Abstract
Ethanol is widely known for its ability to cause dramatic changes in emotion, social cognition, and behavior following systemic administration in humans. Human neuroimaging studies suggest that alcohol dependence and chronic pain may share common mechanisms through amygdala-medial prefrontal cortex (mPFC) interactions. However, whether acute administration of ethanol in the mPFC can modulate pain perception is unknown. Here we showed that bilateral microinjections of ethanol into the prelimbic and infralimbic areas of the mPFC lowered the bilateral mechanical pain threshold for 48 h without influencing thermal pain sensitivity in adult rats. However, bilateral microinjections of artificial cerebrospinal fluid into the mPFC or bilateral microinjections of ethanol into the dorsolateral PFC (also termed as motor cortex area 1 in Paxinos and Watson’s atlas of The Rat Brain. Elsevier Academic Press, Amsterdam, 2005) failed to do so, suggesting regional selectivity of the effects of ethanol. Moreover, bilateral microinjections of ethanol did not change the expression of either pro-apoptotic (caspase-3 and Bax) or anti-apoptotic (Bcl-2) proteins, suggesting that the dose was safe and validating the method used in the current study. To determine whether γ-aminobutyric acid A (GABAA) receptors are involved in mediating the ethanol effects, muscimol, a selective GABAA receptor agonist, or bicuculline, a selective GABAA receptor antagonist, was administered alone or co-administered with ethanol through the same route into the bilateral mPFC. The results showed that muscimol mimicked the effects of ethanol while bicuculline completely reversed the effects of ethanol and muscimol. In conclusion, ethanol increases mechanical pain sensitivity through activation of GABAA receptors in the mPFC of rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ethanol has long been known to influence the processes of emotion, social cognition, and somatic sensation through social drinking and experimental administration [1–3]. Acute alcohol consumption and intranasal oxytocin administration have been proposed to have a common effect on emotion, social cognition, and behavior through acting on limbic and prefrontal cortical structures in humans, resulting in an enhancement of empathy-based altruism such as helping motivation, trust, generosity, and morality [3]. Some human neuroimaging studies have suggested that alcohol-dependence and chronic pain may also share mechanisms through amygdala—medial prefrontal cortex (mPFC) interactions [2]. The mPFC, a cortical structure that includes the prelimbic (PrLC), infralimbic (ILC), and anterior cingulate cortex (ACC) [4–6], has been demonstrated to be involved in pain processing [7–14]. More recently, we also demonstrated that the mPFC is involved in the mediation of empathy for pain in rats, a phenomenon in which the mechanical pain sensitivity and spinal nociceptive responses of rats are dramatically increased after social interaction with a cagemate (but not a non-cagemate) in pain [15]. These results imply that the mPFC is one of the key brain structures involved in the cognitive and emotional modulation of pain [11, 15, 16]. As for the action of ethanol in the central nervous system, some in vitro brain slice studies have shown that ethanol facilitates the release of neurotransmitters such as γ-aminobutyric acid (GABA), dopamine, serotonin, and opioids, whereas it inhibits glutamate activity, resulting in alterations in behavior [1]. Ethanol has been shown to be anxiolytic and sedative-hypnotic, as well as impairing cognition and motor coordination, through the enhancement of GABA release [17]. The effects of ethanol on pain perception, however, are controversial. On one hand, ethanol has been shown to have an analgesic effect by systemic (intraperitoneal, i.p.) administration [18–21], but on the other hand, a hyperalgesic effect can also be induced by systemic or intracerebroventricular administration [22]. Human and animal studies have respectively demonstrated that cerebral blood flow [23–25] and c-Fos immunoreactivity [26, 27] in the PFC are significantly increased after acute alcohol administration. Moreover, the systemic effects of ethanol on behavior can be significantly reversed by disrupting the function of the mPFC [28–31]. However, the effects of the direct action of ethanol in the mPFC remain unclear. Here, we set out to address this question.
Materials and Methods
Animals
Adult male Sprague-Dawley rats weighing 260–320 g were obtained from the Laboratory Animal Center of the Fourth Military Medical University (FMMU), Xi’an, China. The animals were kept in a temperature-controlled room (22–26 °C) under a 12-h light/dark cycle with free access to food and water. Before behavioral tests, the rats were individually habituated to the test boxes for >30 min each day for 5 consecutive days. All behavioral assessments were performed during the light phase of the cycle. The experimental procedures were approved by the Animal Care and Use Committee of the FMMU, and followed the National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH Publication No. 80-23, revised 1996). The animals were treated in accordance with the ethical guidelines established by the International Association for the Study of Pain [32]. The number of animals used and their suffering were minimized.
Surgery
The surgery was carried out as previously described [33–35]. Rats were anesthetized with sodium pentobarbital (50 mg/kg, i.p.), and then placed in a stereotaxic instrument (Narishige Scientific Instrument Lab, Tokyo, Japan). After a midline incision, 2 holes were drilled over the bilateral target regions to allow cannula implantation. According to the Paxinos and Watson’s atlas of The Rat Brain in Stereotaxic Coordinates [36], custom-designed stainless-steel guide cannulas (diameter 0.48 mm; RWD Life Science Co., Ltd., Shenzhen, China) were implanted to target the PrLC (bregma rostrocaudal 3.2 mm, mediolateral 0.7 mm, dorsoventral 3.5 mm), ILC (bregma rostrocaudal 3.2 mm, mediolateral 0.7 mm, dorsoventral 5.0 mm) or dorsolateral PFC (equivalent to the motor cortex area 1, MCx) (bregma rostrocaudal 2.5 mm, mediolateral 2.8 mm, dorsoventral 2.0 mm), which was used as an offsite control [35]. The cannulae were fixed to the skull with dental cement. Stylets were inserted into the cannulae between experiments. Penicillin and streptomycin (each at 300 mg/kg, i.p.) were administered immediately after surgery to prevent infection. After surgery, rats were handled for ~4 min each day to minimize the stress reaction during drug administration and were allowed 7 days for recovery.
