Abstract
Complicated liver hydatid cysts are rare in pregnant women. Its management may have many particularities. The aim of our study was to describe clinical, morphological features, and therapeutic modalities of complicated hydatid cysts in pregnant women. We conducted a case series analysis and a monocentric study, including patients who presented a complicated hydatid cyst during pregnancy, admitted in our surgical department, over a period of 11 years. A total of 8 patients were included. Mean age was 26.1 SD 4 years. Mean term was 16.7 SD 5 weeks. All patients had abdominal pain; one patient had fever; and no patient was icteric. Hyperleukocytosis was present in 2 patients; C-reactive protein was elevated in 2 patients; and liver function tests were disturbed in 3 patients. In abdominal ultrasound, hydatid cyst was located in the right liver in 5 cases and in the left liver in 3 cases. Average size of cysts was 7.6 SD 2.1 cm. All the patients underwent surgery. The approach was a right subcostal incision in 6 cases and a midline incision in 2 cases. “Lagrot” procedure was performed in 7 cases and bipolar drainage in one case. Postoperative course was simple in 6 cases. One patient presented a miscarriage at 10 weeks. Another patient presented an abdominal wall abscess. Complicated hydatid cysts in pregnant women have a noiseless clinical presentation. Abdominal ultrasound is the morphological examination of choice. Conservative treatment is preferred. Fetal prognosis is better if operation is performed during the second trimester.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The occurrence of liver echinococcosis is rare during pregnancy. Its incidence varies from 1/30000 to 1/20000 [1]. Complicated liver hydatid cysts in pregnant women can pose diagnostic and therapeutic difficulties. During pregnancy, the risk of rupture of liver hydatid cyst into bile ducts or peritoneal cavity is increased by more rapid cyst growth [2]. Clinical presentation is variable, ranging from simple pain in right hypochondrium to acute cholangitis, anaphylactic or septic shock. Medical imaging is used to make the diagnosis of complicated hydatid cyst, in combination with other clinical and biological findings [3]. The aim of our study was to describe clinical and morphological features of complicated hydatid cysts in pregnant women, as well as management modalities.
Patients and Methods
It was a case series analysis and monocentric study conducted in a surgery department, over a period of 11 years, from 2009 to 2020. All the patients who presented a hydatid cyst complicated by infection, opening in peritoneum or in bile ducts during pregnancy were included, regardless of their age or pregnancy’s term. The patients with per operatory diagnosis of uncomplicated hydatid cyst were excluded. Clinical, paraclinical, and operative data were extracted from patients’ medical records and operative reports. Data entry and analysis were performed using Statistical Package for Social Sciences (SPSS) version 23.0 software.
The study was approved by the hospital’s local ethics committee.
Results
A total of 8 patients were included in the study. The mean age of the patients was 26.1 SD 4 years with extremes ranging from 22 to 33 years. Clinical, biological, and imaging findings are summarized in Table 1.
Patients’ management was both medical and surgical. Conservative surgical methods were employed. Therapeutic management for each patient is presented in Table 2.
Discussion
Clinical expression of complicated hydatid cysts is variable with multiple possible clinical signs [4]. Different symptoms may be associated, resulting in a variety of more or less suggestive clinical pictures. Abdominal pain is the most frequent clinical sign. Its location varies: mainly not only the right hypochondrium but also the epigastrium and sometimes the whole abdomen. This sign has been found in 7 to 92.5% of cases depending on the series [4]. Rarely, fever is the first sign of ductal infection. It was present in 45.5% of cases in a series of 90 patients [5]. It may be an acute cholangitis, with peaks of up to 40 °C, reflecting bacterial discharge into the bloodstream from bile ducts. These feverish peaks may be accompanied by chills, palpitations, and sometimes a change in general condition [3]. Jaundice usually occurs after pain and fever. It may be a conjunctival sub icterus or a frank mucocutaneous jaundice. It most often indicates obstruction of the main biliary duct. Initially; the passage of hydatid fluid leads to pain and fever. The picture is completed by jaundice when, secondarily, there is a migration of hydatid material. The diagnosis of the opening is therefore easy to make in the presence of jaundice in a patient with a hydatid cyst of the liver [6]. Other signs may be found such as hepatomegaly or an abdominal mass [7]. In our series, all the patients presented abdominal pain; two out of eight patients had a palpable mass in the right hypochondrium; only one patient had fever and no patient was icteric.
