Abstract
This study aimed to assess the safety, effectiveness, and comfort of operating surgeon in conducting laparoscopic cholecystectomy (LC) under spinal anaesthesia (SA) in comparison to general anaesthesia (GA). LC were conducted in 101 patients which were randomly divided via lottery method in two groups, GA (n = 50) and SA (n = 51). Operative time, surgeon’s comfort, intraoperative and postoperative pain, and adverse events were compared between the groups. Two patients from GA and one from SA were removed from the study due to intraoperative complication. Mean anaesthesia time was significantly lower (p = 0.011) in the SA group (48.37 ± 10.91) as compared to the GA group (55.60 ± 16.22). Intraoperative anxiety was found in only one patient in the SA group (2% vs. 0%) who received midazolam 2 mg. Intraoperative right shoulder pain was significantly more (p < 0.001) in the SA group (50% vs. 0%) which was treated by Fentanyl 50 μg in IV boluses. Intraoperative nausea was more in the SA group (4% vs. 0%) but not significantly different. Mean VAS (visual analogue scale) was significantly lower in SA as compared to GA at 0, 3, and 6 hr (p = 0.003, <0.001, and <0.001). Mean VAS for right shoulder tip pain was significantly higher in SA as compared to GA at 0 and 3 hr (p = 0.009 and 0.045). Surgeon’s comfort was higher for GA (100% vs. 94%) but not significantly different. LC under SA is feasible, safe, and with less postoperative pain and mean anaesthesia time; however, surgeon’s comfort was more in the GA group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cholecystectomy is a common treatment in gastrointestinal surgery, and the laparoscopic method has established itself as the gold standard for symptomatic cholelithiasis as well as chronic and acute cholecystitis. This procedure results in less postoperative pain, better cosmesis, and shorter hospital stay and disability from work than open cholecystectomy [1, 2]. However, the overall serious complication rate in laparoscopic cholecystectomy (LC) remains higher than that seen in open cholecystectomy [3, 4]. LC is conventionally done under general anaesthesia (GA). Initially, the indications for spinal anaesthesia (SA) were reported for cases in which GA is difficult, but now, it is a routine procedure for otherwise healthy patients also [5, 6]. SA has the advantage of providing analgesia and total muscle relaxation in a conscious and compliant patient and an uneventful postoperative recovery. At the same time, it also protects against the potential complications of GA [7].
Recent studies have illustrated that LC can be safely performed under SA with low pressure CO2 pneumoperitoneum [8]. The findings of these studies revealed that SA demonstrates less postoperative pain in comparison to GA [9, 10]. Though, frequent postoperative complaints of abdominal discomfort and shoulder pain were reported on using SA [11]. Therefore, this study is designed as a prospective randomized controlled trial to assess whether SA, instead of GA can be used as a routine procedure in clinical practice. The present study also aims to investigate the safety of procedure, postoperative complaints, and comfort of the operating surgeon in conducting LC under SA. The review of related literature revealed that some work has been done on laparoscopic cholecystectomy with various variables. However, none of the previously done studies have included surgeon comfort scale and other parameters which we have monitored in a single study. Hence, I have decided to conduct the present study.
Patients and Methodology
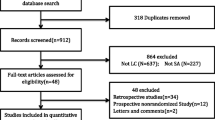
The study was conducted in Department of General Surgery of PG Teaching Tertiary Centre LHDM and Dr Prem Hospital, Panipat. We did Prospective, Single centred, Randomized Control Trial (CTRI Acknowledgement Number: REF/2020/10/037453) for a duration of 18 months. Study included all patients with age 20–65 years having cholelithiasis and fit for surgery according to PAC. Exclusion criteria were ASA group IV, V, and VI patients/patients having acute cholecystitis/cholangitis/acute pancreatitis/bleeding diathesis/local spinal deformity/COPD/pregnancy. All patients were informed about the study, and written informed consent was obtained. Random sampling of patients was done by using the lottery method by putting 51 chits of SA and 50 chits of GA in a bowl (Fig. 1). The patients were divided into two groups by pulling out one chit at a time. Group A underwent conventional four port LC under GA, and Group B underwent the same procedure by using SA. For both groups, the surgery was performed by the same consultant surgeon and anaesthesiologist.