Drugs and Microinjections
Ethanol (Sinopharm Chemical Reagent Co., Ltd., Shanghai, China), the competitive GABAA receptor antagonist bicuculline methochloride (Tocris, Ellisville, MO), and the selective GABAA receptor agonist muscimol hydrobromide (Sigma, St. Louis, MO) were all dissolved in sterile artificial cerebrospinal fluid (ACSF) containing (in mmol/L): 125.0 NaCl, 2.6 KCl, 2.5 NaH2PO4, 1.3 CaCl2, 0.9 MgCl2, 21.0 NaHCO3, and 3.5 glucose. All working solutions were freshly prepared before each experiment and protected from light during the experimental sessions. ACSF served as the vehicle control in all experiments. Rats received bilateral microinjections of ethanol (20 mmol/L, ~90 mg/dL, equivalent to a peak blood concentration of 1.0 g/kg, defined as moderate consumption), bicuculline (20 μmol/L), or muscimol (5 mmol/L) in a volume of 0.5 μL over 60 s using a Hamilton syringe attached to polyethylene tubing as in previous studies [1, 14, 37, 38]. The microinjections started 5 min after injector insertion, and the injectors remained in place for full drug diffusion. Bicuculline was co-administered with ethanol or muscimol into the mPFC 1 h in advance to determine whether a GABAergic mechanism is involved in the effects of ethanol on basal pain sensitivity. The dose of ethanol (20 mmol/L) used in the current study is safe and effective according to previous reports [1, 37]. In many previous studies, blood concentrations ranging from 20 to 90 mg/dL (5–20 mmol/L) have been defined as indicating low to moderate ethanol consumption [1]. Ethanol at 25–100 mmol/L has also been demonstrated to washout-reversibly suppress the persistent activity of PFC neurons in brain slice patch-clamp recordings [37]. Systemic administration of 0.375–3.5 g/kg of ethanol to rats has been shown to result in blood concentrations ranging from ~50 to 350 mg/dL (10–70 mmol/L) which also dose-dependently reduces spike activity in PFC neurons 30 min after treatment [37]. In that study, a dose of 20 mmol/L ethanol (90 mg/dL; equivalent to 1.0 g/kg) was effective and believed to be moderate in amount [37]. In a pilot study, we also demonstrated that intra-PFC microinjection of 20 mmol/L ethanol induced bicuculline-reversible mechanical pain hypersensitivity. Thus, it was safe and reasonable to select 20 mmol/L as a single dose for intracerebral microinjection. To determine whether this dose of ethanol causes loss of neurons, the expression levels of pro-apoptotic (caspase-3 and Bax) and anti-apoptotic (Bcl-2) proteins were measured 1, 2, and 48 h after bilateral microinjection of ethanol or ACSF. The number of neuronal profiles labeled with Ca2+/calmodulin-dependent protein kinase II (CaMKII), a biomarker of excitatory neuronal activity, and the total number of neurons labeled with NeuN were also counted after immunocytochemical staining.
Experimental Design
Animals were randomly divided into 11 groups (Table 1). Basal paw withdrawal mechanical threshold (PWMT, g) and paw withdrawal thermal latency (PWTL, s) were measured one day before drug administration.
Mechanical Pain Sensitivity
Mechanical pain sensitivity was measured using von Frey monofilaments as described previously [39, 40]. Rats were individually adapted in a plastic chamber placed on a metal mesh floor for 30 min before testing. The monofilaments were applied with ascending bending forces of 0.8, 2.0, 5.0, 7.0, 10.0, 13.0, 16.0, 20.0, 25.0, 30.0, 45.0, and 60 g. Each monofilament was applied to the target hind-paw 10 times (once every several seconds) in order to evoke the paw-withdrawal reflex. The bending force that caused a 50% occurrence of the reflex was expressed as the PWMT.
Thermal Pain Sensitivity
Thermal pain sensitivity was measured as the withdrawal latency of the hind-paws in response to radiant heat stimuli [39, 40]. Rats were individually acclimated to a plastic chamber on the surface of a 2-mm thick glass plate for 30 min before testing. Five heat stimuli applied with a TC-1 radiant heat stimulator (new generation RTY-3; Xi’an Bobang Technologies of Chemical Industry Co. Ltd., Xi’an, China) to the plantar area of each hind-paw were repeated at 10-min intervals. The latency was calculated as the time from the beginning of a heat stimulus to the appearance of a marked paw-withdrawal reflex. Each hind-paw of each rat was tested 5 times, and the last 4 values were averaged to give the mean PWTL. The abandon of the first value was due to larger bias in PWTL than the latter ones in each animal. A maximal cutoff of 40 s was used to avoid tissue injury.
Quantification of Persistent Spontaneous Nociceptive Behavior
Estimation of persistent spontaneous nociception was based on our previous report [39]. Before intra-plantar administration of bee venom (BV), the rat received intra-mPFC microinjection of ACSF, ethanol, or muscimol and was acclimated in a transparent box which was placed on a supporting frame 30 cm above the table for 30 min. Then BV was injected into the center of the plantar surface of left hind-paw. BV-induced pain-related behavior was expressed as the number of paw flinches quantified at 5-min intervals for 1 h following injection.
