Abstract
Post-traumatic spigelian hernia is a rare entity and requires a high index of suspicion for its detection. Mostly the cases are diagnosed at the time of first presentation when a swelling is seen at the site of injury. We report a case of missed post-traumatic abdominal wall hernia at the left spigelian point in a 3-year child missed during initial exploration for traumatic jejunal perforation which led to re-exploration for incarceration of hernia. The rarity of presentation as a post-operative complication has not been reported in literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blunt trauma abdomen contributes to a major proportion of pediatric trauma and is also a major cause of morbidity and mortality in children [1]. The mode and severity of impact determine the associated internal injury. Sudden increase in the intraabdominal pressure following blunt trauma can cause the disruption of musculature and fascia. This type of abdominal wall defect with intact overlying skin can lead to herniation of bowel loops through the defect [2]. This post-traumatic herniation at a site without any previous evidence of hernia is known as traumatic abdominal wall hernia (TAWH) [3]. Though rare, TAWH have been reported in children due to their weaker parietal wall and more elastic skin [2, 4]. To the best of our knowledge, we herein discuss the presentation, management, and lessons learnt from the first case in English literature of TAWH in a child missed during primary exploration.
Case Report
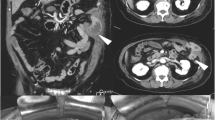
A 3-year boy presented with a history of blunt trauma abdomen, 4 h following a road traffic accident. On primary survey, the child was in shock with blood pressure of 60/30 mmHg and had a positive Focused Assessment with Sonography for Trauma (FAST) suggestive of hemoperitoneum. The child did not respond to two boluses of normal saline at a dose of 20 ml/kg given over 30 min and was classified as a non-responder. As the child was non-responder to fluid resuscitation with a positive FAST examination and the rest of the primary survey being normal, he was directly shifted from red area to the operating room for exploratory laparotomy. On exploration, there was a mesenteric tear with active bleed and a jejunal perforation of size around 4 cm extending toward the mesenteric border. Ligation of bleeder with resection of perforated segment followed by an end-to-end jejuno-jejunal anastomosis was performed. The child had an uneventful postoperative period and was orally allowed on the fifth post-operative day. The child tolerated feeds for 24 h but after that, he developed abdominal pain, distension, and vomiting with an ill-defined parietal wall swelling in the left paramedian region, 3–4 cm below the umbilicus(Fig. 1a). Ultrasonographic scan of the abdomen was unremarkable except that there was a trapped small bowel loop in between the abdominal wall layers (Fig. 1b). As there was no improvement, a relaparotomy was performed. The distal jejunal loops were found herniating through a defect in the parietal wall and pre-gangrenous changes were seen which were reversible on applying hot mop (Fig. 2a). The defect was repaired from the inside in layers and the abdomen was closed (Fig. 2b). The child had an uneventful postoperative period and was discharged on the sixth post-operative day.
Discussion
The first description of trauma-causing abdominal hernia was given by Selby [5]. The diagnostic criteria for TAWH include the immediate appearance of the hernia through the disrupted muscle and fascia after blunt abdominal trauma, and failure of the injury to penetrate the skin (Table 1) [6], but our case was unique as hernia developed in post-operative period. These types of hernia are associated with low-energy impact and the site of herniation is at one of the weakest portions of the spigelian fascia [7]. The spigelian fascia refers to the combined ventral aponeuroses of the transversus abdominis, internal oblique, and external oblique muscles. At the intersection of the semilunar line and the arcuate line, the fascia has its weakest point due to the lack of rectus sheath at this level [7]. In our case, the defect was at this site. Spontaneous spigelian hernia in pediatric age is rare and traumatic spigelian hernia is still rarer. Contrast enhanced computed tomography (CECT) scan of the abdomen is the investigation of choice for diagnosis of any defect in the parietal wall, but CECT is not possible in hemodynamically unstable requiring urgent exploration and the defect can be missed in such cases [6, 7]. Diagnostic laparoscopy is an excellent adjunct in the management of TAWHs [8].
Conclusion
Blunt abdominal trauma can lead to the development of an internal parietal wall defect but the herniation may not happen immediately. The abdominal wall should be routinely checked for internal defects during exploration to avoid devastating complications postoperative obstruction and strangulation.
References
Lynch T, Kilgar J, Al Shibli A (2018) Pediatric abdominal trauma. Curr Pediatr Rev 14(1):59–63. http://www.eurekaselect.com/154920/article
Al Beteddini OS, Abdulla S, Omari O (2016) Traumatic abdominal wall hernia: a case report and literature review. Int J Surg Case Rep 24:57–59. http://www.ncbi.nlm.nih.gov/pubmed/27180322
Hardcastle TC, Du Toit DF, Malherbe C, Coetzee GN, Hoogerboord M, Warren BL et al (2005) Traumatic abdominal wall hernia--four cases and a review of the literature. S Afr J Surg 43(2):41–43. http://www.ncbi.nlm.nih.gov/pubmed/16035382
Mancel B, Aslam A (2003) Traumatic abdominal wall hernia: an unusual bicycle handlebar injury. Pediatr Surg Int 19(11):746–747. https://doi.org/10.1007/s00383-003-1064-8
Selby CD (1906) Direct abdominal hernia of traumatic origin. JAMA 47:1485–1486
Wood RJ, Ney AL, Bubrick MP (1988) Traumatic abdominal hernia: a case report and review of the literature. Am Surg 54(11):648–651
Yee AM, Jazayeri SB, Mac O, Arabian S, Neeki M (2019) Management of traumatic Spigelian hernia: a case report and literature review. Cureus 11(11):e6213. http://www.ncbi.nlm.nih.gov/pubmed/31890414
Lopez R, King S, Maoate K, Beasley S (2011) Laparoscopic repair of paediatric traumatic Spigelian hernia avoids the need for mesh. ANZ J Surg 81(5):396–397. http://www.ncbi.nlm.nih.gov/pubmed/21518204
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Imran, M., Srivastava, V. & Pandey, V. Masquerades of a Traumatic Spigelian Hernia: Lessons Learnt. Indian J Surg (2021). https://doi.org/10.1007/s12262-021-02974-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-021-02974-0