism, pulmonary,” and “embolism.”
Inclusion and Exclusion Criteria
This study aims to evaluate the diagnostic value of miR-134 detection alone in APE. The inclusion criteria were as follows: (1) the subjects were patients with APE diagnosed by CT pulmonary angiography; (2) the studies contained relevant indicators for the diagnosis of APE via miR-134 detection; and (3) the studies were diagnostic tests. The exclusion criteria were as follows: (1) the studies combined the detection of miR-134 with the detection of different microRNAs or other biomarkers; (2) the studies lacked relevant data for analysis; (3) the studies examined non-human subjects; and (4) the studies were repeat studies, reviews, abstracts, or conference reports.
Data Extraction and Quality Assessment
Two authors (Yu Liu and Ming Xie) separately extracted the data, and all disagreements were resolved by discussion to avoid bias. The main extracted information included the first author, publication time, type of disease and control, sample size, sample type, and average age of the subjects. The collected data included sensitivity, specificity, true positive (tp), false positive (fp), false negative (fn), true negative (tn), and the area under the curve (AUC). The Quality Assessment of Diagnostic Accuracy Studies-2(QUADAS-2) was used to evaluate the quality of the included literature [21]. QUADAS-2 consists of four domains: (1) patient selection; (2) index text; (3) reference standard; and (4) flow and timing. Each domain has several signature questions which are answered as “yes,” “no,” or “unclear,” and the risk of bias is determined as “high,” “unclear,” or “low,” through the signature questions. “Yes” means that the risk of bias is low. If all the signature questions for a domain are answered with “yes,” then the risk of bias of the domain is low. If the answer to any of the signature questions is “no,” then there exists a high risk of bias. Concerns about applicability are judged by the degree that the included studies do not match the review questions and are rated as “low,” “high,” or “unclear.” The risk of bias and applicability can be answered as “unclear” when there is not enough information.
Statistical Analysis
RevMan 5.3 and Stata 14.0 were used for statistical analysis. (1) The data extracted were aggregated to obtain the pooled sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and diagnostic odds ratio (DOR), and the AUC was calculated by using the bivariate mixed effects model. It was also necessary to analyze miR-134 levels and subgroup analysis for the sample type was performed. Sensitivity analysis was carried out by using the method of removing included articles one by one. (2) Heterogeneity among the studies was evaluated by using χ2 and I2 tests. For the diagnostic accuracy study, the Spearman correlation coefficient between the logarithm of (1-SPE) and the logarithm of SEN was calculated to evaluate whether there was a threshold effect between studies [22]. If the Spearman correlation coefficient was > 0 and the p value was < 0.05, there was a threshold effect in the study, so the single index of each study could not be combined. Otherwise, if the Spearman correlation coefficient was < 0 and the p value was > 0.05, there was no threshold effect, and the heterogeneity was mainly derived from the non-threshold effect. When I2 was < 50% or the p value was > 0.1, the homogeneity was considered to be good, and the fixed effects model was adopted. The random effects model was adopted when the test results had heterogeneity. (3) A Deeks’ funnel plot was drawn to assess publication bias. A p value of < 0.05 was considered statistically significant (two-sided test).
Results
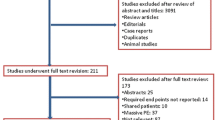
A total of 404 articles were retrieved at the initial stage. After screening, seven articles with 209 APE patients and 174 controls were included in the systematic review, including four in English and three in Chinese [12, 15,16,17,18,19, 23]. The screening process is shown in Fig. 1. The basic information of the included studies is shown in Table 1. All patients were diagnosed with APE by CT pulmonary angiography, and relative miRNA-134 levels in the blood were detected by using real-time quantitative PCR. Table 2 presents the miR-134 levels between the APE patients and controls. The accuracy of microRNA-134 detection for APE diagnosis is shown in Table 3.