Western Blot
Bilateral mPFC tissues were obtained at 1, 2, and 48 h after intra-mPFC microinjection of ethanol (20 mmol/L) and then homogenized in RIPA lysis buffer containing protease inhibitors (Applygen Technologies Inc., Beijing, China). The protein concentration in the lysate was determined using a BCA Protein Assay kit (Thermo Scientific, Rockford, IL). Protein samples were heated at 98 °C for 10 min, and 50 μg of protein was separated on 12% SDS-PAGE gel (Bio-Rad, Berkeley, CA) and then transferred onto PVDF membranes (Immobilon P, Millipore, Billerica, MA). The membranes were blocked with 5% skim milk for 3 h at room temperature and incubated with rabbit polyclonal antibody against Bcl-2, caspase-3, or Bax (1:200 for all three antibodies, Santa Cruz, Dallas, TX) at 4 °C overnight. Then the membranes were incubated with an HRP-conjugated secondary antibody (1:2000, Bio-Rad) at room temperature for 2 h. After that, the membranes were treated with enhanced chemiluminescence reagents and images captured with FluorChem FC2 (Alpha Innotech Corp., San Leandro, CA). The density of the bands was measured with AlphaImager software and normalized to β-tubulin. All western blot analyses were performed at least three times from 5 rats.
Double Immunofluorescent Labeling
Forty-eight hours after intra-mPFC microinjection of ethanol or ACSF, rats were deeply anesthetized with sodium pentobarbital (50 mg/kg, i.p.) and perfused intracardially with saline followed by 4% paraformaldehyde in phosphate-buffered saline (PBS). After perfusion, the brain was removed and post-fixed overnight, then cryoprotected in 30% phosphate-buffered sucrose. Transverse frozen sections (40 μm) were cut on a CM1900 freezing microtome (Leica, Wetzlar, Germany) and then blocked with 1% bovine serum in PBS for 1 h at room temperature. For double immunofluorescent labeling, sections were incubated with a mixture of primary antibodies [mouse anti-CaMKII 1:200 (ab22609, Abcam, Cambridge, MA) and rabbit anti-NeuN 1:200 (ab177487, Abcam)] at 4 °C overnight, followed by a mixture of secondary antibodies [FITC-conjugated goat anti-mouse IgG, 1:200 (Sigma) and Cy3-conjugated sheep anti-rabbit IgG, 1:200 (Sigma)] for 3 h. Photomicrographs were captured under a laser scanning confocal fluorescence microscope (FV 1000, Olympus, Tokyo, Japan) and processed with Image-Pro Plus digitizing software (Olympus). The numbers of CaMKII-positive and NeuN-positive neurons were counted using ImageJ software (NIH, Bethesda, MD).
Histological Localization of Injection Sites
These procedures were as in our previous report [9]. In brief, after the behavioral tests, rats were fully anesthetized with sodium pentobarbital (50 mg/kg, i.p.) and perfused transcardially with sterile saline followed by 4% paraformaldehyde. The brains were removed, postfixed in 4% paraformaldehyde for 3 h and then stored in 30% sucrose until they sank to the bottom of the container. Frozen sections (40 μm) were cut on a freezing microtome (CM1900, Leica, Wetzlar, Germany) and Nissl stained with 0.1% cresyl violet. Photomicrographs were captured on a computer-based microscope CCD camera (DP-70, Olympus) and processed using Image-Pro-Plus 6.1 software (Media Cybernetics, Warrendale, PA).
Statistical Analysis
All data were analyzed using SPSS 19.0 and are presented as the mean ± SEM. Non-parametric analysis (Mann-Whitney U test and Kruskal-Wallis H test [Nemenyi test]) and two-way repeated measures ANOVA were used. P < 0.05 was considered to be statistically significant.
Results
Based on the histological localization of the injection sites, 103 pairs of microinjections were effectively confined to the PrLC and 24 pairs to the ILC on both sides (Fig. 1), while 13 pairs were confined to the bilateral MCx [36] (Fig. 4A, B).
Localization of injection sites. A, C Left panels: images of rat brains showing the sites of cannula implantation through the surface of the medial prefrontal cortices (arrows). Right panels: photomicrographs showing the tracks and sites of cannulation within the bilateral prelimbic cortex (PrLC, arrows) or infralimbic cortex (ILC, arrows) of the medial forebrain (stained with 0.1% cresyl violet). B, D Schematic diagrams showing the injection sites confined to the bilateral PrLC (B, filled circles, n = 103) and ILC (D, filled circles, n = 24) along the rostrocaudal axis. Bre, bregma; fmi, forceps minor of the corpus callosum; ILC, infralimbic cortex; MCx, motor cortex; PrLC, prelimbic cortex.
Bilateral Intra-mPFC Microinjections of Ethanol Decrease Mechanical Pain Threshold and Increase Pain Response
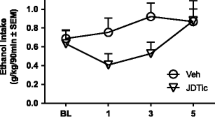
Bilateral microinjections of ethanol (20 mmol/L in 0.5 μL) into the PrLC or the ILC resulted in significant reductions in the PWMT of both hind-paws in naïve rats relative to ACSF controls (Fig. 2A, C). The time-course showed that the ethanol-induced mechanical pain hypersensitivity reached a peak during 1–2 h after injection, followed by half recovery at 24 h and complete recovery at 48 h (Fig. 2A, C). However, rats receiving the same intra-PrLC and intra-ILC ethanol microinjections did not show any statistically significant difference in thermal pain sensitivity relative to the ACSF controls and baseline (Fig. 2B, D). To explore whether the same ethanol treatment can enhance pain responses, bilateral microinjections of ACSF or ethanol were administered to rats receiving BV injections (n = 6 for each group). We found that the number of paw flinches was significantly increased by intra-mPFC ethanol microinjections relative to the ACSF group (Fig. 3).