During anaesthetic management, each patient had received midazolam 1 mg IV, Pantoprazole 40 mg IV, and Ondansetrone 4 mg IV as standard pre-anaesthetic medication. In the GA Group A, anaesthesia was induced in supine position with 2.0 mg/kg of Propofol, 0.1 mg/kg of Vecuronium, and Fentanyl 2 μg/kg. After intubation, patient was placed in reverse trendelenburg position for surgery. Maintenance of anaesthesia was done with O2, N2O, and Isoflurane. EtCO2 maintained between 35 and 45 mmHg. Post-surgery neuromuscular blockade was reversed with 50 μg/kg of Neostigmine and 10 mcg/kg of Glycopyrrolate. In the SA Group B, subarachnoid space was puncture with 25-gauge spinal needle between the L3–L4 spine intervertebral space in sitting or left lateral decubitus position and 2.5–3.5 ml of hyperbaric 0.5% Bupivacaine was injected. Afterwards, patient was placed in the supine position with a head-down position. After confirming the anaesthesia at T4 level by pin prick, “go-ahead” was given. During the procedure, anxiety and right shoulder tip pain were treated with 2 mg Midazolam, Fentanyl 50 μg in IV boluses, and 50 mg Inj Propofol. Intraoperative monitoring of parameters like: Anaesthesia time: In Group A, it was the time taken from induction to extubation. For Group B, it is time taken from spinal puncture to final dressing of patient. Pneumoperitoneum time: This was defined as time from CO2 insufflation through Veress needle till expulsion of all CO2 at end of the procedure. Surgery time: This was defined as time from first incision to final suture in both the groups. Intraoperative significant events were defined as anxiety, right shoulder tip pain, and vomiting. During post-operative period abdominal pain/discomfort, right shoulder tip pain was evaluated by using VAS at 0, 3, 6, 12, and 24 hr after the surgery. Additionally, nausea and vomiting were graded [12]. The comfort of the surgeon during surgery was recorded by using a Surgeon Comfort Scale (SCS) which was developed and standardized by the investigator.
Results
-
a)
Comparison of Intraoperative Factors: The mean anaesthesia time was noted to be 55.60 ± 16.22 in the GA group and 48.37 ± 10.91 in the SA group. The mean anaesthesia time was significantly lower (p = 0.011) in the SA group as compared to the GA group. Similarly, Tiwari et al. [10] demonstrated that the duration of anaesthesia (min) was significantly more in the GA group (49.45 ± 6.73) as compared to the SA group (40.64 ± 5.5 0.02). The mean pneumoperitoneum time was 30.02 ± 15.08 in the GA group and 29.16 ± 8.97 in the SA group which was not significantly different (p = 0.734). The mean surgery time was not significantly different (p = 0.745) in between the GA group (36.46 ± 14.79) and the SA group (35.56 ± 11.92). In this study, anxiety was found in only one patient (2%) in SA received Midazolam 2 mg, whereas no anxiety was found in the GA group. The Hamilton Anxiety Rating Scale (HAM-A) score was 9 in one patient in group B only. Moreover, the incidence of intraoperative anxiety was not significantly different (p = 0.325) in between groups. The intraoperative right shoulder pain was significantly more (p < 0.001) in the SA group (50%) as compared to the GA group (0.0%). Moreover, the right shoulder tip pain was treated by Fentanyl 50 μg in IV boluses. Moderate pain (mean 5.08 ± 0.86 VAS score) was present in 50% patients in group B. So, not a single patient was converted from the SA to GA groups. The percentage of nausea was 0.0% in the GA group (group A) and 4.0% in the SA group (group B). Moreover, the nausea was more in the SA group as compared to the GA group but not significantly different (p = 0.493). The grade II type of nausea was found in these two patients of the SA group. The vomiting was not found in any patients in both groups.
-
b)
Comparison of Post-operative Factors: The mean VAS for post-operative abdominal pain/discomfort was significantly lower in the SA group as compared to the GA group at 0 hr, 3 hr, and 6 hr (p = 0.003, <0.001 and <0.001), whereas it was not significantly different in between groups at 12 hr and 24 hr (p = 0.497 and 0.969) (Table 1).