Study Quality Assessment
The quality assessment of the included studies was evaluated according to QUADAS-2(Fig. 2). The patient selection and index test domains showed that a high risk of bias existed. Concerning risk of bias, the articles selected confirmed APE patients as study subjects and excluded suspected APE patients and patients for whom APE was difficult to identify. This may overestimate the diagnostic accuracy. Furthermore, the case-control design was not avoided, and the index test was conducted with knowledge of the reference standard results, which could have affected the interpretation of the results and caused potential bias. In addition, it was not explicitly reported whether the threshold was prespecified, and there was an appropriate interval between the index test and reference standard. Threshold selection affects sensitivity and specificity. The time interval between the index test and reference standard is also important, as microRNA levels vary over time. There were no applicability concerns in terms of the patient selection, index test, and reference standard domains. All studies used real-time quantitative PCR to measure miR-134 levels and applied CT pulmonary angiography as the reference standard.
miR-134 Levels
miR-134 levels were available in five studies [16,17,18,19, 23]. Since I2 was 94.7% and the p value was < 0.001, the random effects model was used to perform the analysis, which demonstrated that the miR-134 levels in APE patients were higher than those in controls (SMD = 2.84, 95% CI: 1.33–4.34, z = 3.69, p < 0.001) (Fig. 3a). To determine whether the type of sample could affect miR-134 content, we performed subgroup analysis, which showed that both plasma and serum miR-134 levels in APE patients were always higher than those in controls (Fig. 3b).
Diagnostic Meta-analysis
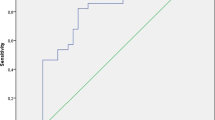
The forest plots of sensitivity and specificity of miRNA-134 detection in the diagnosis of APE are shown in Fig. 4. The pooled sensitivity and specificity with 95% confidence intervals were 0.86 (0.72–0.94) and 0.75 (0.66–0.82), respectively. Additionally, PLR, NLR, and DOR were 3.4 (2.4–4.8), 0.18 (0.08–0.40), and 19 (7–51), respectively. A summary receiver operating characteristic (SROC) curve is shown in Fig. 5a; the AUC was 0.81 (0.77–0.84). As for heterogeneity, the χ2 and I2 test values were 15.48 (p < 0.1) and 67.70%, respectively, for sensitivity, and 6.59 (p > 0.1) and 24.16%, respectively, for specificity, indicating significant heterogeneity in terms of sensitivity. In diagnostic meta-analysis, the threshold effect is a main source of heterogeneity. The Spearman correlation coefficient between the logarithm of (1-SPE) and the logarithm of SEN was − 0.251 (p = 0.631), demonstrating that there was no threshold effect, and the heterogeneity was mainly derived from the non-threshold effect.
Sensitivity analysis was performed by using the method of removing included articles one by one. The results showed no significant change, indicating that no single study had a significant effect on the overall results (Table 4). A funnel plot was drawn to assess publication bias (Fig. 5b); we found that t = 2.08 and p = 0.11, indicating that no significant publication bias existed in the included studies.
Discussion
In this study, the value of microRNA-134 detection for APE diagnosis was systematically appraised through a meta-analysis. This meta-analysis found that miRNA-134 levels were significantly different between patients with APE and controls. In both plasma and serum samples, APE patients had higher miR-134 levels than controls did, suggesting that miR-134 may be a potential biomarker for APE diagnosis. The pooled sensitivity and specificity were 0.86 (0.72–0.94) and 0.75 (0.66–0.82), respectively, suggesting that the detection of miR-134 has good sensitivity and specificity. The PLR and NLR were 3.4 (2.4–4.8) and 0.18 (0.08–0.40), respectively. The likelihood ratio represents the possibility of developing the target disease. The higher the PLR value, the greater the likelihood of developing the target disease; the opposite is true for the NLR value. The DOR and AUC were 19 (7–51) and 0.81 (0.77–0.84), respectively. The DOR showed that the ratio of the ratio of positive tests in the case group to the ratio of positive tests in the control group was 19. The DOR reflects the degree of connection between the diagnostic test and the disease. The larger the value, the better the discrimination effect of the diagnostic test [24]. However, it cannot differentiate between sensitivity and specificity, and the clinical significance is not obvious [25]. On the contrary, the SROC curve is an overall summary of the characteristics of the test and shows the relationship between sensitivity and specificity, with each dot representing an independent study. Thus, in a diagnostic meta-analysis, the AUC is usually used to estimate the overall diagnostic value. The greater the AUC, the higher the diagnostic accuracy of the index test. The interpretation of AUC values is suggested as follows: low (0.5–0.7), moderate (0.7–0.9), or high (0.9–1) accuracy. In brief, miR-134 tests had good accuracy for APE diagnosis, and miR-134 had the potential to be a diagnostic biomarker for APE.
