Abstract
Biliary cystadenomas (BCA) are a group of rare cystic tumors of the biliary ductal system, accounting for less than 5% of the non-parasitic cysts of the liver. Though benign, malignant transformation is as high as 20%. We present two case series of biliary cystadenomas — serous and mucinous. Both patients underwent enucleation of the cysts with good recovery and no recurrence in follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biliary cystadenomas (BCA) are a group of rare cystic tumors of the biliary ductal system, accounting for less than 5% of the non-parasitic cysts of the liver [1,2,3,4]. Majority (90%) are found in middle-aged women [2, 3]. Mostly benign, they do carry a risk of malignant transformation (up to 20%) and the preoperative differentiation between the two is often difficult [2, 4]. BCA has two variants — serous type (common) and mucinous type [1]. Origin of these neoplasms is either from an aberrant bile duct or from primitive hepatobiliary stem cells and 85% are intrahepatic [2, 5]. Intrahepatic lesions may present as an incidental finding or with abdominal pain and fullness. Extrahepatic BCA can manifest with obstructive jaundice and cholangitis [5]. The mucinous variety are further divided into two subgroups: those with mesenchymal tissue resembling ovarian stroma (OS) on histology and those that do not — non-ovarian stroma (non-OS). While the OS variant is much more common and seen exclusively in women, the non-OS variant is equally distributed between men and women and is associated with an overall poorer prognosis and higher rate of recurrence.
Patient 1
A policewoman, 38 years of age, known hypertensive, had presented to us with complaints of dragging pain in the right hypochondrium of 1-month duration. She had no history of fever, vomiting, or yellowish discoloration of eyes or skin. On examination, patient had tenderness in the right hypochondrium. Routine blood investigations were within normal limits. Ultrasound abdomen showed a cyst in the left lobe of the liver with multiple septations which aroused suspicions of biliary cystadenoma. A contrast-enhanced CT done showed a thick-walled multiloculated peripherally enhancing fluid density adjacent and anterior to gall bladder fossa measuring 5.9 × 5.8 × 5.3 cm; no evidence of intrahepatic biliary radicle communication was noted. Magnetic resonance cholangiopancreatography (MRCP) showed the lesion to be located at the confluence of gall bladder, common hepatic, and portal vein. The patient underwent enucleation surgery and cholecystectomy on 17 May 2019. Histopathology revealed a cystic multiloculated swelling with mucinous fluid within a thick fibrocollagenous wall suggestive of mucinous biliary cystadenoma and adjacent inflammatory infiltrates as sequelae of chronic cholecystitis. No recurrence was noted in 1-year follow-up (Fig. 1a–f).
Patient 1: a intrapost operative picture of the enucleated specimen of the cystadenoma measuring roughly 7.5 × 4.5 × 5 cm; b porto venous phase of CECT abdomen and pelvis showing hyperdense lesion; c axial cut of T2-weighted MRCP showing hypointense lesion in the liver parenchyma; d hyperintense lesion at the confluence of the CBD, cystic duct and hepatic ducts; with no established intrahepatic biliary communication; and e and f microscopic images in high power
Patient 2
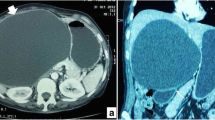
An elderly lady (74 years), home maker, had presented to us with a history of fullness in upper abdomen and nausea for 2 months. Clinical examination revealed a palpable mass in the epigastrium extending to the right hypochondrium measuring 10 × 7 cm, firm in consistency. Investigations showed a normal hemogram, liver function, and renal function tests. Ultrasound of the abdomen revealed a large biloccular 10 × 6.5-cm cystic lesion with debris and calcification in the left lobe of liver displacing stomach inferiorly. CECT abdomen showed well-defined cystic lesion measuring 10 × 7 cm in left lobe with exophytic component. The lesion was seen indenting the lesser curvature of stomach and pancreas with maintained fat planes. She underwent laparotomy and enucleation of the liver cyst. Histopathology showed a cyst wall-lined by cuboidal epithelium and wall composed of fibrocollagenous tissue consistent with serous type of cystadenoma. No recurrence was noted in 7-month follow-up (Fig. 2).