Effects of intra-PrLC and intra-ILC cortical microinjections of ethanol (20 mmol/L in 0.5 μL) on mechanical and thermal pain sensitivity. A Time courses of PWMT after ethanol or ACSF administration in the PrLC [n = 6; ***P < 0.001, ethanol vs ACSF for both hind-paws at 1 h (F = 46.032, df = 1 for the left paw; F = 41.504, df = 1 for the right paw), 2 h (F = 49.843, df = 1 for the left paw; F = 25.410, df = 1 for the right paw), and 24 h (F = 25.971, df = 1 for the left paw; F = 27.458, df = 1 for the right paw)]. C Time courses of the PWMT after ethanol or ACSF administration in the ILC [n = 6; **P < 0.01, ***P < 0.001, ethanol vs ACSF for the left hind-paw at 1 h (F = 21.022, df = 1) and 2 h (F = 29.739, df = 1); ## P < 0.01, ethanol vs ACSF for the right hind-paw at 1 h (F = 16.858, df = 1), 2 h (F = 16.723, df = 1), and 24 h (F = 17.622, df = 1)]. B, D Time courses of the PWTL after ethanol or ACSF administration in the PrLC (B, n = 7) and the ILC (D, n = 6). Two-way repeated measures ANOVA; mean ± SEM.
To determine whether the intra-mPFC ethanol effect is region-selective, we chose the MCx as an offsite control. We found that bilateral intra-MCx microinjections of ethanol or ACSF had no significant effect on mechanical (Fig. 4C) or thermal (Fig. 4D) pain sensitivity.
Localization of intra-MCx cannulation and the effects of intra-MCx microinjection of ethanol (20 mmol/L in 0.5 µL) on mechanical and thermal pain sensitivity. A Left panel: image of a rat brain with arrows indicating the sites of cannula implantation through the surface of the dorsolateral prefrontal cortices (shown as the motor cortex area 1 in the Paxinos and Watson’s atlas, MCx). Right panel: photomicrograph showing the histological localization of tracks and sites of the cannulation within the bilateral MCx (arrows). B Schematic diagrams showing the injection sites (filled circles, n = 13) confined to the bilateral MCx areas along the rostrocaudal axis [diagrams are taken from the rat brain atlas of Paxinos and Watson (2005)]. C, D PWMT and PWTL values 1 h after microinjections (Mann-Whitney U test; n.s., not significant; mean ± SEM). Bre, bregma; CPu, caudate-putamen; MCx, motor cortex.
Further, Western blot showed no changes in the level of pro-apoptotic (caspase-3 and Bax) or anti-apoptotic (Bcl-2) proteins in the mPFC 1, 2, and 48 h after bilateral intra-mPFC microinjections of ethanol relative to ACSF (Fig. 5). Immunocytochemical staining also showed no significant decreases in the number of neuronal profiles labeled with CaMKII (a biomarker of active excitatory neurons [41]) and neuronal nuclear profiles labeled with NeuN (a neuronal nuclear biomarker) in the mPFC (Fig. 6).
Double immunofluorescent labeling of CaMKII and NeuN in rats with intra-mPFC microinjections of ethanol and ACSF. A Microphotographs showing the sites of the implanted cannula and localization of the injection site (*) from one side for ACSF and ethanol. Images in the lower panel are magnifications of the insets in the upper panel. B Ratio of CaMKII-positive to NeuN-positive neuronal profiles (n = 5/group). C Total number of NeuN-positive neuronal profiles (n = 5/group); Mann-Whitney U test for B and C; mean ± SEM. mi, forceps minor of the corpus callosum; n.s., not significant.
Ethanol-Induced Mechanical Pain Hypersensitivity is Mediated by Activation of GABAA Receptors in the mPFC
To further explore the mechanisms underlying the effects of intra-mPFC ethanol, we targeted GABAA receptors by bilateral intra-mPFC microinjections of its agonist muscimol and antagonist bicuculline. We found that the bilateral intra-mPFC administration of muscimol (5 mmol/L in 0.5 μL) mimicked the same treatment with ethanol in terms of both the magnitude and time-course of mechanical pain hypersensitivity (Fig. 7A). But no statistically significant difference in thermal pain sensitivity was found between intra-mPFC muscimol and ACSF at 1, 4, and 8 h after administration (Fig. 7B). Intra-mPFC muscimol also significantly enhanced the BV-induced pain responses relative to the ACSF control (Fig. 3). Moreover, bilateral intra-mPFC co-administration of ethanol or muscimol with bicuculline (20 μmol/L in 0.5μL) completely reversed the hyperalgesic effects of ethanol or muscimol alone (Fig. 8). Finally, bilateral intra-mPFC microinjections of bicuculline alone had no significant effect on basal pain sensitivity to either mechanical or thermal stimuli (Fig. 9).
Effects of intra-mPFC microinjection of muscimol (5 mmol/L in 0.5 μL) on mechanical and thermal pain sensitivity. A Time-courses of the PWMT after muscimol (n = 8) and ACSF (n = 6) administration. B PWTL values after muscimol and ACSF administration (n = 7/group). Two-way repeated measures ANOVA for A and B. ***P < 0.001, muscimol vs ACSF for both hind-paws at 1 h (F = 155.309, df = 1 for the left paw; F = 150.682, df = 1 for the right paw), 2 h (F = 118.629, df = 1 for the left paw; F = 173.014, df = 1 for the right paw), and 4 h (F = 79.761, df = 1 for the left paw; F = 77.233, df = 1 for the right paw). Mean ± SEM; n.s., not significant.
Reversal effects of bicuculline (Bic, 20 μmol/L in 0.5 μL) on the intra-mPFC ethanol- and muscimol-induced mechanical pain hypersensitivity. The numbers of animals used in the groups of ACSF, ethanol, muscimol, ethanol + Bic, and muscimol + Bic were 12, 14, 14, 10, and 7, respectively (***P < 0.001, ethanol or muscimol vs ACSF for both hind-paws; # P < 0.05, ethanol + Bic vs ethanol in the right hind-paw; ## P < 0.01, ethanol + Bic vs ethanol in the left hind-paw and muscimol + Bic vs muscimol in both hind-paws; Kruskal-Wallis H test). Mean ± SEM.