In clinical practice, APE patients have symptoms similar to those of NSTEMI patients, such as chest discomfort, dyspnea, and nausea, and it is not easy to discriminate the two diseases [26, 27]. If the two diseases cannot be accurately distinguished, the correct treatment cannot be conducted in time. Therefore, accurate identification of APE is very important for the treatment of APE and the reduction of mortality due to APE. One of the articles included in this study, which used NSTEMI patients as controls, showed that miR-134 levels were markedly different between the two groups, and miR-134 levels could significantly distinguish APE patients from the controls, suggesting that circulating miR-134 levels possess good differential diagnosis ability in terms of APE and NSTEMI [12]. This may also provide a new direction and basis in the differential diagnosis of APE and NSTEMI. Because of the few related studies and small sample size of this study, miR-134 as a biomarker to identify myocardial infarction and APE requires more study before it can be applied.
D-dimer, a traditional biomarker, is the degradation product of cross-linked fibrin, and D-dimer tests have the disadvantage of low specificity in APE diagnosis [28]. The sensitivity of D-dimer assays was 83% but the specificity was only 39% [29]. When lower than 500 μg/L, the specificity was about 40–68% in diagnosing APE [30]. The present study found that miR-134 could be a potential biomarker in the diagnosis of APE and that its diagnostic value was good. Several studies showed that compared with D-dimer tests, miR-134 tests had higher specificity, though their sensitivity was lower than D-dimer tests. At the same time, microRNA tests combined with D-dimer tests are more accurate than the single detection of either microRNA or D-dimer for APE diagnosis, with increased sensitivity and specificity [31, 32]. The sensitivity/specificity of miR-27a and D-dimer tests were 79.2%/70.0% and 95.8%/67.5%, respectively. After combining miR-27a tests with D-dimer tests, the sensitivity and specificity increased to 90.5% and 80.0%, respectively. In summary, miR-134 tests combined with D-dimer tests may be an excellent detection method and improve the accuracy of APE diagnosis greatly.
This study has certain limitations, such as its small sample size and heterogeneity. This may be due to differences in the control populations of the included articles, some using healthy people as controls, and some using other non-APE patients as controls. Likewise, there were differences in miR-134 levels among the different populations. In addition, the test samples were different; some studies detected circulating miR-134 content in serum, while others detected miR-134 content in plasma. Subgroup analysis of sample types was conducted but could not explain the source of heterogeneity. Due to the small number of included studies, subgroup analysis of control group and meta-regression were not performed. Kessler et al. found that time can affect miR-134 levels, with miR-134 levels declining as time increases [12]. The time of sample collection was not clear, which may have caused the differences among the studies. Despite its limitations, the present research concluded that circulating miR-134 may be used as a new biomarker for APE diagnosis. In conclusion, this study preliminarily confirmed the reliability of miR-134 detection in APE diagnosis, but more tests and studies are needed to further explore and prove this.
Abbreviations
- APE:
-
Acute pulmonary embolism
- NSTEMI:
-
Non-ST segment elevation myocardial infarction
- SROC:
-
Summary receiver operating characteristic
- AUC:
-
The area under the summary receiver operating characteristic curve
- SEN:
-
Sensitivity
- SPE:
-
Specificity
- PLR:
-
Positive likelihood ratio
- NLR:
-
Negative likelihood ratio
- DOR:
-
Diagnostic odds ratio
References
Konstantinides, S. V., Barco, S., Lankeit, M., & Meyer, G. (2016). Management of pulmonary embolism: an update. Journal of the American College of Cardiology, 67(8), 976–990. https://doi.org/10.1016/j.jacc.2015.11.061.
Giordano, N. J., Jansson, P. S., Young, M. N., Hagan, K. A., & Kabrhel, C. (2017). Epidemiology, pathophysiology, stratification, and natural history of pulmonary embolism. Techniques in Vascular and Interventional Radiology, 20(3), 135–140. https://doi.org/10.1053/j.tvir.2017.07.002.
Douma, R. A., Kamphuisen, P. W., & Buller, H. R. (2010). Acute pulmonary embolism. Part 1. Epidemiology and diagnosis. Nature Reviews. Cardiology, 7(10), 585–596. https://doi.org/10.1038/nrcardio.2010.106.