Table 1 Comparisons of post-operative mean VAS
The nausea and vomiting were not significantly different in between groups at 0 hr, 3 hr, 6 hr, 12 hr, and 24 hr (p = 0.872, 0.819, 0.635, 0.778, and 0.809) (Table 2). The mean VAS for right shoulder tip pain was significantly higher in the SA group as compared to the GA group at 0 hr and 3 hr (p = 0.009 and 0.045) but not significantly different in between groups at 6 hr, 12 hr, and 24 hr (p = 0.350, 0.423, and 0.608) (Table 2).
-
c)
Details of Comfort of the Surgeon in Groups: The total comfort score of the scale varies from 0 to 20 showing “not difficult” to “highly difficult” level of surgery. The higher score reflected high level of difficulty and vice-versa.
In our study, the significant diaphragmatic movement with respiration and right shoulder pain during operation were significantly more (p = 0.003 and <0.001) in the SA group as compared to the GA group (Table 3), whereas the rest of the parameters of SCS were comparable between groups.
Table 4 illustrates that the Surgeon comfort was higher in group A as compared to group B but not significantly different (p=0.256).
Discussion
-
a)
Comparison of Intraoperative Factors: The mean anaesthesia time was significantly lower in the spinal anaesthesia group as compared to the general anaesthesia group. Similarly, Tiwari et al. [10] demonstrated that the duration of anaesthesia (min) was significantly more in the GA group (49.45 ± 6.73) as compared to the SA group (40.64 ± 5.5 0.02). The intraoperative right shoulder pain was significantly more in the spinal anaesthesia group (50%) as compared to the general anaesthesia group (0.0%). Moreover, the right shoulder tip pain was treated by Fentanyl 50 μg in IV boluses. Yuksek et al. [5] demonstrated that the incidence of intraoperative right-shoulder pain is 50%; it was severe enough to necessitate anaesthetic conversion in three patients (10.3%) and in five patients (17.2%); additional spraying of the diaphragm with 2% Lidocaine solution was required for control of the pain. The nausea was more in the spinal anaesthesia group as compared to the general anaesthesia group but not significantly different. The vomiting was not found in any patients in both groups. Imbelloni et al. [13] reported that only one patient had nausea and vomiting in the SA group, whereas it was not observed in the GA group.
-
b)
Comparison of Post-operative Factors: The post-operative pain mean VAS was significantly lower in the SA group as compared to the GA group at 0 hr, 3 hr, and 6 hr, whereas it was not significantly different in between groups at 12 hr and 24 hr (Table 1). Similarly, Imbelloni et al. [13] show that the pain evaluated by the VAS was significantly less severe in the spinal anaesthesia group at 2, 4, and 6 hr. Bessa et al. [7] observed that the mean pain scores were significantly lower at 2 and 4 hr postoperatively in the SA group. The mean pain scores were not significantly different at 6, 10, and 24 hr postoperatively between groups. The postoperative nausea and vomiting were not significantly different in between groups at 0 hr, 3 hr, 6 hr, 12 hr, and 24 hr (Table 2). Previous various studies observed that the use of spinal anaesthesia has been associated with a statistically significant lower incidence of PONV [7, 11]. The mean VAS for right shoulder tip pain was significantly higher in the spinal anaesthesia group as compared to the general anaesthesia group (Table 2). Imbelloni et al. [13] reported that in the immediate post-operative period, eight out of 33 patients in the general anaesthesia group and two out of 34 patients in the spinal anaesthesia group developed pain in the right shoulder.
-
c)
Comfort of the Surgeon: We found that the surgeon comfort was higher for general anaesthesia groups (100%) compared to spinal anaesthesia group (94%) (Table 4). Previously Ellakany [14] reported that the surgeon satisfaction score was significantly lower in the GA group (4.1) as compared to the SA group (3). A study reported that there was no statistically significant difference between both groups studied regarding the degree of patient satisfaction with the anaesthetic technique they received.
Conclusion
The present study was carried out to determine the safety, effectiveness, and the comfort of operating surgeon in conducting LC under SA in comparison to GA. LC performed under SA is feasible, safe, and with less postoperative pain and less mean anaesthesia time. Due to higher right shoulder pain, nervousness, and diaphragm moment in spinal group, surgeon satisfaction was more in the GA group. From the study, it was observed that LC under GA is much more beneficial for patients who have anxiety. We also recorded that the patients and surgeons were more comfortable under GA. However, for the patients who are at greater risk due to smoking/COPD, the safest and most effective method will be performing LC under SA. The recovery of patients was not significantly different in between the groups. Although, more studies are needed to support the results.