Discussion
In the present study, we demonstrated that ethanol facilitated spinal nociceptive responses through the direct activation of GABAA receptors in both the PrLC and ILC of the rat mPFC, resulting in mechanical pain hypersensitivity. With regard to the ethanol modulation of pain acting within the mPFC, there are two major concerns: the regional specificity, and neurotoxicity that may damage excitatory neurons. According to the current results, the intra-mPFC effect of ethanol is most likely to be region-specific because intra-MCx microinjection of the same dose of ethanol did not have any significant effects on mechanical or thermal pain sensitivity (Fig. 4). Although a recent report showed that inactivation of the PrLC, but not the ILC, impairs the acquisition and expression of formalin-induced conditioned place avoidance [42], our results indicate that the PrLC and the ILC play the same roles in the mediation of ethanol-induced mechanical pain hypersensitivity. The reason for this difference is not known, but we investigated the effects of ethanol on mechanical and thermal pain sensitivity, while they examined the roles of these brain structures in the mediation of formalin-induced place avoidance, which reflects different components of pain. Neurotoxic effects of the dose used in the current study can also be largely excluded because apoptotic processes are not likely to be involved given the results that neither pro-apoptotic nor anti-apoptotic proteins were changed 2 days after intra-mPFC ethanol microinjection (Fig. 5). Immunocytochemical staining of CaMKII, a biomarker of excitatory neurons, did not show any new loss of neurons around the tracks of cannulae either, largely excluding neurotoxic effects of ethanol on excitatory neurons that may cause an imbalance between excitatory and inhibitory pools (Fig. 6). The reversal effects of bicuculline on the intra-mPFC ethanol effects also provided strong evidence supporting the existence of neuronal activity involving the actions of ethanol and muscimol on GABAA receptors (Figs. 7, 8). However, blockade of GABAA receptors within the mPFC in rats without any other treatment did not change the basal pain sensitivity of either the mechanical or the thermal modality (Fig. 9). Taken together, the facilitation of mechanical pain sensitivity by intra-mPFC ethanol is region-specific and mediated by GABAA receptors. As social interaction with a cagemate in pain can also selectively increase mechanical pain sensitivity in the observer rat via the mPFC, a phenomenon referred to as empathy for pain [15], it is reasonable to propose that the facilitation of mechanical pain sensitivity by intra-mPFC ethanol may share the same top-down pathways as the empathy-associated facilitation of spinal nociception.
Where and How Ethanol Modulates Pain?
In the literature, the effects of ethanol on pain perception have been controversial due to contradictory results. Several studies have shown that acute alcohol administration (i.p.) results in a modest lowering of the sensitivity to noxious stimuli as evaluated by tail-deflection [18], electric shocks [19], and tail-flick [20, 21]. The antinociception induced by acute doses of ethanol is fully suppressed by intrathecal administration of flumazenil, a GABAA receptor antagonist [20], and increased by benzodiazepines (diazepam and midazolam) [43, 44], implicating the participation of the spinal dorsal horn in the ethanol-induced analgesia.
However, it has also been reported that systemic administration of non-hypnotic doses of ethanol and barbiturates to rats results in reduction of tail-flick latency and this is abolished by non-convulsant doses of the GABAA receptor channel blocker picrotoxin, indicating involvement of GABAergic mechanisms in the mediation of ethanol-induced hyperalgesia [22]. Other studies have demonstrated that intracerebroventricular, but not intrathecal administration of these drugs induces a similar hyperalgesic state that is also reversed by a GABAA receptor blocker [45, 46]. These results suggested that ethanol and some barbiturates might induce pain hypersensitivity (hyperalgesia) through acting on GABAA receptors at the supraspinal level, while they induce antinociception (analgesia) through acting on GABAA receptors at the spinal level. Here, we provided direct evidence for an action of ethanol on GABAA receptors in the mPFC, inducing mechanical pain hypersensitivity in naïve rats. The reason why thermal pain sensitivity was not altered by intra-mPFC ethanol is unknown and remains to be further studied.
Involvement of mPFC in Top-Down Facilitation of Mechanical Pain Sensitivity
One of the major findings in the current study was that activation of GABAA receptors in the mPFC by ethanol facilitated mechanical pain sensitivity. One possible explanation of this local effect of ethanol is activation of the descending nociceptive facilitation pathway [47]. It is interesting to note that neuronal activity in the mPFC, especially the PrLC and ILC, can be inhibited by a GABAergic enhancing mechanism under some pathological pain conditions in animal models of joint arthritis, peripheral neuropathy, and visceral pain [14, 48–50]. Moreover, deactivation of excitatory neurons in the PrLC via Cdk5 (cyclin-dependent kinase 5) promotes pain sensation and anxiety [13]. In contrast, optogenetic activation of excitatory pyramidal neurons in the PrLC reverses the GABA-mediated inhibitory state, improving both the sensory and affective aspects of pain [13, 14, 50, 51]. Besides, pharmacological activation of the ILC output with a combination of metabotropic glutamate receptor 5 (mGluR5) and cannabinoid receptor type 1 (CB1) activators inhibits pain-related behavior and restores decision-making in an arthritis model of pain [52]. These results clearly demonstrate that the PrLC and ILC play a major role in the processing of pain information by balancing excitatory and inhibitory synaptic transmission, which in turn monitors spinal nociception via top-down pathways.
Although the PrLC and the ACC are subregions of the mPFC, they may use different neuronal circuits in processing pain information. For example, in a more recent report, it was found that the activation of ACC excitatory pyramidal neurons results in pain hypersensitivity (hyperalgesia), however, inhibition of these neurons or activation of parvalbumin-expressing inhibitory interneurons in the ACC reverses the pain hypersensitivity induced by Freund’s complete adjuvant [53]. However, in another report [48], the neuronal activity recorded in the PrLC in response to bicuculline administered into the PrLC and the ACC was quite different in each case, i.e., bicuculline induced disinhibition when acting within the PrLC, but resulted in inhibition when acting within the ACC, strongly supporting our current finding that GABAA receptor activation in the PrLC is involved in ethanol-induced mechanical pain hypersensitivity by enhancing GABAergic transmission.