Doherty, S. (2017). Pulmonary embolism: an update. Australian Family Physician, 46(11), 816–820.
Righini, M., & Robert-Ebadi, H. (2018). Diagnosis of acute pulmonary embolism. Hamostaseologie, 38(1), 11–21. https://doi.org/10.5482/HAMO-17-07-0023.
Lin, Y. T., Tsai, I. C., Tsai, W. L., Lee, T., Chen, M. C., Lin, P. C., et al. (2010). Comprehensive evaluation of CT pulmonary angiography for patients suspected of having pulmonary embolism. The International Journal of Cardiovascular Imaging, 26(Suppl 1), 111–120. https://doi.org/10.1007/s10554-009-9573-8.
Stein, P. D., Woodard, P. K., Weg, J. G., Wakefield, T. W., Tapson, V. F., Sostman, H. D., et al. (2007). Diagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II investigators. Radiology, 242(1), 15–21. https://doi.org/10.1148/radiol.2421060971.
Meyer, G. (2014). Effective diagnosis and treatment of pulmonary embolism: improving patient outcomes. Archives of Cardiovascular Diseases, 107(6–7), 406–414. https://doi.org/10.1016/j.acvd.2014.05.006.
Crawford, F., Andras, A., Welch, K., Sheares, K., Keeling, D., & Chappell, F. M. (2016). D-dimer test for excluding the diagnosis of pulmonary embolism. Cochrane Database of Systematic Reviews, 8, CD010864. https://doi.org/10.1002/14651858.CD010864.pub2.
Konstantinides, S. V., Meyer, G., Becattini, C., Bueno, H., Geersing, G. J., Harjola, V. P., et al. (2019). 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): the Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). The European Respiratory Journal, 54(3). https://doi.org/10.1183/13993003.01647-2019.
Bartel, D. P. (2004). MicroRNAs: genomics, biogenesis, mechanism, and function. Cell, 116(2), 281–297. https://doi.org/10.1016/s0092-8674(04)00045-5.
Kessler, T., Erdmann, J., Vilne, B., Bruse, P., Kurowski, V., Diemert, P., et al. (2016). Serum microRNA-1233 is a specific biomarker for diagnosing acute pulmonary embolism. Journal of Translational Medicine, 14(1), 120. https://doi.org/10.1186/s12967-016-0886-9.
Deng, H. Y., Li, G., Luo, J., Wang, Z. Q., Yang, X. Y., Lin, Y. D., et al. (2016). MicroRNAs are novel non-invasive diagnostic biomarkers for pulmonary embolism: a meta-analysis. Journal of Thoracic Disease, 8(12), 3580–3587. https://doi.org/10.21037/jtd.2016.12.98.
Xiang, Q., Zhang, H. X., Wang, Z., Liu, Z. Y., Xie, Q. F., Hu, K., et al. (2019). The predictive value of circulating microRNAs for venous thromboembolism diagnosis: a systematic review and diagnostic meta-analysis. Thrombosis Research, 181, 127–134. https://doi.org/10.1016/j.thromres.2019.07.024.
Xiao, J., Jing, Z. C., Ellinor, P. T., Liang, D., Zhang, H., Liu, Y., et al. (2011). MicroRNA-134 as a potential plasma biomarker for the diagnosis of acute pulmonary embolism. Journal of Translational Medicine, 9, 159. https://doi.org/10.1186/1479-5876-9-159.
Wang, Y., Zhao, Z., Zhang, Y., Jiang, X., & Duo, J. (2017). Plasma miRNA-134 is a diagnostic biomarker for acute pulmonary embolism in middle and high altitude areas. Biomedical Research-India, 28(12), 5494–5498.
Haizhen, M. (2018). The expressions of plasma microRNA-134 for the acute pulmonary embolism at high altitude area. Master: Qinghai University.
Heng, Z. (2016). The diagnostic value of microRNA-134 for the acute pulmonary embolism at middle altitude. Master: Qinghai University.
Bang, Z., Ruchang, C., & Xiaodan, Z. (2018). Detection of serum miRNAs markers and clinical value of miR-134 in patients with acute pulmonary embolism. Clinical Education of General Practice, 16(6), 617–620.
McInnes, M. D. F., Moher, D., Thombs, B. D., McGrath, T. A., Bossuyt, P. M., & the, P.-D. T. A. G., et al. (2018). Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: the PRISMA-DTA statement. JAMA, 319(4), 388–396. https://doi.org/10.1001/jama.2017.19163.