Discussion
Non-parasitic cystic neoplasms of liver are found in 5–10% of the population, simple cysts being the commonest and other being biliary cystic tumors, i.e., biliary cystadenomas and cystadenocarcinoma [3]. BCA was first reported by Hueter; resection was reported by Keen 5 years later [2, 3]. Origin of these neoplasms is either from an aberrant bile duct or from primitive hepatobiliary stem cells. These tumors contain internal septations and intraluminal papillary projections, lined by mucus secreting cuboidal or columnar biliary epithelium, surrounded in layers by dense mesenchymal stroma of smooth muscle cells followed by a loose layer of collagen having blood vessels, nerves, and bile ducts [2]. The cyst fluid varies from being clear to bile stained, purulent, or proteinaceous. A blood-stained fluid is suggestive of a cystedenocarcinoma [2].
The clinical features of these tumors depend on whether it is intrahepatic or extrahepatic in nature. Intrahepatic lesions may present as an incidental finding or with abdominal pain and fullness. Extrahepatic BCA can manifest with obstructive jaundice and cholangitis [5]. Ascites due to compression on inferior vena cava or the hepatic veins may also occur [3]. BCA is found to increase in size during pregnancy suggesting hormonal dependence [5]. MRI, US, and CT demonstrate intrahepatic cystic lesions with features such as mural nodules, varying wall thickness, papillary projections, and internal septations [5].
The differential diagnosis in a patient with cystic lesions in the liver includes BCA, hydatid cyst, post-traumatic cyst, liver abscess, polycystic disease, hemorrhagic cyst, embryonal sarcoma, primary or metastatic necrotic neoplasm, atypical simple cyst, and biliary intraductal papillary mucinous neoplasm (IPMN) [4]. Due to a documented high recurrence rate of 80–90% in procedures like aspiration, internal drainage, or marsupialization [3, 4], a better recommended procedure will be a formal resection of the tumor with negative surgical margins. Other procedures like liver resection or enucleation may be done depending on patient characteristics and anatomic location [3,4,5].
References
Averbukh LD, Wu DC, Cho WC, Wu GY (2019) Biliary mucinous cystadenoma: a review of the literature. J Clin Transl Hepatol 7(2):149–153. https://doi.org/10.14218/JCTH.2019.00017
Sugi RV, Sugumar C, Senthil Kumar P, Prabhakaran R, Jeswanth S, Ravichandran P (2018) Extrahepatic intraductal biliary cystadenomas: solving the mystery of “idiopathic biliary obstruction”? A tertiary care institute experience. Int J Hepatobiliary Pancreat Dis 8:100078Z04SS2018
Pillai SA, Velayutham V, Perumal S, Perumal SU, Lakshmanan A, Ramaswami S, Ramasamy R, Sathyanesan J, Palaniappan R, Rajagopal R (2012) Clinical study biliary cystadenomas: a case for complete resection. HPB Surgery 2012(501705):6. https://doi.org/10.1155/2012/501705
Soares KC, Arnaoutakis DJ, Kamel I et al (2014) Cystic neoplasms of the liver: biliary cystadenoma and cystadenocarcinoma. J Am Coll Surg 218(1):119–128. https://doi.org/10.1016/j.jamcollsurg.2013.08.014
Morris MW, Anderson CD, Drake LC, Redfield SM, Subramony C (2012) WB Vanderlan 2012 Giant biliary cystadenoma. J Surg Case Rep 9:15. https://doi.org/10.1093/jscr/2012.9.15
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
Consent was taken from the patients for the same.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Affiliation at time of study: Fr Muller Medical College, Mangalore
Rights and permissions
About this article
Cite this article
Dsouza, C., Diaz, E., Nambiar, S. et al. Biliary Cystadenoma — Our Experience. Indian J Surg 84 (Suppl 2), 551–553 (2022). https://doi.org/10.1007/s12262-022-03490-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03490-5