Biological examinations are not specific in the diagnosis of complicated hydatid cysts in pregnant women, but their objectives are to reinforce the diagnosis of biliary involvement by looking for cholestasis and an infectious syndrome, to study the general repercussions of this condition, to evaluate the patient’s operability and monitor the evolution of the disease after treatment. In 64 patients, the authors found hyperleukocytosis in 33.2% of the cases [8]. In another study, a disturbance of the liver balance was noted in 28.2% of the cases [9]. In our series, hyperleukocytosis was present in 2 out of 8 patients; CRP was elevated in 2 patients; and liver function tests were disturbed in 3 patients.
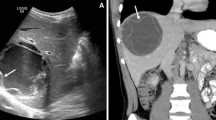
Abdominal ultrasound can confirm the diagnosis in most situations. It can be performed regardless of the term of pregnancy. It is the only examination performed preoperatively in more than 90% of the cases [10]. It allows cyst visualization and precise their number, type, size, topography, and relationship with biliary and vascular elements [11]. This examination has been shown to be reliable for the diagnosis of liver hydatid cyst in over 90% of the cases in most series [12]. Topographical diagnosis of cyst is easy with ultrasound when cyst size does not exceed 20-cm long axis [12]. The appearance of hydatids is variable and is due to changes in intracystic pressure, activity of proligeral membrane, and pericyst remodeling [13]. These aspects have been the subject of about twenty classifications, of which Gharbi’s classification is the only one used in our country, and comprises 5 types corresponding to successive stages of natural evolution of the parasite [12]. The rupture of hydatid cyst in the bile ducts is reflected on ultrasound by a collapsed appearance of cystic contents, by dilatation of intra- and/or extra-hepatic bile ducts, by the presence of hydatid material in the bile ducts and by the existence of a cysto-biliary communication. A complete picture, including all these ultrasound signs, is found in only 25% of the cases. Thus, the diagnosis of a rupture in the bile ducts of the liver’s hydatid cyst is often suspected when it is associated with dilatation of the bile ducts in a clinico-biological context of acute cholangitis [12]. None of the patients in our series had biliary dilatation at the time of diagnosis. Abdominal CT can only be indicated in pregnant women beyond the third trimester. Ultrasound alone or in combination with other investigations allows the diagnosis of the liver’s hydatid cyst in about 96% of the cases [11]. CT remains limited in its indications, especially for remanifested liver’s hydatid cysts in pseudo-tumoral form, univesicular hydatid cysts, hydatid cysts where ultrasound does not allow a topographical diagnosis, especially when they exceed 15 cm in diameter and developed essentially outside the liver, and when there is a suspicion of complications of hydatid cysts that are inaccessible to ultrasound, such as cyst-digestive and cyst-bronchial fistulas [14]. MRI can be performed in pregnant women beyond the first semester. In addition, it is more effective than CT in detecting complications, in particular cyst rupture in the bile ducts (Fig. 1) [15].
Obstetrical examination is used to detect signs of threatened preterm birth and to check fetal vitality in order to adapt the procedure. This examination should look for gyneco-obstetric pathologies that may explain the symptomatology [16]. Fetal heart rate recording is a simple and rapid examination that allows assessment of fetal well-being and also allows detection of uterine contractions [16]. Obstetric ultrasound is an important part of obstetric assessment. It is used to search for obstetric anomalies that may explain the clinical symptomatology on one hand and to assess the fetal well-being on the other. Endovaginal ultrasound can measure the length of the cervix and assess the risk of preterm birth [16].