Whiting, P. F., Rutjes, A. W., Westwood, M. E., Mallett, S., Deeks, J. J., Reitsma, J. B., et al. (2011). QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine, 155(8), 529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009.
Deville, W. L., Buntinx, F., Bouter, L. M., Montori, V. M., de Vet, H. C., van der Windt, D. A., et al. (2002). Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Medical Research Methodology, 2, 9. https://doi.org/10.1186/1471-2288-2-9.
Zhou, X., Wen, W., Shan, X., Qian, J., Li, H., Jiang, T., et al. (2016). MiR-28-3p as a potential plasma marker in diagnosis of pulmonary embolism. Thrombosis Research, 138, 91–95. https://doi.org/10.1016/j.thromres.2015.12.006.
Glas, A. S., Lijmer, J. G., Prins, M. H., Bonsel, G. J., & Bossuyt, P. M. (2003). The diagnostic odds ratio: a single indicator of test performance. Journal of Clinical Epidemiology, 56(11), 1129–1135. https://doi.org/10.1016/s0895-4356(03)00177-x.
Lee, J., Kim, K. W., Choi, S. H., Huh, J., & Park, S. H. (2015). Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical. Researchers-Part II. Statistical. methods of meta-analysis. Korean Journal of Radiology, 16(6), 1188–1196. https://doi.org/10.3348/kjr.2015.16.6.1188.
Kim, J. Y., Kim, K. H., Cho, J. Y., Sim, D. S., Yoon, H. J., Yoon, N. S., et al. (2019). D-dimer/troponin ratio in the differential diagnosis of acute pulmonary embolism from non-ST elevation myocardial infarction. The Korean Journal of Internal Medicine, 34(6), 1263–1271. https://doi.org/10.3904/kjim.2018.153.
Anderson, J. L., & Morrow, D. A. (2017). Acute myocardial infarction. The New England Journal of Medicine, 376(21), 2053–2064. https://doi.org/10.1056/NEJMra1606915.
Weitz, J. I., Fredenburgh, J. C., & Eikelboom, J. W. (2017). A test in context: D-dimer. Journal of the American College of Cardiology, 70(19), 2411–2420. https://doi.org/10.1016/j.jacc.2017.09.024.
Froehling, D. A., Elkin, P. L., Swensen, S. J., Heit, J. A., Pankratz, V. S., & Ryu, J. H. (2004). Sensitivity and specificity of the semiquantitative latex agglutination D-dimer assay for the diagnosis of acute pulmonary embolism as defined by computed tomographic angiography. Mayo Clinic Proceedings, 79(2), 164–168. https://doi.org/10.4065/79.2.164.
Jain, S., Khera, R., Suneja, M., Gehlbach, B., & Kuperman, E. (2015). Role of D-dimer assays in the diagnostic evaluation of pulmonary embolism. The American Journal of the Medical Sciences, 350(6), 501–507. https://doi.org/10.1097/MAJ.0000000000000405.
Wang, Q., Ma, J., Jiang, Z., Wu, F., Ping, J., & Ming, L. (2018). Diagnostic value of circulating microRNA-27a/b in patients with acute pulmonary embolism. International Angiology, 37(1), 19–25. https://doi.org/10.23736/S0392-9590.17.03877-9.
Qian, W. (2018). Diagnostic value and mechanism of plasma microRNA-27a/ b in patients with acute pulmonary embolism. Zhengzhou University.
Acknowledgments
Thanks to Associate Professor Yu Xiaojin, Department of Epidemiology and Health Statistics, School of Public Health, Southeast University, for her help and guidance in data processing and analysis.
Funding
This study was funded by Key Research and Development Project of Hebei Province: Study on circulating biomarkers of acute pulmonary thromboembolism and its application value in risk stratification and prognosis evaluation (grant number 182777198).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Associate Editor Craig M. Stolen oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Y., Xie, M., Gao, X. et al. Predictive Value of Circulating microRNA-134 Levels for Early Diagnosis of Acute Pulmonary Embolism: Meta-analysis. J. of Cardiovasc. Trans. Res. 14, 744–753 (2021). https://doi.org/10.1007/s12265-020-10087-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-10087-4