Does mPFC Mediate Ethanol-Induced Emotional Empathy?
Empathy, a basic prosocial behavior, reflects the natural ability to feel, understand, and share the emotional states of others and is generally divided into emotional (affective) empathy and cognitive empathy [54–58]. Experimental human and animal studies have demonstrated that observing intimates in pain (cagemates for animals) heightens an individual’s pain perception, referred to as empathy for pain [15, 54, 59–63]. Human neuroimaging and functional anatomical studies have revealed that the mPFC (Brodmann’s areas 10 and 11) may be associated with cognitive empathy, while the dorsolateral PFC (Brodmann’s area 44) may be associated with emotional empathy [55]. In rats, bilateral lesions of the mPFC have been demonstrated to eliminate both behaviors associated with empathy for pain and behaviors associated with social attachment and sharing [15]. Moreover, our unpublished data also show that bilateral intra-mPFC microinjection of an oxytocin receptor antagonist and bicuculline blocks behavior associated with empathy for pain in rats. Taken together with our current results, we propose that the mPFC, especially the PrLC and ILC subregions, is involved in the mediation of both ethanol-induced emotional empathy and empathy for pain through social interaction.
Ethanol, recreationally consumed in social settings, is widely known for its ability to increase emotional (affective) empathy, facilitating social attachment and alleviating anxiety at moderate doses [64–70]. However, so far, the exact brain regions involved in ethanol-induced empathy are not known. In the current study, we provide direct evidence that the mPFC is the brain region where ethanol acts to induce pain empathy-like behavioral changes through activating GABAA receptors. The similarity of GABAA receptor activation between ethanol and oxytocin in the mPFC suggests that they share a common structure and neuronal circuits to induce emotional empathy for pain and other prosocial and altruistic behaviors that require further investigation. This proposition is partially supported by a recent study showing involvement of the mPFC and striatum in social play behaviors in rats [71].
In conclusion, ethanol can facilitate mechanical nociception and pain responses through activation of GABAA receptors in the mPFC of rats.
References
Eckardt MJ, File SE, Gessa GL, Grant KA, Guerri C, Hoffman PL, et al. Effects of moderate alcohol consumption on the central nervous system. Alcohol Clin Exp Res 1998, 22: 998–1040.
Apkarian AV, Neugebauer V, Koob G, Edwards S, Levine JD, Ferrari L, et al. Neural mechanisms of pain and alcohol dependence. Pharmacol Biochem Behav 2013, 112: 34–41.
Mitchell IJ, Gillespie SM, Abu-Akel A. Similar effects of intranasal oxytocin administration and acute alcohol consumption on socio-cognitions, emotions and behaviour: Implications for the mechanisms of action. Neurosci Biobehav Rev 2015, 55: 98–106.
Riga D, Matos MR, Glas A, Smit AB, Spijker S, Van den Oever MC. Optogenetic dissection of medial prefrontal cortex circuitry. Front Syst Neurosci 2014, 8: 230.
Giustino TF, Maren S. The role of the medial prefrontal cortex in the conditioning and extinction of fear. Front Behav Neurosci 2015, 9: 298.
Jin J, Maren S. Prefrontal-hippocampal interactions in memory and emotion. Front Syst Neurosci 2015, 9: 170.
Zhuo M. A synaptic model for pain: long-term potentiation in the anterior cingulate cortex. Mol Cells 2007, 23: 259–271.
Zhuo M. Cortical excitation and chronic pain. Trends Neurosci 2008, 31: 199–207.
Ren LY, Lu ZM, Liu MG, Yu YQ, Li Z, Shang GW, et al. Distinct roles of the anterior cingulate cortex in spinal and supraspinal bee venom-induced pain behaviors. Neuroscience 2008, 153: 268–278.
Gong KR, Cao FL, He Y, Gao CY, Wang DD, Li H, et al. Enhanced excitatory and reduced inhibitory synaptic transmission contribute to persistent pain-induced neuronal hyper-responsiveness in anterior cingulate cortex. Neuroscience 2010, 171: 1314–1325.
Liu MG, Chen J. Preclinical research on pain comorbidity with affective disorders and cognitive deficits: Challenges and perspectives. Prog Neurobiol 2014, 116: 13–32.
Lu YF, Wang Y, He Y, Zhang FK, He T, Wang RR, et al. Spatial and temporal plasticity of synaptic organization in anterior cingulate cortex following peripheral inflammatory pain: multi-electrode array recordings in rats. Neurosci Bull 2014, 30: 1–20.
Wang GQ, Cen C, Li C, Cao S, Wang N, Zhou Z, et al. Deactivation of excitatory neurons in the prelimbic cortex via Cdk5 promotes pain sensation and anxiety. Nat Commun 2015, 6: 7660.
Zhang Z, Gadotti VM, Chen L, Souza IA, Stemkowski PL, Zamponi GW. Role of prelimbic GABAergic circuits in sensory and emotional aspects of neuropathic pain. Cell Rep 2015, 12: 752–759.
Li Z, Lu YF, Li CL, Wang Y, Sun W, He T, et al. Social interaction with a cagemate in pain facilitates subsequent spinal nociception via activation of the medial prefrontal cortex in rats. Pain 2014, 155: 1253–1261.
Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci 2013, 14: 502–511.
Kumar S, Porcu P, Werner DF, Matthews DB, Diaz-Granados JL, Helfand RS, et al. The role of GABA(A) receptors in the acute and chronic effects of ethanol: a decade of progress. Psychopharmacology (Berl) 2009, 205: 529–564.
Pohorecky LA, Shah P. Ethanol-induced analgesia. Life Sci 1987, 41: 1289–1295.
Stewart SH, Finn PR, Pihl RO. A dose-response study of the effects of alcohol on the perceptions of pain and discomfort due to electric shock in men at high familial-genetic risk for alcoholism. Psychopharmacology (Berl) 1995, 119: 261–267.