Treatment with albendazole alone has no place in complicated hydatid cysts of the liver, especially as it is not recommended in the first trimester of pregnancy due to its teratogenic and embryotoxic effects [3]. During pregnancy, the risk of liver’s hydatid cyst rupture is increased by the more rapid growth of cyst, which should prompt intervention before delivery [3]. The second trimester is considered the best time to operate on a pregnant woman because of the lower risk of miscarriage (0 compared with 12% in first trimester) and premature delivery (5 to 8% compared with 30% in the third trimester) [17]. In our series, 6 out of 8 patients were operated on in the second trimester; one patient operated on in the first trimester presented a miscarriage postoperatively. Surgical treatment remains the treatment of choice for these complications. It must be done by a classic surgery, most often a right sub-costal incision. In the case of a hydatid cyst open in the biliary tract, per operative cholangiography can be performed with protection of the fetus by a leaded gown. The choice of procedure depends on the characteristics of the cyst and the fistula. Trans-fistulo-odial internal drainage or trans-parieto-hepatic disconnection according to Perdromo are the two methods of choice [18]. In our series, a “Lagrot” procedure was performed in 6 cases, associated with an epiploplasty in one case. Bipolar drainage with closure of cystobiliary fistula was performed in one case.
Tocolysis, lung maturation with corticosteroids, and transfer to a suitable maternity unit should be discussed according to gestational age [19]. Some authors stated that no study has demonstrated the benefit of prophylactic tocolysis and that its use remains a matter of choice [19]. A pre- or postoperative course of corticosteroids can be offered if preterm delivery is threatened before 34 weeks of gestation. This treatment accelerates lung maturation [16].
Conclusion
According to our study’s results, complicated hydatid cysts in pregnant women may have a noiseless clinical presentation, dominated by abdominal pain. Abdominal ultrasound is the morphological examination of choice in pregnant women. Conservative treatment is preferred. The fetal prognosis is better if operation is performed during the second trimester of pregnancy. However, because of the limited number of population in our study, these data need to be further evaluated by other powerful clinical trials.
Data Availability
The data and supportive information is available within the article.
References
Ghosh JK, Goyal SK, Behera MK, Dixit VK, Jain AK (2014) Hydatid cyst of liver presented as obstructive jaundice in pregnancy; managed by Pair. J Clin Exp Hepatol 4(4):366–9. https://doi.org/10.1016/j.jceh.2014.11.002
Can D, Oztekin O, Oztekin O, Tinar S, Sanci M (2003) Hepatic and splenic hydatid cyst during pregnancy: a case report. Arch Gynecol Obstet 268(3):239–40. https://doi.org/10.1007/s00404-002-0348-x
Van Vliet W, Scheele F, Sibinga-Mulder L, Dekker GA (1995) Echinococcosis of the liver during pregnancy. Int J Gynaecol Obstet 49(3):323–4. https://doi.org/10.1016/0020-7292(95)02360-o
Blairon L, Derbel F, Hamida R, Delmée M (2000) Le kyste hydatique du foie Approche clinique et thérapeutique À propos de 97 cas opérés dans un CHU de Tunisie centrale. Med Mal Infec 30:641–9. https://doi.org/10.1016/S0399-077X(00)80035-9
Kourias B, Mantonakis S (1968) Hydatid cysts of the liver rupturing into the bile ducts. Current therapeutic measures. Analysis of 90 operated cases. J Chir Paris 96(1):21–36 (PMID: 5704077)
Ufuk F, Duran M (2018) Intrabiliary rupture of hepatic hydatid cyst leading to biliary obstruction, cholangitis, and septicemia. J Emerg Med 54(1):e15-7. https://doi.org/10.1016/j.jemermed.2017.09.009