Abbreviations
- SA:
-
spinal anaesthesia
- GA:
-
general anaesthesia
- LC:
-
laparoscopic cholecystectomy
- ASA grade:
-
American Society of Anaesthesiologists
- RR:
-
respiratory rate
- SD:
-
standard deviation
- Kg:
-
kilogram
- Hrs:
-
hours
- mins:
-
minutes
- VAS :
-
visual analogue scale
- PONV:
-
postoperative nausea and vomiting
- PR:
-
pulse rate
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- CO2:
-
carbon dioxide
- EtCO2:
-
end-tidal carbon dioxide
- PACU:
-
post-anaesthesia care unit
- SCS:
-
surgeon comfort scale
- HAM-A:
-
Hamilton Anxiety Rating Scale
- COPD:
-
chronic obstructive pulmonary disease
- PAC:
-
pre-anaesthetic checkup
References
Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW (1992) Laparoscopic cholecystectomy. The new 'gold standard'? Arch Surg 127:917
Yamashita Y, Takada T, Kawarada Y et al (2007) Surgical treatment of patients with acute cholecystitis: Tokyo guidelines. J Hepato-Biliary-Pancreat Surg 14:91
Vollmer CM Jr, Callery MP (2007) Biliary injury following laparoscopic cholecystectomy: why still a problem? Gastroenterology 133:1039
Khan MH, Howard TJ, Fogel EL et al (2007) Frequency of biliary complications after laparoscopic cholecystectomy detected by ERCP: experience at a large tertiary referral center. Gastrointest Endosc 65:247
Yuksek YN, Akat AZ, Gozalan U, Daglar G, Pala Y, Canturk M, Tutuncu T, Kama NA (2008) Laparoscopic cholecystectomy under spinal anaesthesia. Am J Surg 195:533–536
Yu G, Wen Q, Qiu L et al (2015) Laparoscopic cholecystectomy under spinal anaesthesia vs. general anaesthesia: a meta-analysis of randomized controlled trials. BMC Anesthesiol 15:176
Bessa SS, El-Sayes IA, El-Saiedi MK, Abdel-Baki NA, Abdel-Maksoud MM (2010) Laparoscopic cholecystectomy under spinal versus general anaesthesia: a prospective, randomized study. J Laparoendosc Adv Surg Tech 20:515–520
Hajong R, Khariong PD, Baruah AJ, Anand M, Khongwar D (2014) Laparoscopic cholecystectomy under epidural anaesthesia: a feasibility study. N Am J Med Sci 6:566–569
Das W, Bhattacharya S, Ghosh S, Saha S, Mallik S, Pal S (2015) Comparison between general anaesthesia and spinal anaesthesia in attenuation of stress response in laparoscopic cholecystectomy: a randomized prospective trial. Saudi J Anaesth 9:184–188
Tiwari S, Chauhan A, Chaterjee P, Alam MT (2013) Laparoscopic cholecystectomy under spinal anaesthesia: a prospective, randomised study. J Minim Access Surg 9:65–71
Tzovaras G, Fafoulakis F, Pratsas K, Georgopoulou S, Stamatiou G, Hatzitheofilou C (2008) Spinal vs general anaesthesia for laparoscopic cholecystectomy: interim analysis of a controlled randomized trial. Arch Surg 143:497–501
Wiesen SM, Unger SW, Barkin JS et al (1993) Laparoscopic cholecystectomy: the procedure of choice for acute cholecystitis. Am J Gastroenterol 88:334
Imbelloni LE, Fornasari M, Fialho JC, Sant'Anna R, Cordeiro JA (2010) General anaesthesia versus spinal anaesthesia for laparoscopic cholecystectomy. Rev Bras Anestesiol 60(3):217–227
Ellakany M (2013) Comparative study between general and thoracic spinal anaesthesia for laparoscopic cholecystectomy. Egypt J Anaesth 29:375–381
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Verma, R.K., Kumar, A., Gupta, S. et al. Randomised Controlled Clinical Trial of Spinal and General Anaesthesia in Laparoscopic Cholecystectomy. Indian J Surg (2023). https://doi.org/10.1007/s12262-023-03970-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-023-03970-2