Gatch MB. Effects of benzodiazepines on acute and chronic ethanol-induced nociception in rats. Alcohol Clin Exp Res 1999, 23: 1736–1743.
Gatch MB, Lal H. Effects of ethanol and ethanol withdrawal on nociception in rats. Alcohol Clin Exp Res 1999, 23: 328–333.
Tatsuo MA, Yokoro CM, Salgado JV, Pesquero SM, Santana MA, Francischi JN. Hyperalgesic effect induced by barbiturates, midazolam and ethanol: pharmacological evidence for GABA-A receptor involvement. Braz J Med Biol Res 1997, 30: 251–256.
Volkow ND, Mullani N, Gould L, Adler SS, Guynn RW, Overall JE, et al. Effects of acute alcohol intoxication on cerebral blood flow measured with PET. Psychiatry Res 1988, 24: 201–209.
Sano M, Wendt PE, Wirsen A, Stenberg G, Risberg J, Ingvar DH. Acute effects of alcohol on regional cerebral blood flow in man. J Stud Alcohol 1993, 54: 369–376.
Tolentino NJ, Wierenga CE, Hall S, Tapert SF, Paulus MP, Liu TT, et al. Alcohol effects on cerebral blood flow in subjects with low and high responses to alcohol. Alcohol Clin Exp Res 2011, 35: 1034–1040.
Leriche M, Mendez M, Zimmer L, Berod A. Acute ethanol induces Fos in GABAergic and non-GABAergic forebrain neurons: a double-labeling study in the medial prefrontal cortex and extended amygdala. Neuroscience 2008, 153: 259–267.
Segovia KN, Vontell R, Lopez-Cruz L, Salamone JD, Correa M. c-Fos immunoreactivity in prefrontal, basal ganglia and limbic areas of the rat brain after central and peripheral administration of ethanol and its metabolite acetaldehyde. Front Behav Neurosci 2013, 7: 48.
Faccidomo S, Bannai M, Miczek KA. Escalated aggression after alcohol drinking in male mice: dorsal raphe and prefrontal cortex serotonin and 5-HT(1B) receptors. Neuropsychopharmacology 2008, 33: 2888–2899.
Barbier E, Tapocik JD, Juergens N, Pitcairn C, Borich A, Schank JR, et al. DNA methylation in the medial prefrontal cortex regulates alcohol-induced behavior and plasticity. J Neurosci 2015, 35: 6153–6164.
Ding ZM, Ingraham CM, Rodd ZA, McBride WJ. The reinforcing effects of ethanol within the posterior ventral tegmental area depend on dopamine neurotransmission to forebrain cortico-limbic systems. Addict Biol 2015, 20: 458–468.
Hwa LS, Nathanson AJ, Shimamoto A, Tayeh JK, Wilens AR, Holly EN, et al. Aggression and increased glutamate in the mPFC during withdrawal from intermittent alcohol in outbred mice. Psychopharmacology (Berl) 2015, 232: 2889–2902.
Zimmermann M. Ethical guidelines for investigations of experimental pain in conscious animals. Pain 1983, 16: 109–110.
Gilmartin MR, Kwapis JL, Helmstetter FJ. Trace and contextual fear conditioning are impaired following unilateral microinjection of muscimol in the ventral hippocampus or amygdala, but not the medial prefrontal cortex. Neurobiol Learn Mem 2012, 97: 452–464.
Shaw CL, Watson GD, Hallock HL, Cline KM, Griffin AL. The role of the medial prefrontal cortex in the acquisition, retention, and reversal of a tactile visuospatial conditional discrimination task. Behav Brain Res 2013, 236: 94–101.
Okine BN, Rea K, Olango WM, Price J, Herdman S, Madasu MK, et al. A role for PPARalpha in the medial prefrontal cortex in formalin-evoked nociceptive responding in rats. Br J Pharmacol 2014, 171: 1462–1471.
Paxinos G Watson C. The Rat Brain in Stereotaxic Coordinates. Amsterdam: Elsevier Academic Press, 2005.
Tu Y, Kroener S, Abernathy K, Lapish C, Seamans J, Chandler LJ, et al. Ethanol inhibits persistent activity in prefrontal cortical neurons. J Neurosci 2007, 27: 4765–4775.
Jo YS, Lee J, Mizumori SJ. Effects of prefrontal cortical inactivation on neural activity in the ventral tegmental area. J Neurosci 2013, 33: 8159–8171.
Chen J, Luo C, Li H, Chen H. Primary hyperalgesia to mechanical and heat stimuli following subcutaneous bee venom injection into the plantar surface of hindpaw in the conscious rat: a comparative study with the formalin test. Pain 1999, 83: 67–76.
Yang F, Fu H, Lu YF, Wang XL, Yang Y, Yang F, et al. Post-stroke pain hypersensitivity induced by experimental thalamic hemorrhage in rats is region-specific and demonstrates limited efficacy of gabapentin. Neurosci Bull 2014, 30: 887–902.
McDonald AJ, Mascagni F. Neuronal localization of m1 muscarinic receptor immunoreactivity in the rat basolateral amygdala. Brain Struct Funct 2010, 215: 37–48.
Jiang ZC, Pan Q, Zheng C, Deng XF, Wang JY, Luo F. Inactivation of the prelimbic rather than infralimbic cortex impairs acquisition and expression of formalin-induced conditioned place avoidance. Neurosci Lett 2014, 569:89–93.
Niv D, Whitwam JG, Loh L. Depression of nociceptive sympathetic reflexes by the intrathecal administration of midazolam. Br J Anaesth 1983, 55: 541–547.
Jurna I. Depression of nociceptive sensory activity in the rat spinal cord due to the intrathecal administration of drugs: effect of diazepam. Neurosurgery 1984, 15: 917–920.