Collado-Aliaga J, Romero-Alegría Á, Alonso-Sardón M, Prieto-Vicente V, López-Bernus A, Velasco-Tirado V et al (2021) Portal hypertension as a complication of cystic echinococcosis: a 20-year cohort analysis. Am J Trop Med Hyg 105(3):692–7. https://doi.org/10.4269/ajtmh.21-0274
Daali M, Fakir Y, Hssaida R, Hajji A, Hda A (2001) Hydatid cysts of the liver opening in the biliary tract. Report of 64 cases. Ann Chir 126(3):242–5. https://doi.org/10.1016/s0003-3944(01)00507-7
Lygidakis NJ (1983) Diagnosis and treatment of intrabiliary rupture of hydatid cyst of the liver. Arch Surg 118(10):1186–9. https://doi.org/10.1001/archsurg.1983.01390100056014
Gharbi HA, Ben Chehida F, Moussa N, Bellagha I, Ben Amor N, Hammou A et al (1995) Hydatid cyst of the liver. Gastroenterol Clin Biol 19(5 Pt 2):B110-118 (PMID: 8522090)
Gharbi H, Mnif J, Abdallah M, Abdelmoula B, Hammou-Jeddi A (1986) Epidémiologie du kyste hydatique en Tunisie. I: Résultats de l’enquête par échographie abdominale portant sur 3116 sujets dans la région de Menzel Bourguiba. Med Mal Infec 16(3):151–156. https://doi.org/10.1016/S0399-077X(86)80218-9
Gharbi HA, Hassine W, Brauner MW, Dupuch K (1981) Ultrasound examination of the hydatic liver. Radiology 139(2):459–63. https://doi.org/10.1148/radiology.139.2.7220891
Beyrouti MI, Beyrouti R, Abbes I, Kharrat M, Amar MB, Frikha F et al (2004) Acute rupture of hydatid cysts in the peritoneum: 17 cases. Presse Med 33(6):378–84. https://doi.org/10.1016/s0755-4982(04)98600-9
Grosdidier J Boissel P Nesseler J Delfosse J Grosdidier D (1984) Traitement du kyste hydatique du foie. A propos de 62 cas. In: Annales médicales de Nancy et de l’Est 445–52.
Klotz F Nicolas X Debonne JM Garcia JF Andreu JM (2000) Kystes hydatiques du foie. Encycl Méd Chir 7–023-A-10:16.
Ducarme G, Bonne S, Khater C, Ceccaldi P-F, Poujade O, Luton D (2012) Acute non-obstetrical diseases during pregnancy and role of the obstetrician. Presse Med 41(2):125–33. https://doi.org/10.1016/j.lpm.2011.04.003
Curet MJ, Allen D, Josloff RK, Pitcher DE, Curet LB, Miscall BG et al (1996) Laparoscopy during pregnancy. Arch Surg 131(5):546–551. https://doi.org/10.1001/archsurg.1996.01430170092017
Trigui A, Rejab H, Krichene J, Tlili A, Trabelsi J, Kachoua A et al (2021) Surgical treatment of hydatid cysts with large biliocystic fistula in conservative strategy. Pan Afr Med J 38:195. https://doi.org/10.11604/pamj.2021.38.195.27098
Hée P, Viktrup L (1999) The diagnosis of appendicitis during pregnancy and maternal and fetal outcome after appendectomy. Int J Gynaecol Obstet 65(2):129–35. https://doi.org/10.1016/s0020-7292(99)00013-2
Author information
Authors and Affiliations
Contributions
All the authors participated in the design of the study and wrote the manuscript. All the authors read and approved the final manuscript.
- Mahjoubi Mohamed Farès has drafted the work.
- Ben Dhaou Anis has substantively revised the work.
- Karoui Yasser, Rezgui Bochra, and Essid Nada have made substantial contributions to the literature research.
- Mounir Ben Moussa has made substantial contributions to the conception of the work.
Corresponding author
Ethics declarations
Ethics Approval
Our locally appointed ethics committee “Charles Nicolle Hospital local committee” has approved the research protocol.
Human and Animal Rights
Our study complies with the Declaration of Helsinki.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farès, M.M., Anis, B.D., Yasser, K. et al. Pregnancy and Large Liver Hydatid Cyst. Indian J Surg 85, 307–312 (2023). https://doi.org/10.1007/s12262-022-03421-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03421-4