Tatsuo MA, Salgado JV, Yokoro CM, Duarte ID, Francischi JN. Midazolam-induced hyperalgesia in rats: modulation via GABA(A) receptors at supraspinal level. Eur J Pharmacol 1999, 370: 9–15.
Yokoro CM, Pesquero SM, Turchetti-Maia RM, Francischi JN, Tatsuo MA. Acute phenobarbital administration induces hyperalgesia: pharmacological evidence for the involvement of supraspinal GABA-A receptors. Braz J Med Biol Res 2001, 34: 397–405.
Ossipov MH, Dussor GO, Porreca F. Central modulation of pain. J Clin Invest 2010, 120: 3779–3787.
Ji G, Neugebauer V. Pain-related deactivation of medial prefrontal cortical neurons involves mGluR1 and GABA(A) receptors. J Neurophysiol 2011, 106: 2642–2652.
Ji G, Neugebauer V. CB1 augments mGluR5 function in medial prefrontal cortical neurons to inhibit amygdala hyperactivity in an arthritis pain model. Eur J Neurosci 2014, 39: 455–466.
Jurik A, Auffenberg E, Klein S, Deussing JM, Schmid RM, Wotjak CT, et al. Roles of prefrontal cortex and paraventricular thalamus in affective and mechanical components of visceral nociception. Pain 2015, 156: 2479–2491.
Lee M, Manders TR, Eberle SE, Su C, D’Amour J, Yang R, et al. Activation of corticostriatal circuitry relieves chronic neuropathic pain. J Neurosci 2015, 35: 5247–5259.
Kiritoshi T, Ji G, Neugebauer V. Rescue of impaired mGluR5-driven endocannabinoid signaling restores prefrontal cortical output to inhibit pain in arthritic rats. J Neurosci 2016, 36: 837–850.
Kang SJ, Kwak C, Lee J, Sim SE, Shim J, Choi T, et al. Bidirectional modulation of hyperalgesia via the specific control of excitatory and inhibitory neuronal activity in the ACC. Mol Brain 2015, 8: 81.
Singer T, Seymour B, O’Doherty J, Kaube H, Dolan RJ, Frith CD. Empathy for pain involves the affective but not sensory components of pain. Science 2004, 303: 1157–1162.
Shamay-Tsoory SG, Aharon-Peretz J, Perry D. Two systems for empathy: a double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesions. Brain 2009, 132: 617–627.
Shamay-Tsoory SG. The neural bases for empathy. Neuroscientist 2011, 17: 18–24.
Bernhardt BC, Singer T. The neural basis of empathy. Annu Rev Neurosci 2012, 35: 1–23.
Decety J, Norman GJ, Berntson GG, Cacioppo JT. A neurobehavioral evolutionary perspective on the mechanisms underlying empathy. Prog Neurobiol 2012, 98: 38–48.
Goubert L, Craig KD, Vervoort T, Morley S, Sullivan MJ, de CWAC, et al. Facing others in pain: the effects of empathy. Pain 2005, 118: 285–288.
Langford DJ, Crager SE, Shehzad Z, Smith SB, Sotocinal SG, Levenstadt JS, et al. Social modulation of pain as evidence for empathy in mice. Science 2006, 312: 1967–1970.
Loggia ML, Mogil JS, Bushnell MC. Empathy hurts: compassion for another increases both sensory and affective components of pain perception. Pain 2008, 136: 168–176.
Godinho F, Faillenot I, Perchet C, Frot M, Magnin M, Garcia-Larrea L. How the pain of others enhances our pain: searching the cerebral correlates of ‘compassional hyperalgesia’. Eur J Pain 2012, 16: 748–759.
Mogil JS. Social modulation of and by pain in humans and rodents. Pain 2015, 156 Suppl 1: S35–41.
Steele CM, Critchlow B, Liu TJ. Alcohol and social behavior II: the helpful drunkard. J Pers Soc Psychol 1985, 48: 35–46.
Varlinskaya EI, Spear LP. Acute effects of ethanol on social behavior of adolescent and adult rats: role of familiarity of the test situation. Alcohol Clin Exp Res 2002, 26: 1502–1511.
Varlinskaya EI, Spear LP. Increases in anxiety-like behavior induced by acute stress are reversed by ethanol in adolescent but not adult rats. Pharmacol Biochem Behav 2012, 100: 440–450.
Trezza V, Baarendse PJ, Vanderschuren LJ. Prosocial effects of nicotine and ethanol in adolescent rats through partially dissociable neurobehavioral mechanisms. Neuropsychopharmacology 2009, 34: 2560–2573.
Sayette MA, Creswell KG, Dimoff JD, Fairbairn CE, Cohn JF, Heckman BW, et al. Alcohol and group formation: a multimodal investigation of the effects of alcohol on emotion and social bonding. Psychol Sci 2012, 23: 869–878.
Fairbairn CE, Sayette MA. A social-attributional analysis of alcohol response. Psychol Bull 2014, 140: 1361–1382.
Fairbairn CE, Sayette MA. Frigessi A. Alcohol and emotional contagion: an examination of the spreading of smiles in male and female drinking groups. Clin Psychol Sci 2015, 3: 686–701.
Van Kerkhof LW, Damsteegt R, Trezza V, Voorn P, Vanderschuren LJ. Social play behavior in adolescent rats is mediated by functional activity in medial prefrontal cortex and striatum. Neuropsychopharmacology 2013, 38: 1899–1909.
Acknowledgments
This work was supported by grants from the National Basic Research Development Program of China (2013CB835103) and the National Natural Science Foundation of China (81571072 and 31600855).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Kai-Wen Geng, Ting He and Rui-Rui Wang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Geng, KW., He, T., Wang, RR. et al. Ethanol Increases Mechanical Pain Sensitivity in Rats via Activation of GABAA Receptors in Medial Prefrontal Cortex. Neurosci. Bull. 32, 433–444 (2016). https://doi.org/10.1007/s12264-016-0063-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12264-016-0063-4